Hong Kong Med J 2021 Apr;27(2):113–7 | Epub 15 Nov 2020
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Effect of COVID-19 on delivery plans and
postnatal depression scores of pregnant women
PW Hui, MD, FRCOG; Grace Ma, MHSM (Health Services Management); Mimi TY Seto, MB, BS, MRCOG; KW Cheung, MB, BS, MRCOG
Department of Obstetrics and Gynaecology, Queen Mary Hospital, Pokfulam, Hong Kong
Corresponding author: Dr PW Hui (apwhui@hku.hk)
Abstract
Introduction: Owing to the coronavirus disease
2019 outbreak Hong Kong hospitals have suspended
visiting periods and made mask wearing mandatory.
In obstetrics, companionship during childbirth has
been suspended and prenatal exercises, antenatal
talks, hospital tours, and postnatal classes have
been cancelled. The aim of the present study was to
investigate the effects of these restrictive measures
on delivery plans and risks of postpartum depression.
Methods: We compared pregnancy data and the
Edinburgh Postpartum Depression Scale (EPDS)
scores of women who delivered between the
pre-alert period (1 Jan 2019 to 4 Jan 2020) and
post-alert period (5 Jan 2020 to 30 Apr 2020) in a
tertiary university public hospital in Hong Kong.
Screening for postpartum depression was performed
routinely using the EPDS questionnaire 1 day and
within 1 week after delivery.
Results: There was a 13.1% reduction in the number
of deliveries between 1 January and 30 April from
1144 in 2019 to 994 in 2020. The EPDS scores were
available for 4357 out of 4531 deliveries (96.2%). A
significantly higher proportion of women had EPDS
scores of ≥10 1 day after delivery in the post-alert group than the pre-alert group (14.4% vs 11.9%;
P<0.05). More women used pethidine (6.2% vs 4.6%)
and fewer used a birthing ball (8.5% vs 12.4%) for
pain relief during labour in the post-alert group.
Conclusions: Pregnant women reported more
depressive symptoms in the postpartum period
following the alert announcement regarding
coronavirus infection in Hong Kong. This was
coupled with a drop in the delivery rate at our public
hospital. Suspension of childbirth companionship
might have altered the methods of intrapartum pain
relief and the overall pregnancy experience.
New knowledge added by this study
- The delivery rate at a public hospital was reduced during the coronavirus disease 2019 (COVID-19) pandemic.
- Women who delivered in the public hospital had higher Edinburgh Postnatal Depression Scale scores during the coronavirus alert period.
- A lower rate of non-pharmacological pain relief and a higher rate of pethidine usage were observed during labour.
- Obstetricians should be aware of the psychological burden of the COVID-19 outbreak on pregnant women, especially in the immediate postpartum period.
- Alternative measures and effective intervention should be available to support these women during this pandemic crisis.
Introduction
The outbreak of coronavirus disease 2019
(COVID-19) leads to a declaration of a serious level
of response on 4 January 2020, which was escalated
to the emergency level on 25 January 2020.1 2
Corresponding policies were imposed by the Hospital
Authority at that time. Visiting periods were
suspended, and mask wearing became mandatory
in hospitals. In obstetrics, companionship during
childbirth was stopped, as were visits to newborns
staying with mothers in the postnatal ward. All prenatal exercise, antenatal talks, hospital tours,
and postnatal classes were cancelled. The infection
continued to spread worldwide, and a pandemic
was declared by the World Health Organization on
11 March 2020. The first case of a COVID-19-infected
pregnant mother was confirmed on 20 March 2020.
The Hong Kong Government has further restricted
travel and tightened social distancing and other
measures to limit the spread of COVID-19.
Increased psychological stress and anxiety
levels have been reported in countries with major outbreaks.3 4 As reflected by the Edinburgh Postnatal
Depression Scale (EPDS), pregnant women assessed
after the declaration of the COVID-19 epidemic had
significantly higher rates of depressive symptoms
than women assessed before the announcement
in China.5 6 Behavioural changes have also been
recognised among pregnant women.7 This evolving
situation and its concomitant alterations in obstetric
care can potentially pose extra psychological stress
during the peripartum period.
In our university-affiliated tertiary hospital in
Hong Kong, screening for women at risk of or having
emotional problems is performed for all pregnancies
antenatally during a booking visit. Counselling
and support are provided by trained midwives and
nurses from Comprehensive Child Development
Service to those in need. Postpartum depression is
routinely assessed after delivery using the validated
EPDS.8 9 The aim of the present study was to examine
the effect of COVID-19 and its concurrent service
adjustments on couples’ obstetric planning and
postpartum depression.
Methods
This was a retrospective study of the delivery data
and EPDS scores of women who delivered at Queen
Mary Hospital in Hong Kong from 1 January 2019
to 30 April 2020. Information related to the original
number of bookings, actual deliveries, childbirth
companionship, basic demographics, mode of delivery, epidural rate, and other methods of pain
relief were retrieved from the Clinical Information
System and Clinical Data Analysis and Reporting
System of the Hospital Authority.
