© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Candida glabrata fungal ball cystitis is a rare
complication of conservative treatment of
placenta accreta: a case report
CK Wong, MB, ChB1; LY Cho, MB, BS, FHKAM (Obstetrics and Gynaecology)1; WL Lau, MB, BS, FHKAM (Obstetrics and Gynaecology)1; Ingrid YY Cheung, MB, ChB, FHKAM (Pathology)2; Chloe HT Yu, MB, BS3; IC Law, MB, BS, FHKAM (Surgery)3; WC Leung, MD, FHKAM (Obstetrics and Gynaecology)1
1 Department of Obstetrics and Gynaecology, Kwong Wah Hospital, Hong Kong
2 Department of Pathology, Kwong Wah Hospital, Hong Kong
3 Department of Surgery, Kwong Wah Hospital, Hong Kong
Corresponding author: Dr CK Wong (wongchunkitjack@hotmail.com)
Case report
In October 2019, a 42-year-old pregnant woman was
admitted to hospital at 35+2 weeks of gestation for
an elective caesarean section because of anterior
placenta praevia type I and suspected placenta
accreta. She was gravida 6 and parity 3+2. Her first
pregnancy in 1996 resulted in a normal vaginal
delivery. The second and third pregnancies were
surgically terminated in the first trimester. Fourth
and fifth pregnancies resulted in a lower segment
caesarean section in China due to oligohydramnios
and previous caesarean section.
The patient had an uneventful antenatal course
in the current pregnancy. Nonetheless ultrasound
examination at 35+2 weeks of gestation revealed an
anterior placenta praevia type I with the placenta’s
leading-edge 2.7 cm from the os. A diagnosis of
placenta accreta was made due to vascularities over
the subserosal surface of the lower segment.
A classical caesarean section was performed
after completing a course of antenatal corticosteroid
at 36+4 weeks of gestation. Around four-fifths of the
placenta separated spontaneously after 30 minutes.
The placenta was trimmed away and 3 × 3 cm of
anterior adherent placenta around the internal os
was left in place. Active bleeding from the lower
segment of the uterus and anterior placental bed
was controlled with Sengstaken–Blakemore balloon
tamponade (Rüsch Teleflex, Germany). Uterine
artery embolisation was performed at the same
operation by interventional radiologists. Total blood
loss for the operation was 500 mL.
After surgery, the patient was transferred
to the intensive care unit. Balloon tamponade was
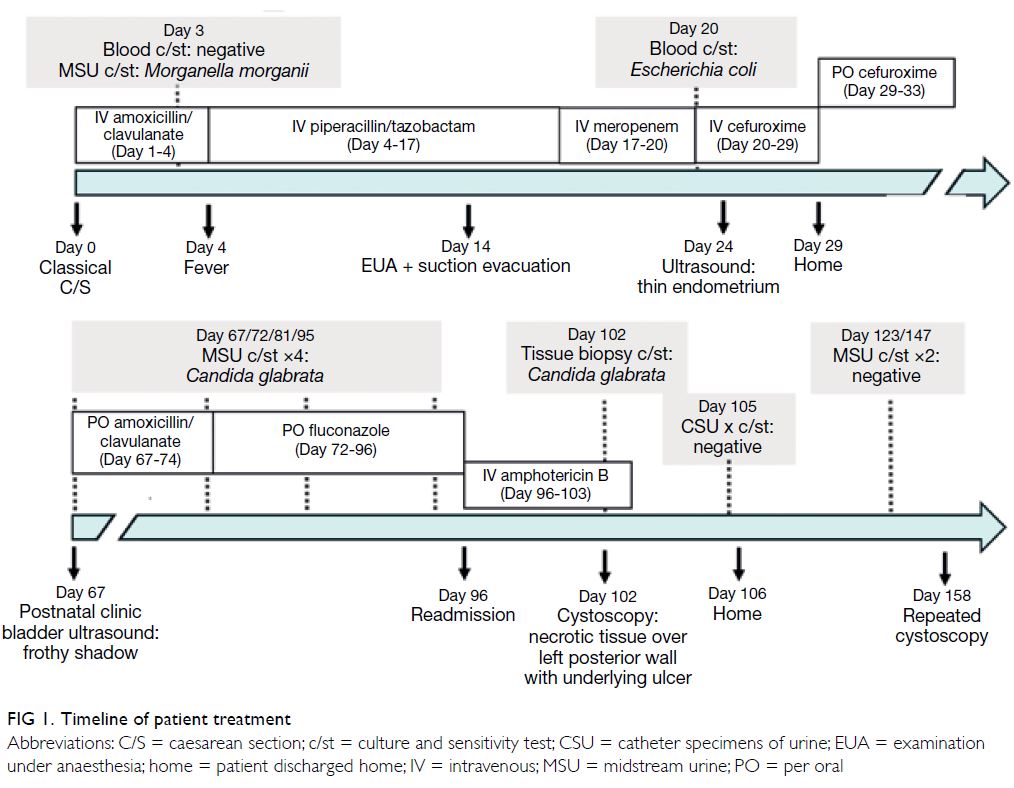
removed on day 1 (Fig 1). Prophylactic amoxicillin
and clavulanate was administered intravenously
after the operation. She complained of dysuria
and developed a persistent swinging fever from
