Hong Kong Med J 2021 Aug;27(4):258–65 | Epub 26 Feb 2021
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Effect of SARS and COVID-19 outbreaks on
urology practice and training
CH Yee, MB, BS, FRCS (Urol)1,2; HF Wong, MB, ChB1,2; Mandy HM Tam, MB, ChB, FRCS (Urol)1,3; Steffi KK Yuen, MB, BS, FRCS (Urol)1,4; HC Chan, MB, ChB, FRCS (Urol)5; MH Cheung, MB, ChB, FRCS (Urol)6; Alan TO Yu, MB, BS, FRCS (Urol)7,8; Y Chiu, MB, ChB, FRCS (Urol)9;
NH Chan, MB, ChB, FRCS (Urol)10; LH Leung, MB, ChB, FRCS (Urol)11; Ada TL Ng, MB, BS, FRCS (Urol)12,13; Denathan MC Law, MB, BS, FRCS (Urol)14; TL Ng, MB, BS, FRCS (Urol)15; Jeremy YC Teoh, MB, BS, FRCS (Urol)1,2; Peter KF Chiu, MB, ChB, FRCS (Urol)1,2; CF Ng, MB, ChB, FRCS (Urol)1,2
1 SH Ho Urology Centre, Department of Surgery, The Chinese University of Hong Kong, Hong Kong
2 Department of Surgery, Prince of Wales Hospital, Shatin, Hong Kong
3 Department of Surgery, Alice Ho Miu Ling Nethersole Hospital, Hong Kong
4 Department of Surgery, North District Hospital, Hong Kong
5 Department of Surgery, United Christian Hospital, Hong Kong
6 Department of Surgery, Tseung Kwan O Hospital, Hong Kong
7 Department of Surgery, Tuen Mun Hospital, Hong Kong
8 Department of Surgery, Pok Oi Hospital, Hong Kong
9 Department of Surgery, Princess Margaret Hospital, Hong Kong
10 Department of Surgery, Pamela Youde Nethersole Eastern Hospital, Hong Kong
11 Department of Surgery, Kwong Wah Hospital, Hong Kong
12 Department of Surgery, Queen Mary Hospital, Hong Kong
13 Department of Surgery, Tung Wah Hospital, Hong Kong
14 Department of Surgery, Caritas Medical Centre, Hong Kong
15 Department of Surgery, Queen Elizabeth Hospital, Hong Kong
Corresponding author: Dr CH Yee (yeechihang@surgery.cuhk.edu.hk)
Abstract
Introduction: The objective was to investigate the
changes in urology practice during coronavirus
disease 2019 (COVID-19) pandemic with a
perspective from our experience with severe acute
respiratory syndrome (SARS) in 2003.
Methods: Institutional data from all urology
centres in the Hong Kong public sector during the
COVID-19 pandemic (1 Feb 2020–31 Mar 2020)
and a non-COVID-19 control period (1 Feb 2019–31 Mar 2019) were acquired. An online anonymous
questionnaire was used to gauge the impact of
COVID-19 on resident training. The clinical output
of tertiary centres was compared with data from the
SARS period.
Results: The numbers of operating sessions, clinic
attendance, cystoscopy sessions, prostate biopsy,
and shockwave lithotripsy sessions were reduced by
40.5%, 28.5%, 49.6%, 44.8%, and 38.5%, respectively,
across all the centres reviewed. The mean numbers of
operating sessions before and during the COVID-19
pandemic were 85.1±30.3 and 50.6±25.7, respectively
(P=0.005). All centres gave priority to cancer-related
surgeries. Benign prostatic hyperplasia-related
surgery (39.1%) and ureteric stone surgery (25.5%)
were the most commonly delayed surgeries. The
degree of reduction in urology services was less
than that during SARS (47.2%, 55.3%, and 70.5%
for operating sessions, cystoscopy, and biopsy,
respectively). The mean numbers of operations
performed by residents before and during the
COVID-19 pandemic were 75.4±48.0 and 34.9±17.2,
respectively (P=0.002).
Conclusion: A comprehensive review of urology practice during the COVID-19 pandemic revealed changes in every aspect of practice.
New knowledge added by this study
- As in other parts of the world, the impact of coronavirus disease 2019 on urology affected all key aspects of service. However, the degree of impact was less than that during the severe acute respiratory syndrome epidemic.
- Urology training was affected by the dramatic reduction in the number of surgeries performed for benign prostatic hyperplasia and urolithiasis.
- A prompt infection control response on the hospital level and heightened public awareness of personal hygiene have reduced the risk of infection among medical personnel to a minimal level.
- A prioritisation policy of surgeries and services by malignancy alone during pandemics is worth reconsideration. More detailed differentiation of the urgency of interventions is needed to cover the whole spectrum of diseases, from benign to malignant.