Screening for postpartum depression was
performed routinely by asking all women to complete
the EPDS questionnaire 1 day after delivery.
This assessment was conducted again by phone
within 1 week after delivery. The EPDS consists of
10 questions with a maximum score of 30 and has
a validated Chinese version.9 10 A cut-off of ≥10
was adopted locally. Women with high scores were
counselled by a dedicated team of midwives and
psychiatric nurses.
Comparisons of delivery data and EPDS scores
were performed between women who delivered
during the pre-alert period (1 Jan 2019 to 4 Jan 2020)
and the post-alert period (5 Jan 2020 to 30 Apr 2020).
Analysis was performed using SPSS (Windows
version 25; IBM Corp, Armonk [NY], United States).
Student’s t tests and Chi squared tests were used as
appropriate with P<0.05 considered as statistically
significant.
Results
There were 1997 pregnant women with expected
delivery dates between January 2020 and April 2020
booked for delivery at Queen Mary Hospital, as
compared with 1869 bookings for the corresponding
4-month period in 2019. However, there was a
13.1% reduction in the number of actual deliveries
between 1 January and 30 April, from 1144 in 2019
to 994 in 2020. Fewer than half of the total number
of women who originally booked for delivery in our
hospital eventually delivered there, and the drop was
more profound from February to April 2020. As a
result, there were 3577 deliveries from 1 January
2019 to 4 January 2020 (ie, the pre-alert group) and
954 deliveries from 5 January 2020 to 30 April 2020
(ie, the post-alert group).
A significantly higher proportion of Chinese
women (85.1% vs 81.5%; P<0.05) delivered during
the post-alert period, while proportion of women
with labour companionship was significantly
reduced (21.8% vs 88.8%; P<0.05) compared with
the pre-alert period. For pain relief during labour,
more women received pethidine injections and
fewer women used a birthing ball during the post-alert
period. The other parameters were comparable
between the two groups (Table 1).
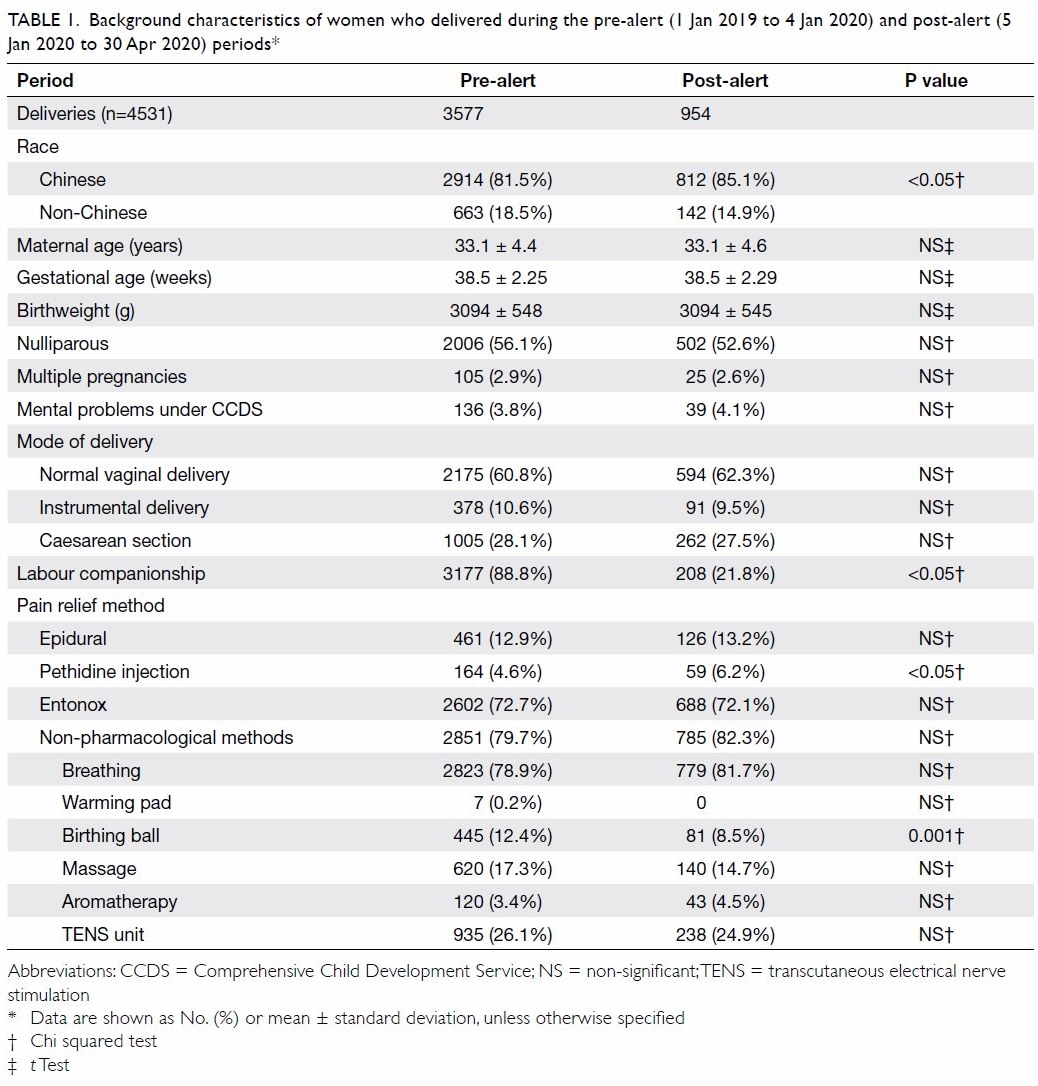
Table 1. Background characteristics of women who delivered during the pre-alert (1 Jan 2019 to 4 Jan 2020) and post-alert (5 Jan 2020 to 30 Apr 2020) periods
Out of 4531 total deliveries, EPDS scores
were available for 4357 (96.2%) 1 day after delivery
and 3772 (83.2%) within 1 week after delivery. A
significantly higher proportion of women had EPDS
scores of ≥10 1 day after delivery in the post-alert
group compared with the pre-alert group (14.4% vs
11.9%; P<0.05). This proportion was reduced to 2.9%
on the second assessment within 1 week of delivery, at which point the scores became comparable with those of the pre-alert group (2.3%).
