© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Pictorial Blood Loss Assessment Chart for evaluating heavy menstrual bleeding in Asian women
Jennifer KY Ko, MB, BS, FHAKM (Obstetrics and Gynaecology)1; Terence T Lao, MD2; Vincent YT Cheung, FRCOG, FRCSC1
1 Department of Obstetrics and Gynaecology, The University of Hong Kong and Queen Mary Hospital, Hong Kong
2 Department of Obstetrics and Gynaecology, The University of Hong Kong (Honorary), Hong Kong
Corresponding author: Dr Jennifer KY Ko (jenko@hku.hk)
Abstract
Introduction: Heavy menstrual bleeding is a
common gynaecological problem, but some
women may prefer not to articulate their menstrual
problems. The objective of this study was to evaluate
the usefulness and acceptability of the Pictorial
Blood Loss Assessment Chart (PBAC) as a self-screening
tool in evaluation of menstrual blood loss
among Asian women in Hong Kong.
Methods: This prospective cohort study recruited
206 women from the general gynaecology ward
and out-patient clinic: 118 had self-perceived heavy
menstrual bleeding and 88 had self-perceived normal
menstrual flow. Participants were asked to fill in the
PBAC for one menstrual cycle.
Results: Compared with women who had self-perceived
normal menstrual flow, women with self-perceived
heavy menstrual bleeding had significantly
higher total PBAC scores and numbers of flooding
episodes, larger clot sizes and numbers, more days
of bleeding, and lower haemoglobin levels. Receiver-operating characteristic curve analysis demonstrated good pairwise associations of self-perceived
symptoms with PBAC score and haemoglobin level.
Conclusions: The PBAC can be used to differentiate
self-perceived heavy and normal menstrual bleeding
in Asian women in Hong Kong. It can also serve as
an additional indicator of possible heavy menstrual
bleeding to alert women of the need to seek early
medical attention.
New knowledge added by this study
- The Pictorial Blood Loss Assessment Chart (PBAC) offers a semi-objective method for evaluation of heavy menstrual bleeding in women whose cultural backgrounds may cause reluctance in discussing their gynaecological or menstrual problems.
- More than 10% of women with self-perceived normal menstrual bleeding had PBAC scores >100, had anaemia, and/or required iron supplements.
- The best PBAC cut-off score (76) yielded a sensitivity of 93.2% and a specificity of 83.0% for predicting selfperceived heavy menstrual bleeding.
- The PBAC may be useful as a self-screening tool for heavy menstrual bleeding among Asian women in Hong Kong, facilitating early medical evaluation of apparently asymptomatic women with unrecognised anaemia.
- Development of PBAC-containing mobile apps or websites may improve the usability of the PBAC in clinical and research settings.
- Localisation of the PBAC to include items encountered daily (such as ‘tofu’ or ‘palm’, rather than coins) could improve the usefulness of this tool.
- The PBAC may be useful for evaluation of responses to interventions during randomised controlled trials involving women with adenomyosis and uterine fibroids.
Introduction
The clinical decision regarding a need for treatment
of menstrual bleeding relies on the patient’s
perception of flow amount and its effects on
her physical, emotional, and social well-being.1
However, retrospective recall regarding the amount
of menstrual flow in previous cycles is heavily
influenced by a woman’s subjective perception and is not always associated with the measured blood
loss.2 The ‘gold standard’ approach for assessment
of menstrual blood loss is the alkaline haematin
method, which requires a woman to collect all
soiled sanitary products for laboratory assessment2;
however, this is a cumbersome non-hygienic impractical method outside the research setting.