day 2. Amoxicillin and clavulanate was switched
to piperacillin/tazobactam on day 4 after blood and urine tests for sepsis. Culture of midstream
urine showed Morganella morganii sensitive to
piperacillin/tazobactam and a gram-negative
bacillus. Microbiologists advised continuation of
piperacillin/tazobactam for 7 to 10 days.
Examination under anaesthesia and
ultrasound-guided suction evacuation were
performed on day 14 due to increased per-vaginal
bleeding. Intra-operatively, yellowish pus was seen
leaking from the cervical os and retained product of
gestation weighing 48 g was retrieved. Culture of the
pus grew Escherichia coli sensitive to piperacillin/tazobactam. The patient again presented with fever
postoperatively and blood culture revealed E coli
septicaemia. Piperacillin/tazobactam was switched
to meropenem on day 17. Blood culture sensitivity
testing revealed E coli sensitive to meropenem
and cefuroxime. Hence, meropenem was switched
to cefuroxime. Ultrasound examination on day
24 revealed no evidence of retained product of
gestation. Cefuroxime was continued for 14 days.
At 5-week follow-up examination, the
patient reported a 1-week history of whitish debris
in her urine, dysuria, and urinary frequency.
Ultrasonography revealed incomplete emptying of
the bladder with a lot of frothy shadows (Fig 2a).
Urinary tract infection was suspected so amoxicillin
and clavulanate and phenazopyridine were prescribed
for 1 week. Culture of the midstream urine showed
Candida glabrata (Fig 2b). A microbiologist was
consulted and fluconazole 400 mg prescribed for 10
days.
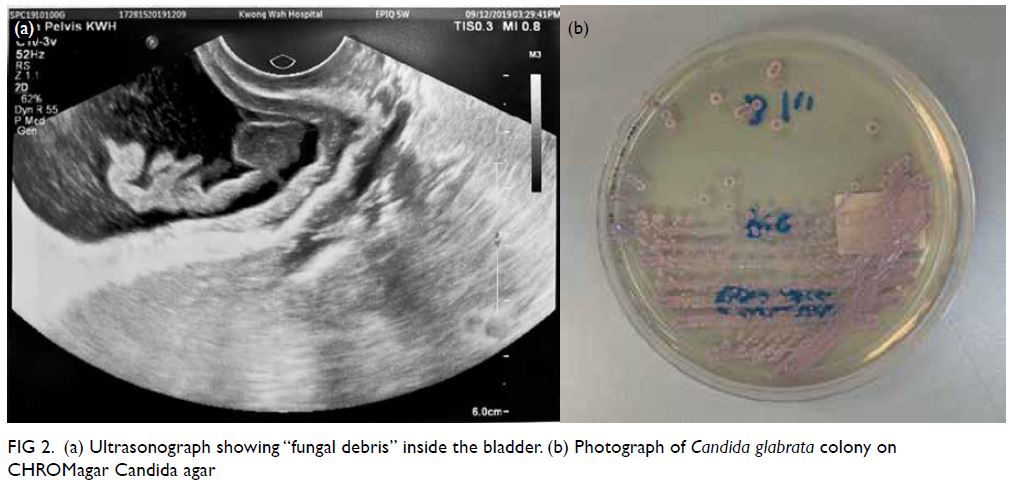
Figure 2. (a) Ultrasonograph showing “fungal debris” inside the bladder. (b) Photograph of Candida glabrata colony on CHROMagar Candida agar
Susceptibility testing of the C glabrata isolated from urine collected after admission was performed by using Sensititre YeastOne (TREK Diagnostic
Systems, United Kingdom) and revealed a required
fluconazole minimal inhibitory concentration of
16 μg/mL, confirming that it was in the susceptible-dose
dependent category. However, the patient’s
symptoms persisted after completing 24 days of fluconazole and ultrasound showed persistent
“fungal debris” inside the bladder. She was
readmitted 13 weeks after the operation for further
management. Amphotericin B deoxycholate was administered intravenously for 7 days. A drug-related
fever developed during the first dose but resolved
after premedication with oral acetaminophen and
intravenous diphenhydramine.
