Hong Kong Med J 2021 Dec;27(6):458–60 | Epub 12 Nov 2021
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
COMMENTARY
Celebrating 60 years of corneal transplant in
Hong Kong
KW Kam, FRCS (Glasg), MSc Epidemiology (London)1,2; Victoria WY Wong, FRCSEd, FRCOphth2,3,4; Vanissa WS Chow, FRCSEd, FCOphthHK5; Evan PF Yiu, FRCS (Glasg), FHKAM (Ophthalmology)6; Alvin L Young, MMedSc (Hons), FRCOphth1,2
1 Department of Ophthalmology and Visual Sciences, Prince of Wales Hospital, Hong Kong
2 Department of Ophthalmology and Visual Sciences, The Chinese University of Hong Kong, Hong Kong
3 HKU Health System, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong
4 Department of Ophthalmology, Queen Mary Hospital and Grantham Hospital, Hong Kong
5 Department of Ophthalmology and Visual Sciences, Hong Kong Eye Hospital, Hong Kong
6 Tuen Mun Eye Centre, Hong Kong
Corresponding author: Prof Alvin L Young (youngla@ha.org.hk)
Visual restoration through transplantation was
limited to animal experiments until the first
successful human corneal transplant more than a
century ago in the Czech Republic area.1 Nowadays,
corneal transplant/keratoplasty is one of the most
commonly performed transplantation globally.
However, 4.2 million people still have corneal
blindness making it the fourth leading cause
of blindness according to the World Health
Organization, and graft scarcity remains a challenge.2
In Hong Kong, the first corneal transplant was
performed in 1961 at Tung Wah Eastern Hospital.
The expatriate surgeons performed many corneal
transplants using fresh corneas from American
eye banks (Fig a, b). This led to the establishment
of the Hong Kong Eye Bank (HKEB) and Research
Foundation in 1962.3
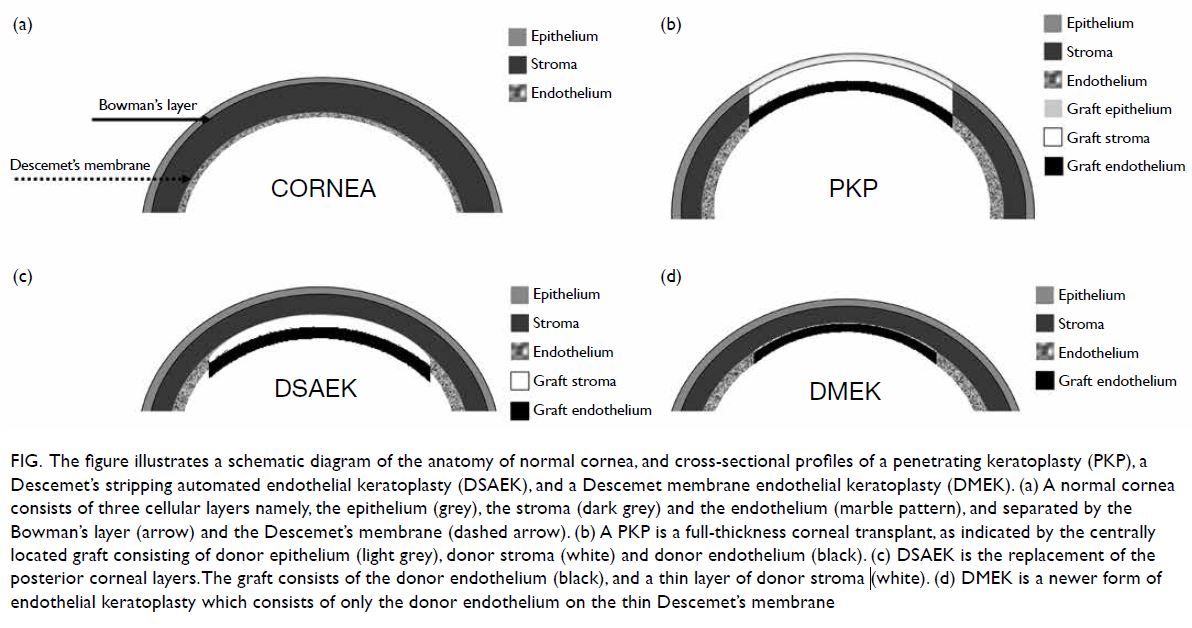
Figure. The figure illustrates a schematic diagram of the anatomy of normal cornea, and cross-sectional profiles of a penetrating keratoplasty (PKP), a Descemet’s stripping automated endothelial keratoplasty (DSAEK), and a Descemet membrane endothelial keratoplasty (DMEK). (a) A normal cornea consists of three cellular layers namely, the epithelium (grey), the stroma (dark grey) and the endothelium (marble pattern), and separated by the Bowman’s layer (arrow) and the Descemet’s membrane (dashed arrow). (b) A PKP is a full-thickness corneal transplant, as indicated by the centrally located graft consisting of donor epithelium (light grey), donor stroma (white) and donor endothelium (black). (c) DSAEK is the replacement of the posterior corneal layers. The graft consists of the donor endothelium (black), and a thin layer of donor stroma (white). (d) DMEK is a newer form of endothelial keratoplasty which consists of only the donor endothelium on the thin Descemet’s membrane
In the early years, the HKEB functioned mainly
as a distributing centre, because local donation was
rare. The concept of eye donation after death was
not widely accepted, because local eye surgeons
were sceptical regarding the success rate of corneal
transplant in the era before microscopic surgery,
and many local citizens subscribed to Confucian’s
ideology of ‘filial piety’, that is, a person’s body, hair,
and skin are gifts from their parents that should not
be damaged. As a result, the HKEB had to rely on
imported tissues from the International Eye Bank in
Sri Lanka. During the 1970s to 80s, between 20 and
40 corneas were flown to Hong Kong annually which
was insufficient to meet the local demand.