The Pictorial Blood Loss Assessment Chart (PBAC) is a scoring system developed as a semi-quantitative
evaluation of menstrual blood loss,
which considers the number of sanitary products
used, the degree to which these products are soiled
with blood, the number and size of blood clots
passed, and the number of flooding episodes.3 The
PBAC has been validated with the alkaline haematin
method to diagnose heavy menstrual bleeding in
several studies in other populations.3 4 5 Furthermore,
the PBAC has been used as a measurement tool to
evaluate menstrual blood loss in systematic reviews
and randomised controlled clinical trials.6
In the clinical setting, it can be difficult for a
physician to determine the amount and implication
of menstrual flow in a patient reporting heavy
menstrual bleeding. Menstruation is a taboo topic in
many communities, including among Asian women
in Hong Kong.7 8 9 10 Some women may prefer not to, or
find it difficult or embarrassing to, articulate details
regarding their menstrual problems.7 8 9 Furthermore,
some women may be unaware of heavy menstrual
bleeding.
The objective of this study was to evaluate the
usefulness of the PBAC as a self-evaluation tool for
heavy menstrual bleeding. Additionally, we sought to
determine the acceptability of the PBAC and whether
PBAC scores were associated with menstrual blood
loss severity among Asian women in Hong Kong.
Methods
This prospective cohort study compared PBAC scores
between women who presented with and without
heavy menstrual bleeding. Women were recruited
between November 2014 and January 2016 through
the gynaecology ward or the general gynaecology
out-patient clinic of a university-affiliated hospital. They attended the out-patient clinic for routine
follow-up or were admitted to the ward for elective
or emergent treatment. Inclusion criteria included
good general health, absence of other medical
conditions which might lead to anaemia, no prior
PBAC use, and age ≥18 years. Women were excluded
if they were pregnant, in menopause, receiving
hormonal treatment, mentally incompetent,
and/or undergoing treatment/monitoring of a
gynaecological malignancy. Ethics approval was
obtained from the Institutional Review Board of The
University of Hong Kong/Hospital Authority Hong
Kong West Cluster. Written informed consent was
obtained from all study participants.
Women were approached by the research
nurse and were placed into heavy menstrual bleeding
and normal menstrual bleeding groups based on
their self-reported menstrual cycle symptoms over
the preceding 6 months. All group allocations were
noted by the nurse. All participants, regardless of
perceived menstrual flow, were instructed by the
research nurse to fill in a PBAC for one cycle in the
next cycle. They were also instructed to answer a
question regarding whether they found the PBAC
acceptable (yes/no) and a question regarding the
ease of use of the PBAC (scale of 1-5; 1=easiest
and 5=hardest). The PBAC originally described by
Higham et al3 was used, but diagrams of clot sizes
were modified to the sizes of local coins. The PBAC
consisted of a series of diagrams representing lightly,
moderately, and heavily soaked towels and tampons
(depending on the degree of staining) to evaluate
menstrual blood loss.3 The numbers of pads or
tampons used each day were recorded. In the event
of clot passage, the number and size were recorded;
flooding episodes were also recorded. A total score
was calculated by multiplying by a factor of 1 for
each lightly soiled item, 5 for each medium soiled
item, 10 for a fully soaked tampon, and 20 for a
fully soaked pad.3 Small and large clots were given a
score of 1 and 5, respectively.3 Women continued to
use their own sanitary products (ie, products used
prior to the study) and were asked to document
the types and sizes of sanitary products used. Each
woman was asked to return the completed PBAC to
the research nurse by mail in a stamped envelope.
The following clinical data were retrieved from the
women’s electronic medical records and used in the
analysis: age, haemoglobin level within 3 months
before the consultation or on the day of consultation
(if available), and the iron supplement status (using/not using).
The sample size was determined based on an
anticipated 20% difference in accuracy endpoints
between study groups and a standard deviation
of 40%. Allowing for 10% non-responders, the
calculated sample size per group was 70 women.
Statistical tests were performed using SPSS Statistics (Windows version 24; IBM Corp, Armonk [NY],
United States). Comparisons between groups were
made using the Chi squared test for categorical
variables and the non-parametric Mann–Whitney U
test for continuous variables. Continuous variables
were expressed as median and range. A P value of
<0.05 was considered statistically significant. The
kappa statistic was used to test agreement between
subjective evaluation of heavy menstrual bleeding
and the PBAC score at various cut-off scores.