Introduction
In November 2002, there were reports of severe
pneumonia of unknown aetiology in Guangdong
Province in Southern China, which totalled more
than 300 cases by February 2003.1 The disease was
spread to Hong Kong in February 2003 through a
visitor from southern China, eventually leading to
hospital and community outbreaks.2 The World
Health Organization (WHO) named the condition
severe acute respiratory syndrome (SARS) and issued
a global alert and instituted worldwide surveillance
on 13 March 2003.3 A novel coronavirus (SARS-CoV)
was identified as the causative agent.4 The epidemic
reached its peak in Hong Kong at the end of March
2003, when the disease was spread to the community,
and it was eventually brought under control in
May 2003. By the end of the epidemic in July 2003,
8096 cases had been reported in 29 countries and
regions, with a death toll of 774 (9.6%).5
Seventeen years later, a coronavirus took
the world by surprise again. At the end of 2019, a
cluster of patients with pneumonia of unidentified
cause were reported in Wuhan, China.6 The first
case of similar pneumonia of unknown aetiology
outside China was reported in Thailand on
13 January 2020, and subsequently, the disease struck
Hong Kong on 23 January 2020. The novel virus is designated as severe acute respiratory syndrome
coronavirus-2 (SARS-CoV-2), and the standard
name of coronavirus disease 2019 (COVID-19)
was announced by the WHO to correspond to the
pneumonia caused by this novel coronavirus. On
30 January 2020, the WHO declared a ‘public health
emergency of international concern’, and later, on
11 March 2020, COVID-19 was characterised by the
WHO as a pandemic.7
The impact of COVID-19 affected the whole
spectrum of clinical practice, just like it has affected
every corner of the world. Although urology does
not stand at the forefront of care for patients with
COVID-19, every practising urologist has been
affected by the global outbreak. Hong Kong is
in the unique position of having dealt with two
serious coronavirus outbreaks in two decades. The
invaluable lessons learnt from SARS in 2003 can help
the urology community to face COVID-19 in 2020.
The current study aimed to review the territory-wide
urology practice in Hong Kong during SARS and
COVID-19 from the perspectives of both practising
urologists and urology residents in training.
Methods
Hong Kong’s healthcare system is divided into a
government-run service and a private sector. The
public sector dominates secondary and tertiary care,
accounting for approximately 80% of all hospital
admissions, 90% of total bed-days, and 100% of
professional training for doctors.8 The current study
focused on a comprehensive review of urology
practice in Hong Kong’s public sector.
This study was approved by the ethics
committee of our institution. All 11 urology units
in the public sector were included in the review
(Table 1). For ease of interpretation, two hospitals
were sometimes grouped as a single unit when
they provide a comprehensive urology service
together. Four areas were investigated to assess the
impact of COVID-19 in the urology community:
(1) new urology practice strategies introduced;
(2) new infection control measures for urologists;
(3) training and academic activities; and (4) cross-specialty
deployment from urology teams to
support COVID-19 frontline staff. With regard to
new urology practice strategies and new infection
control measures, five aspects of urology services
were individually studied: (1) surgery; (2) out-patient
clinics; (3) endoscopy; (4) prostate biopsy; and (5)
shockwave lithotripsy (SWL).
After COVID-19 spread to Hong Kong at the
end of January, the number of new cases rose steadily.
A brief surge was observed in March 2020 due to an
increase of imported cases before travel restrictions
were implemented.9 Urology service data from
1 February 2020 to 31 March 2020 were collected
from all centres in the public sector to investigate the impact of COVID-19 on the four previously
mentioned areas of urology practice and training.
Similar data from 1 February 2019 to 31 March
2019 were captured as a control for comparison.
Furthermore, an anonymous online questionnaire
was sent to all urology residents to gauge the impact
of COVID-19 on training in detail.
The Prince of Wales Hospital was at the
forefront of the SARS outbreak in Hong Kong in
2003.2 The Hospital’s urology service during SARS
(ie, 1 March 2003-30 April 2003) was reviewed using
institutional data. A control period from 1 March
2004 to 30 April 2004 was adopted for comparison
against the urology practice during SARS. Descriptive
statistics were used to characterise the demographic
data. Continuous variables were described as
means, and categorical variables were described as
frequencies. Means were compared using t tests with
statistical significance set at 5%. The SPSS software
package (Windows version 22.0; IBM Corp, Armonk
[NY], United States) was used for analysis.
