© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Managing limitations of the LMA Classic laryngeal mask as a conduit for tracheal intubation in impending paediatric airway obstruction: a case report
Gareth CH Cheng, MB, ChB; Jaclyn WM Wong, FHKCA, FHKAM (Anaesthesiology)
Department of Anaesthesia and Operating Theatre Services, Kwong Wah Hospital, Hong Kong
Corresponding author: Dr Gareth CH Cheng (gareth@fellow.hkam.hk)
Case report
Peritonsillar abscess (quinsy) is the most common
deep neck infection in children and adolescents,
although it is less frequently seen in young children.1
Airway compromise is a feared complication. We
describe the successful management of a patient with
impending paediatric airway obstruction. The LMA
Classic™ laryngeal mask (Teleflex Medical Ltd., Co.
Westmeath, Ireland) was the only paediatric-sized
supraglottic device available in our operating theatre
and was modified to work around its limitations as a
conduit for tracheal intubation.
In March 2020, an 18-month-old girl with
good past health weighing 9.5 kg was admitted to our
district general hospital 8 days after onset of fever up to 38.9°C, with worsening left facial swelling,
inspiratory stridor during sleep, drooling and poor
feeding.
On examination, she was pink and calm
when carried upright. Her throat was swollen
with bilateral grade 3 tonsils and the left cheek
and submandibular region were grossly swollen
(~10 cm × 6 cm). Contrast computed tomography
of the neck revealed a 3.3-cm × 4.8-cm × 3.8-cm
peritonsillar abscess with rightward deviation of
the upper airway and significant narrowing at the
larynx, with the narrowest cross-section measuring
3.5 mm (Fig 1).
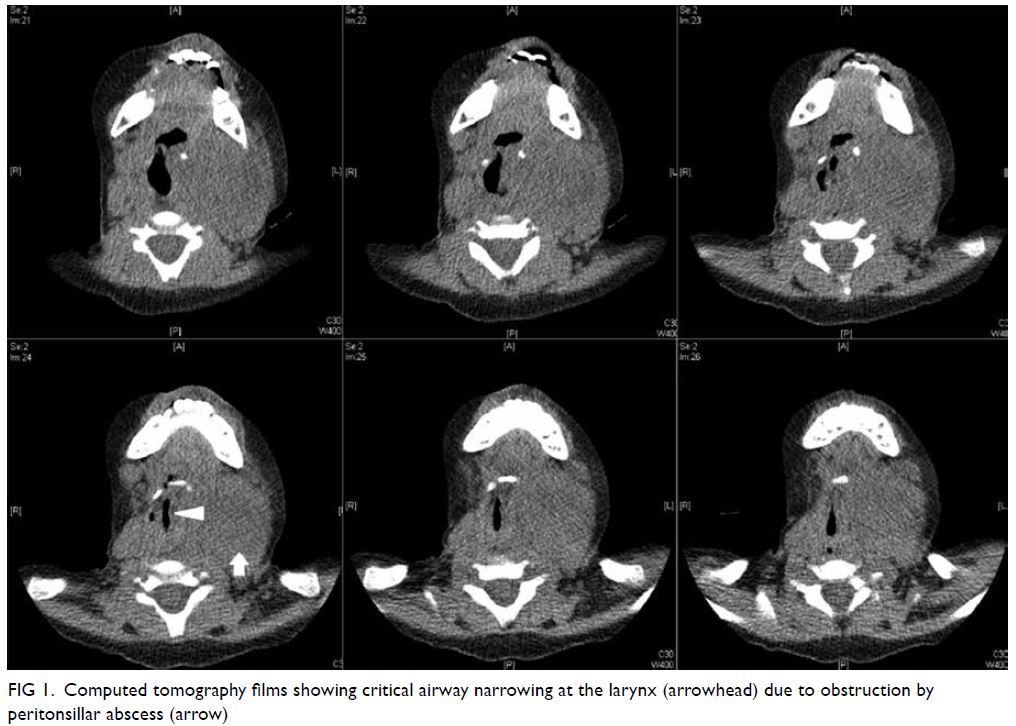
Figure 1. Computed tomography films showing critical airway narrowing at the larynx (arrowhead) due to obstruction by peritonsillar abscess (arrow)
In view of the critical airway diameter and
the impending progression to complete airway obstruction, and after discussion with the on-call
head and neck surgeons and the patient’s mother,
the decision was made to proceed with emergency
incision and drainage under general anaesthesia.
The sizing of all our airway equipment was
checked in advance. The distal aperture bars of a #1.5
LMA Classic laryngeal mask were cut to facilitate
use as an intubation conduit.
The patient had a 24G intravenous cannula
in situ on arrival in theatre. Surgeons were ready at
the bedside with front-of-neck access equipment on
standby. Hong Kong College of Anaesthesiologists
standard monitoring was applied. Gaseous induction
with spontaneous ventilation was performed using
an Ayres’ T-piece and 4% sevoflurane in 100%
oxygen. After an adequate depth of anaesthesia
was achieved as assessed by vital parameters,
intubation using video laryngoscopy was attempted.
Two initial attempts were unsuccessful, with very
rapid desaturation down to an SpO2 of 50% to 60%.