Predictions of heavy menstrual bleeding according
to the PBAC score and haemoglobin level were
determined using area under the receiver-operating
characteristic curve analysis.
Results
The response rate was better than expected and
more women than expected were recruited in
each clinic session; this yielded a final sample size
larger than originally planned. However, among
292 women who were asked to complete the PBAC,
the return rate was only 206/292 (70.5%). In all,
118 women had self-perceived heavy menstrual
bleeding and 88 women had self-perceived normal
menstrual flow. Haemoglobin level data were
available in 179/292 (61.3%) women (116 in the heavy
menstrual bleeding group and 63 in the normal
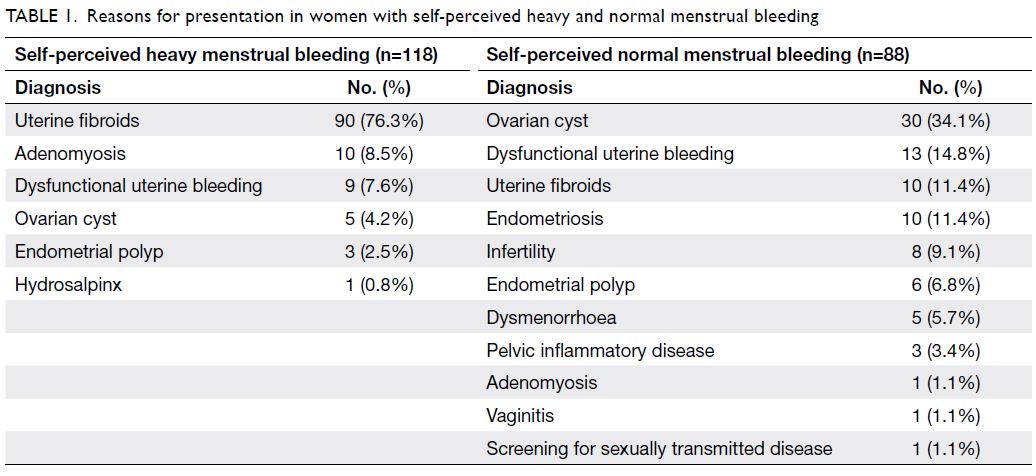
menstrual bleeding group). Table 1 summarises
the reasons for presentation in both groups of
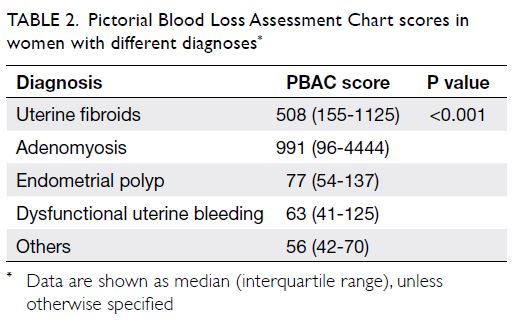
women. The PBAC scores based on different
diagnoses are shown in Table 2. Women with heavy
menstrual bleeding were older than women with
normal menstrual bleeding (median age 44 years,
[interquartile range=40-48] vs 38 years [interquartile
range=31-43], respectively, P<0.001). There was no
significant difference in education level between
groups (Table 3).