Flexible cystoscopy revealed necrotic tissue
approximately 3 × 4 cm over the left posterior
bladder wall, away from the left ureteric orifice, with
an underlying ulcer (Fig 3a and b). It was removed
with forceps and a basket. A fistula was suspected,
and second flexible cystoscopy scheduled 2 months
later. A computed tomography urogram with
contrast was arranged to exclude fistula.
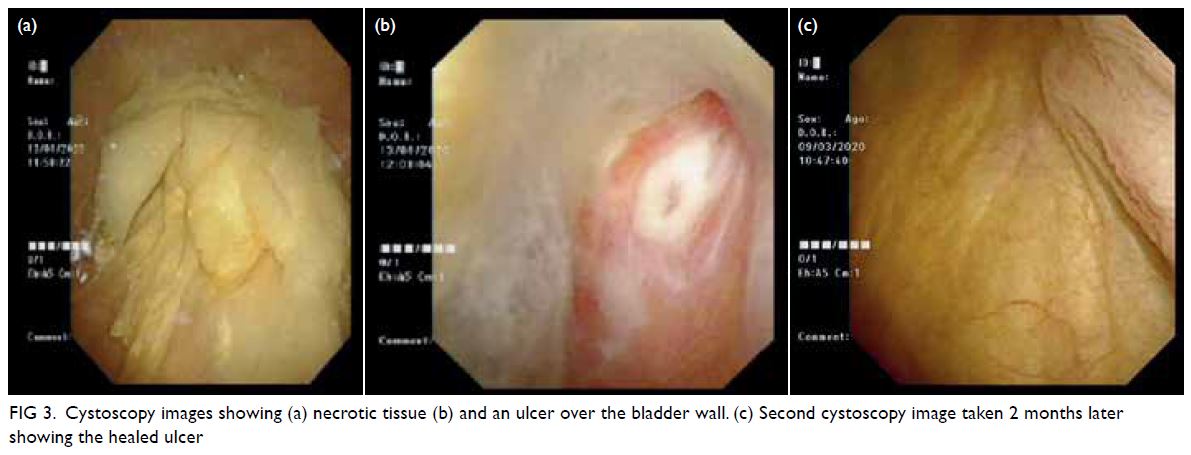
Figure 3. Cystoscopy images showing (a) necrotic tissue (b) and an ulcer over the bladder wall. (c) Second cystoscopy image taken 2 months later showing the healed ulcer
The second flexible cystoscopy revealed a
normal bladder and a healed ulcer over the left
posterior wall (Fig 3c). Computed tomography
urogram showed no evidence of fistula. During
postnatal follow-up, there were no urinary
symptoms.
Discussion
This is the first case of C glabrata cystitis as a complication in our case series of planned
conservative management of placenta accreta.1
Candida species are a part of the normal flora of the
gastrointestinal and vaginal tracts. The incidence of
candiduria has been increasing in recent decades
and the presence of C glabrata has become clinically
significant due to its high resistance to routine
antifungal agents. Risk factors for candiduria in our
case included urinary catheterisation, intensive care
unit stay, use of broad-spectrum antibiotics, female
sex, and prior surgery.2
The placental remnants in our case induced
infection and septicaemia. Subsequent prolonged
use of broad-spectrum antibiotics predisposed
our patient to fungal cystitis. There was no clinical
or pathological evidence of placenta percreta.