In the following decade there was a gradual
acceptance of organ donation after death, as solid
organ transplantation became available, society
became more Westernised, and levels of education
and public awareness were increased. Moreover, a
shortage of burial plots led to a shift to cremation,
weakening the concept of preserving a whole body
for the afterlife. In the 90s, even patients with
unilateral corneal blindness were keen to undergo surgery. To address soaring demand and the variable
quality of tissue from Sri Lanka, the HKEB started
harvesting corneas from local donors in 1992. The
quality of locally harvested cornea continued to
improve, and in 1997, importation from Sri Lanka
was stopped.
Since 2000, the Hospital Authority (HA) of
Hong Kong assumed responsibility for managing
organ supply, and the HKEB was renamed the HA
Lions Eye Bank. Management was later transferred
to the Hong Kong Eye Hospital from December 2009
and was again renamed the HA Eye Bank (HAEB)
from July 2016.
The HAEB has made great strides in
governance, quality, safety, personnel training, and
credentialing in meeting international standards.
Strategic partnerships with leading eye banks have
provided opportunities for progress. Since 2015,
HAEB has collaborated with Sight Life on quality
certification and entered into a global partnership
with Sight Life in 2017. This has strengthened
the HAEB in the regional eye banking scene. This
is reflected in the fact that >300 corneal buttons
have been harvested annually since 2017. As of
31 December 2020, 280 patients were on the waiting
list for a corneal transplant. The average waiting time
has now shortened to around 1 year. The youngest
donor was a 20-month-old infant and the oldest
cornea recipient was a centenarian. Unfortunately,
similar to other transplant activities, donation and
harvest rates have been adversely affected by the
coronavirus disease 2019 pandemic.
Graft scarcity remains the limiting factor
for the total number of keratoplasty procedures
performed each year. A global survey revealed
that 12.7 million people were waiting for a corneal
transplant and only one in 70 of those would receive
a cornea.4
Novel surgical techniques emerged to
selectively replace diseased corneal layers in the form of lamellar keratoplasty. With the aid of
ophthalmic microscopes, finer surgical instruments
and equipment, corneal surgeons migrated towards
partial-thickness corneal transplants. In addition to
better visual outcomes and lower risks of rejection, a
single donor cornea may be transplanted into two or
more patients with different pathologies.5
One of the more popular forms of lamellar
keratoplasty is endothelial keratoplasty (Fig c), which
replaces the diseased corneal endothelium and allows
for the restoration of corneal clarity.6 In January 2005,
the first Descemet stripping endothelial keratoplasty
was successfully performed at the Prince of Wales
Hospital. This operation required meticulous
dissection of the donor cornea into a thicker anterior
portion and a very thin posterior layer. The posterior
lenticule (<200 μm) was implanted into the patient’s
eye and secured only by a gas bubble without any
need for suturing. Chinese eyes are known to
be technically challenging; nonetheless, visual
outcomes and complication profiles of procedures
conducted in Hong Kong patients are comparable to
international standards.7 8 9
As endothelial keratoplasty gained popularity,
in 2008, the HKEB also started to pre-cut corneal
tissues for surgeons. Having pre-cut tissues
significantly reduces the operating time and obviates
any risks of cancellation due to inadvertent graft
damage during preparation.
In 2011, Tuen Mun Eye Centre performed the
first Descemet membrane endothelial keratoplasty (DMEK).10 This form of endothelial keratoplasty
involves a much thinner donor than Descemet
stripping endothelial keratoplasty, yielding the
potential of less rejection risk and better vision (Fig d). As this membrane is extremely thin and delicate, accidental tears during preparation may occur
leading to wastage. This must be weighed against
graft shortages. Recently, a modified endothelium-in
technique utilising a pull-through device was
developed in Singapore.11 This technique was first
applied at the Caritas Medical Centre in late 2020.