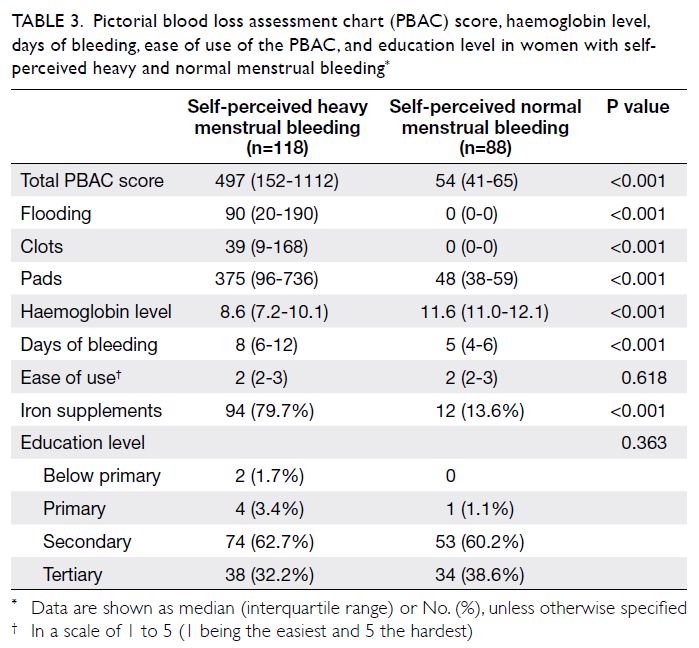
Table 3. Pictorial blood loss assessment chart (PBAC) score, haemoglobin level, days of bleeding, ease of use of the PBAC, and education level in women with selfperceived heavy and normal menstrual bleeding
Nearly all women in the study used pads; one
woman used both pads and tampons. In total, 147/206
(71.4%) women used various brands and sizes of
pads with distinct absorbency characteristics during
the menstrual cycle; the remaining 59/206 (28.6%)
women used only one type of pad. Seven women
used diapers and three women used postpartum
pads. The median PBAC scores of women who
reported heavy and normal menstrual bleeding
were 497 (interquartile range=152-1112) and 54
(interquartile range=41-65), respectively (Table 3).
Compared with women who had normal menstrual
flow, women with heavy menstrual bleeding had
significantly higher total PBAC scores and numbers
of flooding episodes, larger clot sizes and numbers,
more days of bleeding, and lower haemoglobin levels
(Table 3). Using cut-off scores of 76, 80, 100, 130, 150, and 185, levels of agreement between PBAC score
and self-reported symptoms in the diagnosis of heavy
menstrual bleeding are shown in Table 4. Women with
anaemia, defined as haemoglobin level <11.0 g/dL,
had significantly higher median PBAC scores than
did women without anaemia (508 [interquartile range=168-1087] vs 58 [interquartile range=46-84],
P<0.01). Receiver-operating characteristic curves
demonstrating the predictive abilities of the PBAC
and haemoglobin level for heavy menstrual bleeding
are shown in the Figure. The area under the receiver-operating
characteristic curves of the PBAC and
haemoglobin level for prediction of heavy menstrual
bleeding were 0.961 (95% confidence=0.940-09.982)
and 0.876 (95% confidence=0.821-0.931),
respectively. The PBAC cut-off score with the highest
Youden index was 76, which yielded a sensitivity of
93.2% and a specificity of 83.0% for predicting self-perceived
heavy menstrual bleeding.