Chandraharan et al3 introduced the use of the
Triple-P procedure to manage patients with morbidly
adherent placenta. As the Triple-P procedure removes all intrauterine placental remnants, it may
reduce the risk of intrauterine infection and sepsis.
Nevertheless, there is limited surgical expertise in
this procedure in our unit.
Compared with other Candida species, many
C glabrata isolates are resistant to azoles due to
efflux pump–mediated resistance, genetic alterations
under stress and biofilm protection.4 A study in the
United States revealed that 14% of C glabrata isolates
were resistant to fluconazole.5
The presence of fungus ball/fungal bezoars in
urinary tract infection is extremely rare in adults.
According to treatment guidelines of the Infectious
Diseases Society of America, removal of the
obstructing mycelial mass by surgical or endoscopic
means is strongly recommended.6 Although culture
results revealed that the C glabrata was susceptible-dose-dependent to fluconazole, use of fluconazole
alone was likely to be insufficient due to the fungal
ball in the bladder. A multidisciplinary approach
including microbiologists and urologists is essential.
In symptomatic Candida cystitis, first-line
treatment is oral fluconazole 200 mg daily for 2 weeks.
For fluconazole-resistant C glabrata, amphotericin
B deoxycholate or oral flucytosine are the drugs
of choice. Around 50% of patients prescribed an
amphotericin B infusion experience infusion-related
adverse events, such as fever, chills, rigors,
hypotension, and rarely, hypokalaemia resulting in
ventricular fibrillation. In addition, renal toxicity is
a well-known adverse effect.5 Close monitoring of
renal function and electrolytes is essential.
Placenta accreta spectrum treated
conservatively by leaving the placenta in situ
is a recognised and successful management
option, but is associated with risks of infection or
postpartum haemorrhage. Our case demonstrates that fungal infection can develop during the period of conservative management and requires
multidisciplinary consultation.
Author contributions
Concept or design: CK Wong, WC Leung.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: CK Wong, WC Leung.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: CK Wong, WC Leung.
Critical revision of the manuscript for important intellectual content: All authors.
Conflicts of interest
The authors have no conflicts of interest to disclose.
Acknowledgement
The authors thank interventional radiologists Dr KH Lee and Dr CW Tang for their contributions to this report.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The patient was treated in accordance with the Declaration of Helsinki, provided informed consent for all treatments and procedures, and provided consent for publication.
References
1. Lo TK, Yung WK, Lau WL, Law B, Lau S, Leung WC. Planned conservative management of placenta accreta—experience of a regional general hospital. J Maternal Fetal Neonatal Med 2013;27:291-6. Crossref
2. Gajdács M, Dóczi I, Ábrók M, Lázár A, Burián K. Epidemiology of candiduria and Candida urinary tract
infections in inpatients and outpatients: results from
a 10-year retrospective survey. Cent European J Urol
2019;72:209-14.
3. Chandraharan E, Rao S, Belli A, Arulkumaran S. The
Triple-P procedure as a conservative surgical alternative
to peripartum hysterectomy for placenta percreta. Int J
Gynecol Obstet 2012;117:191-4. Crossref
4. Rodrigues CF, Silva S, Henriques M. Candida glabrata: a
review of its features and resistance. Eur J Clin Microbiol
Infect Dis 2013;33:673-88. Crossref
5. Pfaller MA, Messer SA, Hollis RJ, et al. Variation in
susceptibility of bloodstream isolates of Candida glabrata
to fluconazole according to patient age and geographic
location in the United States in 2001 to 2007. J Clin
Microbiol 2009;47:3185-90. Crossref
6. Pappas PG, Kauffman CA, Andes DR, et al. Executive
Summary: Clinical Practice Guideline for the Management
of Candidiasis: 2016 Update by the Infectious Diseases
Society of America. Clin Infect Dis 2016;62:409-17. Crossref