Results
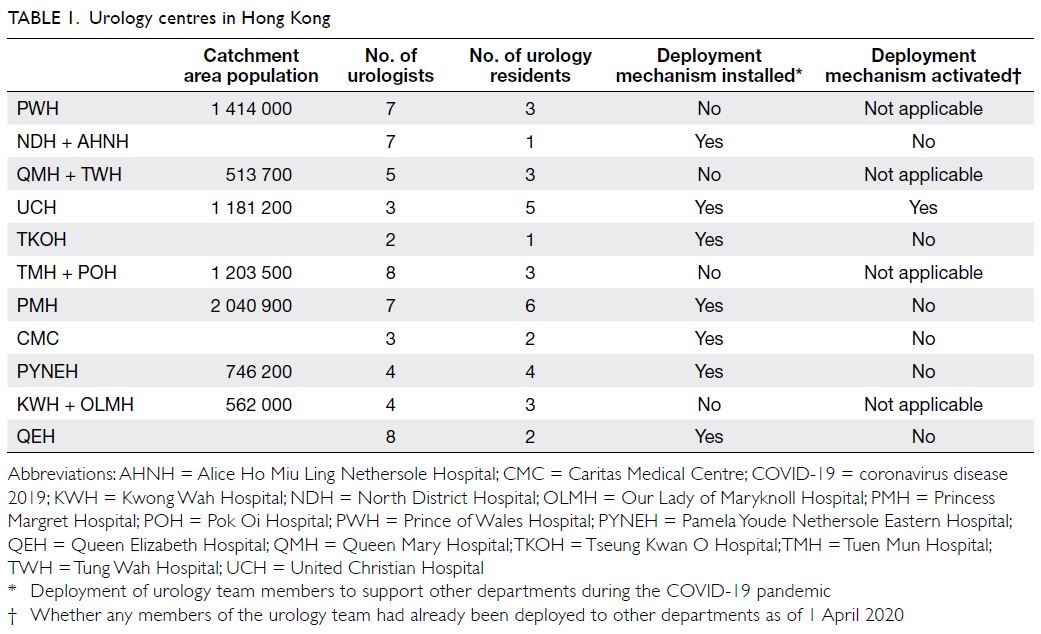
The review covered 11 urology units encompassing
the urology practice of 15 hospitals in Hong Kong
that serve a population of 7.5 million (Table 1).10
All of the investigated urology units have reduced
their numbers of operating sessions (Fig 1). The first
hospital began to reduce surgeries on 27 January
2020, only 4 days after the first COVID-19 case was
confirmed in Hong Kong. Across all urology units, the mean numbers of operating sessions before
the COVID-19 pandemic (1 Feb 2019–31 March
2019) and during the COVID-19 pandemic (1 Feb
2020–31 March 2020) were 85.1±30.3 and 50.6±25.7,
respectively (P=0.005). All urology units have given
priority to cancer or cancer-related surgeries. The
most commonly delayed type of surgery during
the COVID-19 pandemic was benign prostatic