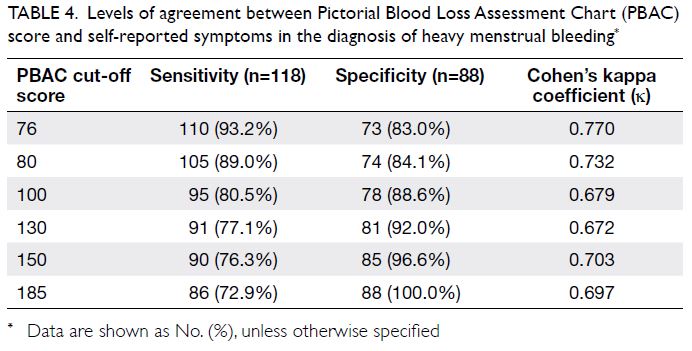
Table 4. Levels of agreement between Pictorial Blood Loss Assessment Chart (PBAC) score and self-reported symptoms in the diagnosis of heavy menstrual bleeding
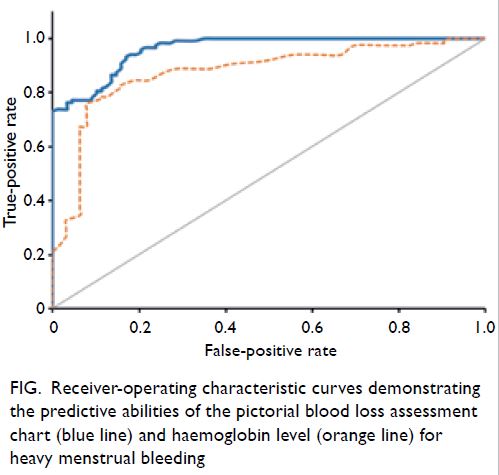
Figure. Receiver-operating characteristic curves demonstrating the predictive abilities of the pictorial blood loss assessment chart (blue line) and haemoglobin level (orange line) for heavy menstrual bleeding
All women in our study were able to complete
the PBAC. Missing information was filled in with the
help of the research nurse via phone contact after
return of the PBAC. Twenty-eight women (13.6%)
who began the PBAC on the day of consultation
were contacted by phone to urge them to return
the PBAC using the stamped envelopes. Another
11 women (5.4%) with prolonged menstrual
bleeding did not provide full details regarding their
menstrual bleeding; they were contacted by phone
for confirmation. In all, 200/206 women (97.1%)
found the PBAC acceptable: 113/118 (95.8%) in the
heavy menstrual bleeding group and 87/88 (98.9%)
in normal menstrual bleeding group. Assuming
that the reason for non-response was that those
women found the PBAC to be unacceptable, the
acceptability rate was 200/292 (68.5%). There was no
significant difference in the perceived ease of use of
the PBAC; the median rating was 2 in both groups
(P=0.618; Table 3). Notable written comments
from the women concerning the PBAC were that it
could not accurately describe their menstrual blood
loss (n=19), it required explanation (n=11), it was
inconvenient or involved recall problems (n=3), and
it did not record other symptoms which were more
distressing (n=1).
Discussion
Our results suggested that the reported PBAC
scores in this group of Asian women comprised a
useful tool for differentiating self-perceived heavy
and normal menstrual bleeding. Heavy menstrual
bleeding considerably impacts a woman’s quality of
life; interventions should be designed to improve
the quality of life, rather than focusing on the exact
amount of menstrual blood loss.1 Nevertheless,
some women may be unaware of heavy bleeding or
find it difficult to describe the amount of menstrual
flow. The PBAC offers a semi-objective method for
initial self-evaluation of the amount of menstrual
bleeding in women whose cultural backgrounds may
cause reluctance in discussing their gynaecological
or menstrual problems. This self-evaluation can alert
women to seek medical attention, thus facilitating
clinical evaluation and treatment. The PBAC cut-off scores included in Table 4 have been used in previous
studies to imply heavy menstrual bleeding.3 4 5 11
The recommendation of a particular cut-off score
depends on the clinical context (ie, whether a higher
sensitivity or specificity is required). For example, if
the PBAC is used as a screening tool, a lower cut-off
score may be appropriate to alert women to seek
medical attention. In contrast, if the PBAC is used to
evaluate women with heavy menstrual bleeding for
potential participation in a research study, a higher
cut-off score may be used to recruit women with
more severe symptoms to evaluate their response to
treatment.
In our study, 10 women (11.4%) in the self-perceived
normal menstrual bleeding group had
PBAC scores of >100, although they reported normal
menstrual bleeding. In the self-perceived normal
menstrual bleeding group, 14 women had anaemia
(haemoglobin level <11.0 g/dL), among which five
women had a haemoglobin level of <10.0 g/dL.
Twelve women who reported normal menstrual
bleeding were using iron supplements. Although
most women accurately recognised heavy menstrual
bleeding, use of the PBAC identified an additional
10% of women who might have unperceived
abnormal bleeding. Of the 10 women with self-perceived
normal menstrual bleeding (PBAC scores
of 101-180), seven (70%) had anaemia. Thus, use
of the PBAC might enable identification of a small
group of apparently asymptomatic women who had
unrecognised anaemia, thereby facilitating earlier
medical attention.