In February 2013, the HAEB updated the local
criteria for cornea donation in accordance with
American and European standards.12 The pool of
potential donors was thus expanded as patients with
solid organ malignancy were able to donate their
corneas after death. In August 2018, The Chinese
University of Hong Kong Jockey Club Ophthalmic
Microsurgical Training Programme started the
first penetrating keratoplasty simulated training for
young ophthalmologists. As DMEK gains popularity,
the HAEB will advance to preparation of pre-stripped
DMEK grafts for surgeons. In May 2021, the HAEB
organised the first territory-wide DMEK wet lab for
corneal surgeons to gain hands-on experience with
stripped endothelial grafts. This was followed by a
wet lab organised by the Caritas Medical Centre on
their experience of endothelium-in DMEK.
Common to solid organ grafting, there is a
limited lifespan for any transplanted corneal graft.
In cases where further grafts are not indicated, one could resort to artificial corneas. Apart from the
more established osteo-odonto-keratoprosthesis13
and Boston keratoprosthesis, newer forms of
artificial corneas are being developed.
Corneal surgeons are excited about the
potential rho-kinase inhibitors medical therapy,
which could restore corneal endothelial health. The
use of cultivated human corneal endothelial cells and
injecting such into the anterior chamber will likely
revolutionise the concept of corneal transplant.14
As we gain knowledge in corneal genetics, we
may even be able to prevent corneal degeneration
from the outset with genetic therapy.15
Author contributions
Concept or design: AL Young.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: KW Kam.
Critical revision of the manuscript for important intellectual content: AL Young.
Acquisition of data: All authors.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: KW Kam.
Critical revision of the manuscript for important intellectual content: AL Young.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors would like to acknowledge the tremendous support and contributions from Ms Catherine Wong,
Manager of the Hong Kong Eye Bank.
Funding/support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Ethics approval is not required for this commentary which did not involve human or animal subjects.
References
1. Crawford AZ, Patel DV, McGhee CN. A brief history of corneal transplantation: from ancient to modern. Oman J
Ophthalmol 2013;6(Suppl 1):S12-7. Crossref
2. Wong KH, Kam KW, Chen LJ, Young AL. Corneal blindness
and current major treatment concern-graft scarcity. Int J
Ophthalmol 2017;10:1154-62.
3. Ho PC. Thirty-five years of eye banking in Hong Kong—a
metamorphosis and a commitment renewed. Hong Kong J
Ophthalmol 1997;1:19-24.
4. Gain P, Jullienne R, He Z, et al. Global survey of corneal
transplantation and eye banking. JAMA Ophthalmol
2016;134:167-73. Crossref
5. Young AL, Kam KW, Jhanji V, Cheng LL, Rao SK. A new era
in corneal transplantation: paradigm shift and evolution of
techniques. Hong Kong Med J 2012;18:509-16.
6. Young AL, Rao SK, Cheng LL, Lam PT. Endothelial keratoplasty. Hong Kong J Ophthalmol 2008;12:25-32.
7. Li AL, Kwok RP, Kam KW, Young AL. A 5-year analysis of endothelial vs penetrating keratoplasty graft survival in Chinese patients. Int J Ophthalmol 2020;13:1374-7. Crossref
8. Young AL, Kwok RP, Jhanji V, Cheng LL, Rao SK. Long-term outcomes of endothelial keratoplasty in Chinese eyes at a University Hospital. Eye Vis (Lond) 2014;1:8. Crossref
9. Young AL, Rao SK, Lam DS. Endothelial keratoplasty: where are we? Clin Exp Ophthalmol 2008;36:707-8. Crossref
10. Monnereau C, Quilendrino R, Dapena I, et al. Multicenter study of descemet membrane endothelial keratoplasty: first case series of 18 surgeons. JAMA Ophthalmol
2014;132:1192-8. Crossref
11. Ang M, Mehta JS, Newman SD, Han SB, Chai J, Tan D. Descemet membrane endothelial keratoplasty: preliminary
results of a donor insertion pull-through technique using a
donor mat device. Am J Ophthalmol 2016;171:27-34. Crossref
12. Hospital Authority. Cluster Presentation Programme—Kowloon Central Cluster. Eye Bank and Cornea Donation
Service in Hong Kong. 2021. Available from: https://www.ha.org.hk/haho/ho/cad_bnc/HAB-P310.pdf. Accessed 6
Jul 2021.
13. Lam NM, Rao SK, Young AL, Cheng LL, Lam DS.
Modified Osteo-Odonto Keratoprosthesis (MOOKP) in
patients with severe anterior segment disease: Our Hong
Kong Experience. ASCRS 2008. Chicago, United States
2008. Available from: http://ascrs2008.abstractsnet.com/handouts/000153_Modified_Osteo-Odonto_Keratoprosthesis_(MOOKP)_in_patients.ppt. Accessed 6 Jul 2021.
14. Kinoshita S, Koizumi N, Ueno M, et al. Injection of cultured
cells with a ROCK inhibitor for bullous keratopathy. N
Engl J Med 2018;378:995-1003. Crossref
15. Sarnicola C, Farooq AV, Colby K. Fuchs endothelial corneal dystrophy: update on pathogenesis and future directions. Eye Contact Lens 2019;45:1-10. Crossref