hyperplasia–related surgery, accounting for 39.1% of
all delayed cases, followed by ureteric stone surgery
(25.5%). In addition, all living-related transplant
surgeries were suspended during the COVID-19
pandemic period.
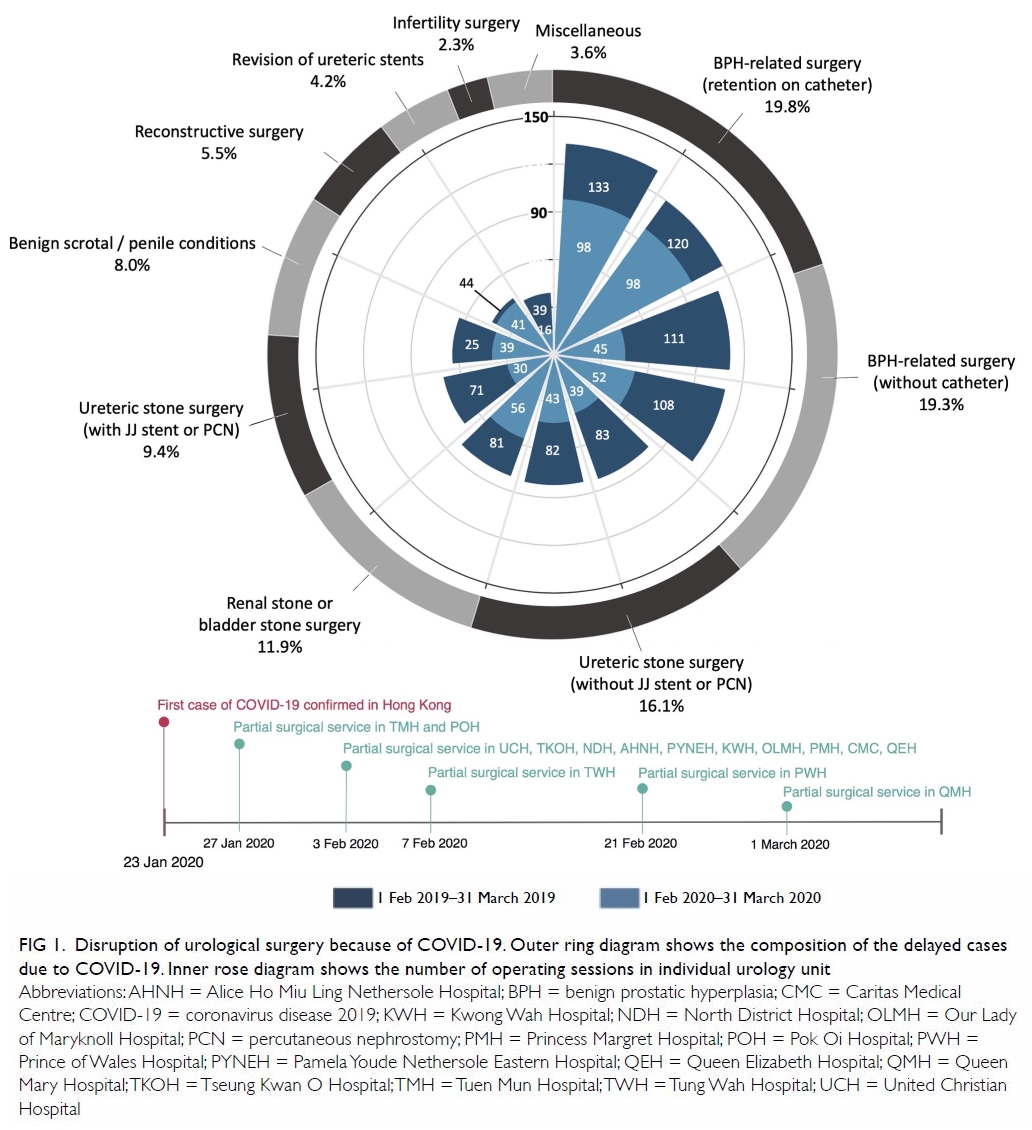
Figure 1. Disruption of urological surgery because of COVID-19. Outer ring diagram shows the composition of the delayed cases due to COVID-19. Inner rose diagram shows the number of operating sessions in individual urology unit
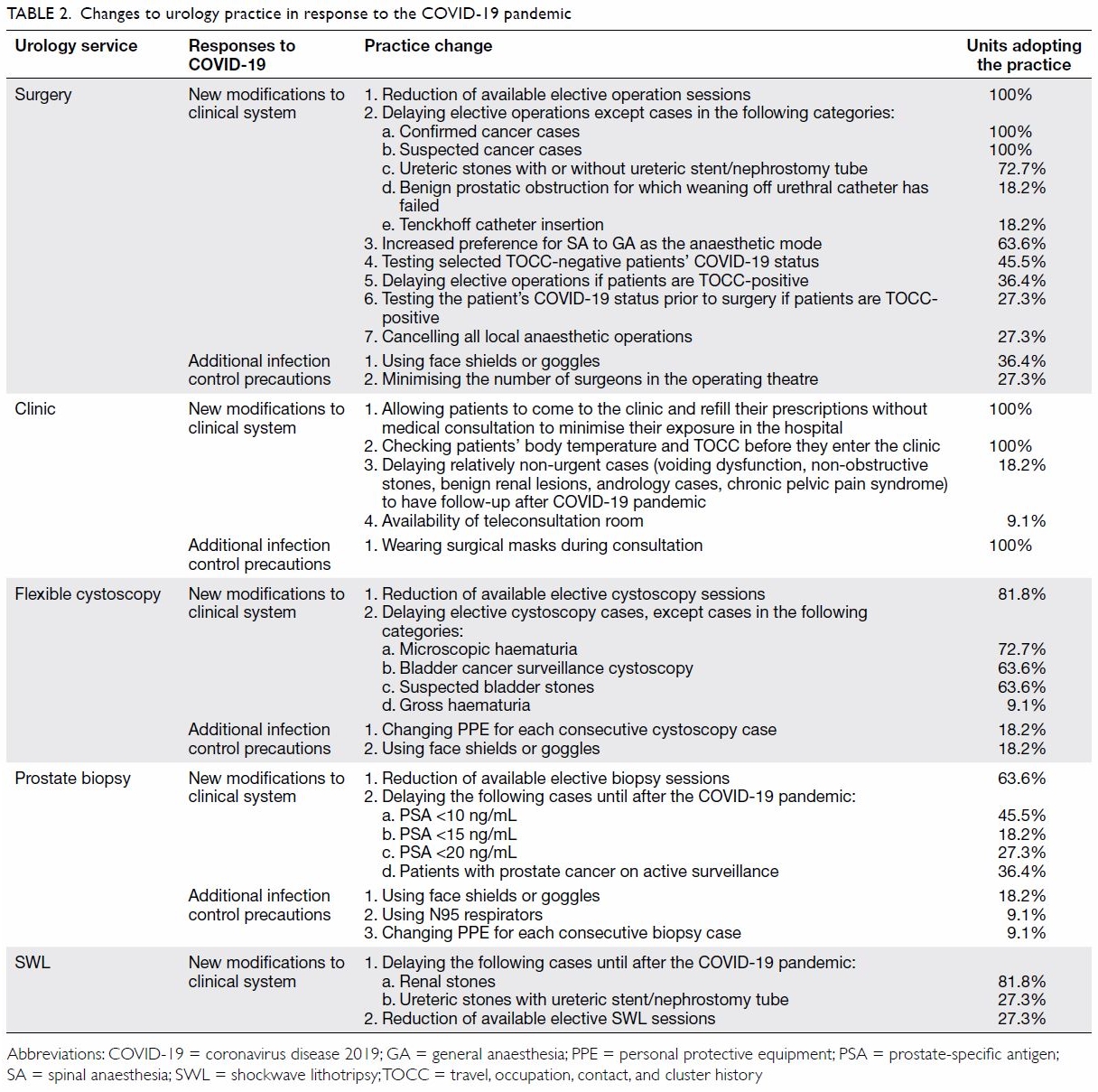
All five aspects of urology services have been
reduced in the territory (Fig 2). The numbers of
operating sessions, clinic attendance, cystoscopy
sessions, prostate biopsies, and SWL cases were
reduced by 40.5%, 28.5%, 49.6%, 44.8%, and 38.5%,
respectively across all of the reviewed centres.