In our study, women were asked to use their
own sanitary products, rather than using specific
brands and sizes of pads; thus, our findings are more
representative of realistic PBAC use, compared
with results acquired in a research setting. Most
women used different brands and sizes of pads with
different absorbency characteristics, even within
a single cycle. In addition, several women used
adult diapers or postpartum pads, which implied
substantial difference in blood loss compared with
the usual sanitary pads. The range of PBAC scores
was much larger in our study than in previous
studies.3 4 5 11 12 One woman in our study had a PBAC
score of 32 301; she had prolonged vaginal bleeding
for 56 days and had a haemoglobin level of 4.5 g/dL.
Women with adenomyosis and uterine fibroids had
significantly higher PBAC scores than did women
with other diagnoses. Therefore, the PBAC may be
useful for evaluation of responses to interventions
during randomised controlled trials involving these
groups.
Although women in our study who returned
the PBAC found it acceptable and generally easy to
use, the return rate should be considered. Notably,
19/206 (9.2%) women commented that the range of
icons in the PBAC did not accurately reflect their blood loss on pads or clots because they experienced
difficulty in evaluating the amount of blood loss
(based on a particular stain) when comparing among
pads with different absorbency characteristics. The
clots were of irregular size and women felt that a
scale or use of items encountered daily (such as ‘tofu’
or ‘palm’, rather than coins) could more accurately
describe these clots. Women (particularly in the
heavy menstrual bleeding group) who had to sit on
the toilet during flooding episodes could not quantify
their bleeding; several women with prolonged
bleeding did not continue the PBAC evaluation
because they felt that continuing the documentation
was time-consuming and annoying. In total, 5.3%
of the women commented that clearer instructions
could be provided. This is consistent with the
findings by Zakherah et al,5 who reported that
improved instructions led to greater accuracy when
a physician or nurse reviewed the documentation
with the patient. The role of the nurse in our study
was crucial. Our research nurse found it helpful to
demonstrate to the women how to fill in the PBAC
using their current or previous cycle; the nurse also
helped the women to complete the PBAC in the event
of substantial missing information, especially among
women with prolonged menstrual bleeding. Some
women probably completed the PBAC by recall,
rather than in a day-by-day manner. This aspect
should be considered when the PBAC is applied as
a self-screening tool. The development of PBAC-containing
mobile apps or websites accessible by the
public may improve the usability of the PBAC as a
self-screening tool in terms of better convenience
and less recall bias, especially among younger
women.
Our study had some limitations. First, we
only evaluated use of the PBAC in a small group
of patients who presented for clinical treatment,
rather than the general population; this may limit
the generalisability of the results. Second, we did not
study the inter-cycle variability in PBAC score or the
effects of other demographic factors (eg, household
income) which may affect the use of the PBAC.
Although only one cycle of menstrual bleeding was
charted in our study and women may have unusual
menstrual flow in subsequent cycles, previous
studies have demonstrated high consistency with
low inter-cycle variation in women who completed a
second PBAC evaluation without treatment.11 Third,
patients may have been offered treatment during the
consultation; because the PBAC was completed in
the cycle after consultation, the PBAC score may not
fully reflect the pre-consultation reported symptoms,
especially among women with self-perceived heavy
menstrual bleeding. Fourth, compliance with iron
therapy was not checked; this could have affected the
haemoglobin results. However, the aim of our study
was to evaluate the relationship between the PBAC score and self-perceived menstrual flow. Overall,
the results of this population-specific study might
support the use of the PBAC as a potential self-screening
tool for heavy menstrual bleeding among
Asian women in Hong Kong.