Subsequent attempts at rescue bag mask ventilation
failed despite optimisation by positioning and
oropharyngeal airway. Fortunately, a final attempt
to insert the laryngeal mask was successful and
ventilation was maintained.
As a definitive airway was still necessary,
a 2.2-mm fibreoptic bronchoscope was passed
through the laryngeal mask and a 3.5-mm Microcuff
endotracheal tube (ETT) carefully railroaded
over the bronchoscope into the trachea. Correct
positioning was confirmed by bilateral chest
auscultation and capnography. We deemed it unsafe
to leave the laryngeal mask in place as traction could
risk ETT dislodgement postoperatively. The video
laryngoscope was used to visualise the distal end
of the ETT near the vocal cords and it was secured
with Magill forceps. The laryngeal mask was slowly
pulled out over the ETT, but the 15-mm connector
of the laryngeal mask could not be passed over the
ETT pilot balloon even when deflated. Hence, we
carefully cut down the laryngeal mask with scissors,
leaving only the end with the 15-mm connector still
attached (Fig 2).

Figure 2. Endotracheal tube cuff ‘stuck’ on 15-mm connector (arrow); remnants of cut down LMA Classic laryngeal mask with scissor incision line seen (arrowhead)
The operation proceeded uneventfully.
Subsequently the patient was transferred to the
paediatric intensive care unit and kept intubated
and sedated. She was discharged after a short
hospital stay, with good recovery on clinic follow-up
examination.
Discussion
Paediatric airway emergencies are rare and among
the most challenging crises faced by anaesthetists.
Unique paediatric considerations such as inability
to cooperate during preoxygenation, intolerance to
awake techniques and difficult front-of-neck access,
in addition to inherent differences in paediatric
physiology, significantly reduce the safe apnoeic time and greatly increase the risk of hypoxia.
Ideally, this case would have been managed in
a specialist tertiary centre with a wider selection of
equipment and expertise; unfortunately, our requests
for night-time case transfer were denied. The
availability and use of an intubating laryngeal mask
with a larger-sized inner channel such as an air-Q™
(Salter Labs, Lake Forest [IL], United States) would
have been preferable to an LMA Classic. This would
have made it easier for us to remove the laryngeal
mask over the ETT after intubation without having
to improvise with our limited equipment in an
already stressful situation. Although the Association
of Paediatric Anaesthetists guidelines2 recommend
leaving the laryngeal mask in place after intubation,
we deemed it necessary to remove it since continued
postoperative ventilation was anticipated.
Often, manufacturer-recommended ETT/laryngeal mask combinations take account only of
the ability to pass the ETT through the laryngeal
mask. They may not consider the ability to remove
the laryngeal mask over the ETT when the diameter
of the ETT pilot balloon cuff exceeds that of the
outer diameter of the ETT. This problem was
illustrated in an article by Kleine-Brueggeney et al3
who found that only the air-Q models of supraglottic
airways were able to be removed over the ETT with all manufacturer-recommended size combinations,
as the air-Q had the largest inner channel diameter
among other equivalently sized supraglottic airways.
Alternatively, we could have chosen to cut
off the pilot balloon and repair the cuff with an
angiocatheter.4 Another option might have been
to use an uncuffed tube, although it would not
have been ideal in our case due to the possibility
of postoperative blood or secretions tracking down
and contaminating the lower airway. Furthermore,
exchange of a poorly fitting uncuffed tube would
have been difficult and potentially dangerous in our
situation, as the airway could easily have been lost.
In conclusion, in addition to meticulous
airway planning, testing combinations of ETT and
laryngeal mask for both insertion and subsequent
removal is important to avoid complications during
airway management. Availability of an intubating
laryngeal mask such as an air-Q may be particularly
advantageous in such cases.
Author contributions
Concept or design: GCH Cheng.
Acquisition of data: GCH Cheng.
Analysis or interpretation of data: GCH Cheng.
Drafting of the manuscript: Both authors.
Critical revision of the manuscript for important intellectual content: GCH Cheng.
Acquisition of data: GCH Cheng.
Analysis or interpretation of data: GCH Cheng.
Drafting of the manuscript: Both authors.
Critical revision of the manuscript for important intellectual content: GCH Cheng.
Both authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
Both authors have disclosed no conflicts of interest.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This case report was published with the written consent of the patient’s mother.
References
1. Ungkanont K, Yellon RF, Weissman JL, Casselbrant ML, González-Valdepeña H, Bluestone CD. Head and neck
space infections in infants and children. Otolarngol Head
Neck Sur 1995;112:375-82. Crossref
2. Association of Paediatric Anaesthetists. Unanticipated
difficult tracheal intubation during routine induction of
anaesthesia in a child aged 1 to 8 years. Available from:
https://www.das.uk.com/files/APA2-UnantDiffTracInt-FINAL.pdf. Accessed 21 Jan 2021.
3. Kleine-Brueggeney M, Kotarlic M, Theiler L, Greif R.
Limitations of pediatric supraglottic airway devices as
conduits for intubation—an in vitro study. Can J Anaesth
2018;65:14-22. Crossref
4. Kovatsis PG, Fiadjoe JE, Stricker PA. Simple, reliable replacement of pilot balloons for a variety of clinical situations. Paediatric Anaesth 2010;20:490-4. Crossref