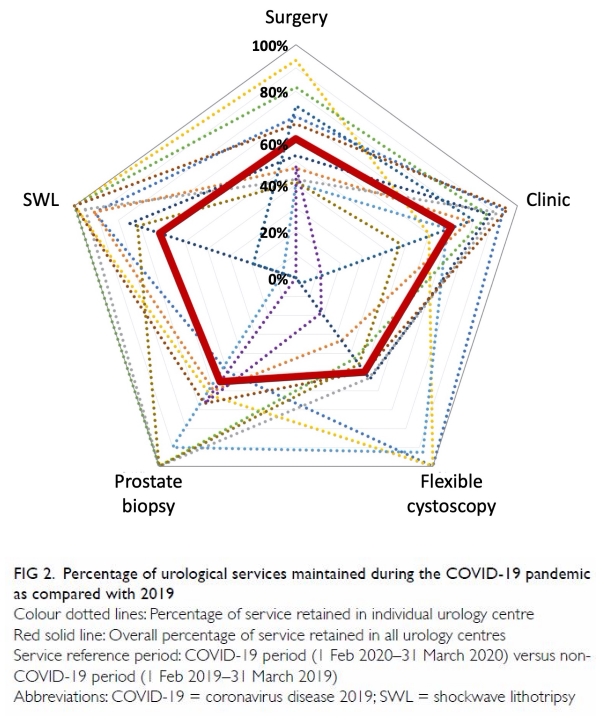
Figure 2. Percentage of urological services maintained during the COVID-19 pandemic as compared with 2019
Table 2 summarises the practice changes in
the urology units. These included special attention
to patients with TOCC (travel, occupation, contact,
and cluster history) risk of COVID-19 infection.
These patients were either deferred in their hospital
attendance or were assessed by a dedicated group
of medical personnel so as to achieve efficient
use of personal protective equipment (PPE).
Teleconsultation was available in one of the centres
for urologists to carry out clinical consultations with
TOCC-positive patients. Most urologists executed
their clinical duties wearing regular surgical masks.
Only one urology centre used N95 respirators in clinical practice, specifically for prostate biopsy.
A comparison of urology services in Prince of
Wales Hospital between the COVID-19 pandemic
in 2020 and the SARS period in 2003 is shown in
Figure 3. There was less reduction in all aspects during
COVID-19 than during SARS (operating sessions:
30.9% vs 47.2%; cystoscopy: 27.7% vs 55.3%; prostate
biopsy: 47.6% vs 70.5%; SWL: 13.9% vs 23.6%). The
percentage reductions of different urology services
during the COVID-19 pandemic in Prince of Wales
Hospital were all less than those during the SARS
period in 2003. The absolute urology output during
SARS actually exceeded that during the 2004 non-SARS normal time in some areas, including flexible cystoscopy and SWL cases.