There is considerable endpoint heterogeneity
in the current literature with respect to the
outcomes of various treatment options for heavy
menstrual bleeding. Furthermore, there is currently
no core outcome set for valid comparison and
interpretation of data from research studies and
assessments regarding abnormal uterine bleeding.6
Although PBAC scores have shown high inter-individual
variation, they had low intra-individual
variation;11 thus, the PBAC may be useful in future
studies of treatment responses in individual women.
Despite the large variety of commercially available
sanitary products, the PBAC remains a reliable
screening tool for semi-quantitative evaluation of
menstrual blood loss, which can alert women to seek
medical attention for heavy menstrual bleeding.
Additional studies are needed to confirm the clinical
usefulness of the PBAC, especially in the context of
the evolution and advancement of superabsorbent
sanitary products currently available. Overall, the
advantages of the PBAC are its relative objectivity
and flexibility as a tool for screening, diagnosis, and
evaluation of treatment effect.
Author contributions
Concept or design: JKY Ko, VYT Cheung.
Acquisition of data: JKY Ko, VYT Cheung.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: JKY Ko.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: JKY Ko, VYT Cheung.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: JKY Ko.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank Ms Wai-ki Choi for patient recruitment, teaching women about the Pictorial Blood Loss Assessment
Chart, and managing the database.
Declaration
The study was presented in an oral presentation at the FOCUS in O&G 2018 Congress in Hong Kong (17-18 November 2018).
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Ethics approval was obtained from the Institutional Review Board of The University of Hong Kong/Hospital Authority
Hong Kong West Cluster (Ref: UW 14-299). Written informed
consent was obtained from all study participants.
References
1. National Institute for Health and Care Excellence guideline.
Heavy menstrual bleeding: assessment and management.
14 Mar 2018 (last updated 24 May 2021). Available from:
http://www.nice.org.uk/guidance/ng88. Accessed 25 Nov 2021.
2. Magnay JL, O’Brien S, Gerlinger C, Seitz C. A systematic
review of methods to measure menstrual blood loss. BMC
Womens Health 2018;18:142. Crossref
3. Higham JM, O’Brien PM, Shaw RW. Assessment of
menstrual blood loss using a pictorial chart. Br J Obstet
Gynaecol 1990;97:734-9. Crossref
4. Janssen CA, Scholten PC, Heintz AP. A simple visual
assessment technique to discriminate between
menorrhagia and normal menstrual blood loss. Obstet
Gynecol 1995;85:977-82. Crossref
5. Zakherah MS, Sayed GH, El-Nashar SA, Shaaban MM.
Pictorial blood loss assessment chart in the evaluation of
heavy menstrual bleeding: diagnostic accuracy compared
to alkaline hematin. Gynecol Obstet Invest 2011;71:281-4. Crossref
6. Herman MC, Penninx J, Geomini PM, Mol BW, Bongers MY.
Choice of primary outcomes evaluating treatment for
heavy menstrual bleeding. BJOG 2016;123:1593-8. Crossref
7. Garg S, Anand T. Menstruation related myths in India: strategies for combating it. J Family Med Prim Care
2015;4:184-6. Crossref
8. The Lancet Child Adolescent Health. Normalising
menstruation, empowering girls. Lancet Child Adolesc
Health 2018;2:379. Crossref
9. Agampodi TC, Agampodi SB. Normalising menstruation,
empowering girls: the situation in Sri Lanka. Lancet Child
Adolesc Health. 2018;2:e16. Crossref
10. Wong WC, Li MK, Chan WY, et al. A cross-sectional
study of the beliefs and attitudes towards menstruation of
Chinese undergraduate males and females in Hong Kong. J
Clin Nurs 2013;22:3320-7. Crossref
11. Hald K, Lieng M. Assessment of periodic blood loss:
interindividual and intraindividual variations of pictorial
blood loss assessment chart registrations. J Minim Invasive
Gynecol 2014;21:662-8. Crossref
12. Reid PC, Coker A, Coltart R. Assessment of menstrual
blood loss using a pictorial chart: a validation study. BJOG
2000;107:320-2. Crossref