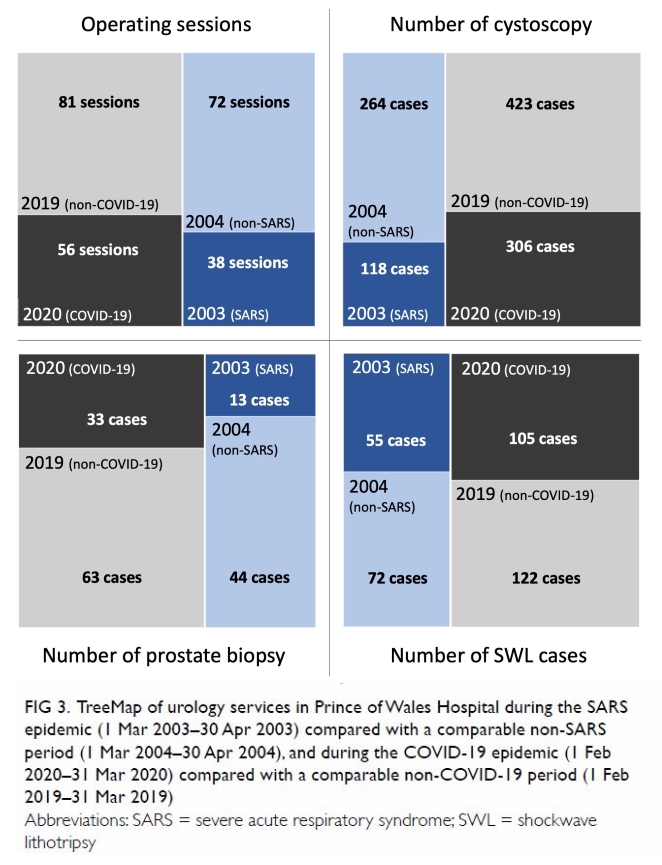
Figure 3. TreeMap of urology services in Prince of Wales Hospital during the SARS epidemic (1 Mar 2003–30 Apr 2003) compared with a comparable non-SARS period (1 Mar 2004–30 Apr 2004), and during the COVID-19 epidemic (1 Feb 2020–31 Mar 2020) compared with a comparable non-COVID-19 period (1 Feb 2019–31 Mar 2019)
Training and academic activities were heavily
affected by the COVID-19 pandemic (online
supplementary Appendix). The survey of urology
residents yielded a response rate of 48.5% (16/33).
Surgical exposure was significantly hampered, and
53.3% of the respondents had their professional
examinations cancelled because of COVID-19,
resulting in delays in their acquisition of professional
qualifications. Three out of the 11 centres reported
having switched some of their academic meetings to
online platforms.
Discussion
The most obvious impact of COVID-19 on urology
practice has been the reduction of different aspects of
urology service. The deliberate reduction of various
surgeries and out-patient investigation sessions
carries a twofold intention. Besides attempting to
minimise infection risk via reduction of patient flow
in hospital clinical areas, such actions were also a
response to the worldwide crisis of PPE shortage.11
By providing limited service, especially with regard
to the availability of general anaesthetic sessions
for surgery, it is hoped that adequate PPE can be
reserved for frontline staff members who have to
handle patients with COVID-19.
Risk assessment based on quantifiable criteria
is essential in the selection of patients whose surgical
or investigative procedures are to be deferred. All
centres adopted prostate-specific antigen (PSA)
level as a guideline for rearranging prostate biopsy
priority. Chiu et al12 demonstrated that a Prostate
Health Index cut-off of 35 produced a high-grade
prostate cancer detection sensitivity of 82% and
specificity of 74%. Its diagnostic performance is
superior to that of PSA, PSA density, and free-to–total PSA ratio) among patients with PSA values of
2 to 20 ng/mL. When its usage is more widely
accepted by the urology community in practice, it
could provide useful guidance in prioritising patients
for prostate biopsy when resources are limited.
Most centres in the study reserved operating
sessions for cancer cases or complicated stones.
This is largely in line with the recommendation of
Stensland et al13, who suggested that uncomplicated
endourology procedures, reconstructive surgeries,
transplant surgeries, and andrological interventions
be delayed. A similar perspective was endorsed
by the European Association of Urology.14
Subcategorisation of urological cancer surgeries
is necessary because of the wide spectrum of
cancer behaviour within the specialty.13 14 High-grade
bladder cancer, advanced kidney cancer, and
testicular cancer should take priority for operations,
whereas most prostatectomies for prostate cancer
should be delayed. In the current review, no
differentiation was assigned to hospital policies of
prioritising cancer surgery. Delays in interventions
for other benign conditions could ultimately increase
the risk of complications and unscheduled hospital
admissions. Nevo et al15 reported that prolonged
stent dwelling time was a risk factor for postoperative
sepsis. Prospective assessment is needed to evaluate
our current surgery triage protocol.
There are still conflicting opinions regarding
the risk of SARS-CoV-2 transmission during
laparoscopic and robotic surgery. The SARS-CoV-2
virus can remain viable and infectious in aerosols
for hours,16 but respiratory aerosol-generating
procedures seem to have a higher viral content and thus pose a greater risk of transmission than surgical
aerosol-generating procedures that aerosolise
blood and tissue fluid.17 The EAU Robotic Urology
Section recommended that laparoscopic and robotic
surgeries proceed with the necessary precautions.18
In all of the centres reviewed in the study,
laparoscopic and robotic surgeries were executed
with conventional infection control protocols. Thus
far, no COVID-19 cases have been reported to be
transmitted via laparoscopic or robotic surgery.
With respect to the PPE used, regular use of
face shields or goggles was not observed in most
centres. Evidence so far has shown that besides
the respiratory system, SARS-CoV-2 can infect the
digestive system and the urinary system, causing
the virus to be found in the stool and urine.19 Ling
et al20 reported COVID-19 cases in which urine
samples remained positive even after throat swabs
had converted negative. A similar observation about
stool was reported by Chen et al,21 who found that
64.29% of patients tested positive for viral RNA
in faeces after pharyngeal swabs turned negative.
As asymptomatic COVID-19 patients have been
reported,22 and contact with urine and stool during
urological procedures is not uncommon, the optimal standard of PPE for urologists needs further consideration.
We observe that the surveyed residents’
training and academic activities were affected by
the current pandemic. Furthermore, there may
be a preference for surgical interventions to be
performed by more experienced surgeons so as to
reduce the operating time.23 In addition, most of the
delayed cases during this COVID-19 pandemic were
endourology cases (Fig 1), which account for the main bulk of urology resident training materials. A
similar observation was echoed by urology residents
in Italy.24
The outbreak of SARS in 2003 marked a
critical turning point in Hong Kong. Invaluable
lessons were learnt, including improvements
in infection control measures and more rapid
response. The public has perceived face masks as a
tool for preventing infection both during the SARS
outbreak and in the post-SARS era.25 Lau et al26 reported that 70.7% of the respondents to a survey
in Hong Kong would frequently wear masks, 67.3%
would avoid going to hospitals, and 71.5% would
avoid going to crowded places if a few new SARS
cases were reported. Further, healthcare workers
have developed good infection control habits (eg,
hand hygiene precautions and appropriate PPE
selection).8 These elements all contributed to the
multi-faceted strategies of different institutions’
urology departments when they were confronted by
COVID-19 in 2020. The current study revealed that
measures to minimise the infection risk were adopted
in the very early phase of COVID-19 emergence. All
of the investigated urology centres have reorganised
their services to decrease patient flow and reduce the
risk of mass gathering. Together with the heightened
public awareness of personal hygiene, these factors
could assist with containment of infection. Taking
Prince of Wales Hospital as an example, the clinical
output of minimal services during the COVID-19
pandemic was still higher than that in 2004 during
the post-SARS period. This pattern is expected to be
similar in other major urology centres in Hong Kong
considering the growth in population and service
need. However, no hospital outbreaks of COVID-19
have been observed so far in Hong Kong, unlike
during SARS, and unlike a number of centres in other
parts of the world during COVID-19. The experience
of SARS in Hong Kong might have inadvertently
prepared medical personnel across all specialties in
our locality to face this COVID-19 pandemic with a
more timely and comprehensive reaction.
A limitation of our study is that we did not
investigate behaviour in the private sector. However,
the public sector accounts for about 70% of hospital-based
services provided in Hong Kong,27 and thus,
it is reasonable to interpret the current study as a
meaningful representation of urology practice across
the whole city during the COVID-19 pandemic.
Conclusion
Our study on urology practice reviewed the impact
of COVID-19 from a metropolitan-city-wide
perspective. The unique experience of the SARS
outbreak in 2003 prepared Hong Kong in an unusual
way to face the current pandemic of COVID-19.
Changes to every aspect of urology practice were
observed. Rapid responses from surgical teams in
concert with the efforts from different specialties
in the medical field have minimised the risk of
outbreaks in hospitals and institutions. Prospective
studies are needed to review the outcomes of these
changes to urology practice.
Author contributions
CH Yee and CF Ng contributed to the concept of the study. CH Yee contributed to the analysis and interpretation of
data, and drafting of the manuscript. All authors contributed to the acquisition of data and critical revision for important
intellectual content. All authors had full access to the data,
contributed to the study, approved the final version for
publication, and take responsibility for its accuracy and
integrity.
Conflicts of interest
As editors of the journal, JYC Teoh and CF Ng were not involved in the peer review process. Other authors have
disclosed no conflicts of interest.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The study was approved by the ethics committee of our
institution’s Survey and Behavioural Research Ethics board
(Ref SBRE-19-563).
References
1. Zhong NS, Zheng BJ, Li YM, et al. Epidemiology and
cause of severe acute respiratory syndrome (SARS) in
Guangdong, People’s Republic of China, in February, 2003. Lancet 2003;362:1353-8. Crossref
2. Tomlinson B, Cockram C. SARS: experience at Prince of
Wales Hospital, Hong Kong. Lancet 2003;361:1486-7. Crossref
3. Tsang KW, Ho PL, Ooi GC, et al. A cluster of cases of
severe acute respiratory syndrome in Hong Kong. N Engl J
Med 2003;348:1977-85. Crossref
4. Peiris JS, Yuen KY, Osterhaus AD, Stöhr K. The severe
acute respiratory syndrome. N Engl J Med 2003;349:2431-
41. Crossref
5. Hui DS. Severe acute respiratory syndrome (SARS): lessons
learnt in Hong Kong. J Thorac Dis 2013;5 Suppl 2:S122-6.
6. Li Q, Guan X, Wu P, et al. Early transmission dynamics in
Wuhan, China, of novel coronavirus-infected pneumonia.
N Engl J Med 2020;382:1199-207. Crossref
7. World Health Organization. WHO director-general’s
opening remarks at the media briefing on COVID-19–
11 March 2020. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Accessed 17 Apr 2020.
8. Food and Health Bureau, Hong Kong SAR Government.
Report of the strategic review on healthcare manpower
planning and professional development. Available from:
https://www.fhb.gov.hk/en/press_and_publications/otherinfo/180500_sr/srreport.html. Accessed 17 Apr 2020.
9. Centre for Health Protection, Hong Kong SAR
Government. Coronavirus disease (COVID-19) in HK.
Available from: https://chp-dashboard.geodata.gov.hk/covid-19/en.html. Accessed 17 Apr 2020.
10. Census and Statistics Department, Hong Kong SAR
Government. Population. Available from: https://www.censtatd.gov.hk/hkstat/sub/so20.jsp. Accessed 17 Apr 2020.
11. Ranney ML, Griffeth V, Jha AK. Critical supply shortages—the need for ventilators and personal protective equipment
during the COVID-19 pandemic. N Engl J Med
2020;382:e41. Crossref
12. Chiu PK, Ng CF, Semjonow A, et al. A multicentre
evaluation of the role of the prostate health index (PHI)
in regions with differing prevalence of prostate cancer:
adjustment of PHI reference ranges is needed for European
and Asian settings. Eur Urol 2019;75:558-61. Crossref
13. Stensland KD, Morgan TM, Moinzadeh A, et al.
Considerations in the triage of urologic surgeries during
the COVID-19 pandemic. Eur Urol 2020;77:663-6. Crossref
14. Ribal MJ, Cornford P, Briganti A, et al. European
Association of Urology Guidelines Office Rapid Reaction
Group: an organisation-wide collaborative effort to adapt the European Association of Urology Guidelines
recommendations to the coronavirus disease 2019 era. Eur
Urol 2020;78:21-8. Crossref
15. Nevo A, Mano R, Baniel J, Lifshitz DA. Ureteric stent
dwelling time: a risk factor for post-ureteroscopy sepsis.
BJU Int 2017;120:117-22. Crossref
16. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol
and surface stability of SARS-CoV-2 as compared with
SARS-CoV-1. N Engl J Med 2020;382:1564-7. Crossref
17. Cook TM. Personal protective equipment during the
coronavirus disease (COVID) 2019 pandemic—a narrative
review. Anaesthesia 2020;75:920-7. Crossref
18. Mottrie A. EAU Robotic Urology Section (ERUS)
guidelines during COVID-19 emergency. Available from:
https://uroweb.org/eau-robotic-urology-section-erusguidelines-
during-covid-19-emergency/. Accessed 17 Apr
2020.
19. Ozma MA, Maroufi P, Khodadadi E, et al. Clinical
manifestation, diagnosis, prevention and control of SARS-CoV-
2 (COVID-19) during the outbreak period. Infez Med
2020;28:53-65.
20. Ling Y, Xu SB, Lin YX, et al. Persistence and clearance of
viral RNA in 2019 novel coronavirus disease rehabilitation
patients. Chin Med J (Engl) 2020;133:1039-43. Crossref
21. Chen Y, Chen L, Deng Q, et al. The presence of SARS-CoV-2 RNA in feces of COVID-19 patients. J Med Virol
2020;92:833-40.Crossref
22. Bai Y, Yao L, Wei T, et al. Presumed asymptomatic carrier
transmission of COVID-19. JAMA 2020;323:1406-7. Crossref
23. Porpiglia F, Checcucci E, Amparore D, et al. Slowdown
of urology residents’ learning curve during COVID-19
emergency. BJU Int 2020;125:E15-7. Crossref
24. Amparore D, Claps F, Cacciamani GE, et al. Impact of the
COVID-19 pandemic on urology residency training in
Italy. Minerva Urol Nefrol 2020;72:505-9. Crossref
25. Siu JY. Qualitative study on the shifting sociocultural
meanings of the facemask in Hong Kong since the severe
acute respiratory syndrome (SARS) outbreak: implications
for infection control in the post-SARS era. Int J Equity
Health 2016;15:73. Crossref
26. Lau JT, Yang X, Pang E, Tsui HY, Wong E, Wing YK.
SARS-related perceptions in Hong Kong. Emerg Infect Dis
2005;11:417-24.
27. Census and Statistics Department, Hong Kong SAR
Government. Thematic household survey report No. 63.
December 2017. Available from: https://www.statistics.gov.hk/pub/B11302632017XXXXB0100.pdf. Accessed 10 Apr 2020.