Compared with the first assessment 1 day
after delivery, women in both groups demonstrated
significantly lower mean EPDS scores on the
second assessment within 1 week (pre-alert group:
4.71 vs 1.36; post-alert group: 4.93 vs 1.42; P<0.01).
The mean EPDS scores obtained on both 1 day
(4.93 vs 4.71) and within 1 week (1.42 vs 1.36) after
delivery were higher following the declaration of alert
response, although the difference was statistically
insignificant. The monthly mean EPDS score 1 day
after delivery was higher during the post-alert period
(range, 4.87-4.99) than during the pre-alert period
(4.71; 95% confidence interval=4.57-4.85; Table 2).
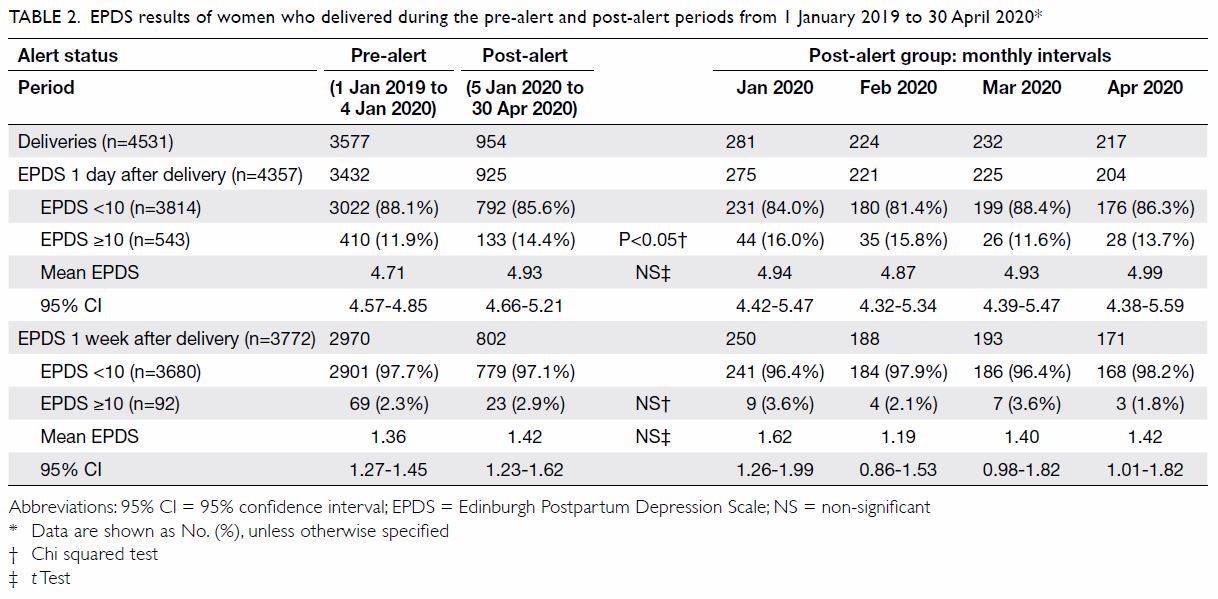
Table 2. EPDS results of women who delivered during the pre-alert and post-alert periods from 1 January 2019 to 30 April 2020
Discussion
The present study is the first to report the impact
of COVID-19 on obstetric care and postpartum
depression in Hong Kong. The delivery rate in public
hospitals has dropped dramatically in the post-alert
period. This drop has been more profound since
February 2020, especially among non-Chinese
women. As of 30 April 2020, there had been three
confirmed COVID-19 cases in pregnant women in
Hong Kong. Although local changes in public health
behaviour, social distancing, and isolation have
largely contained the local outbreak of COVID-19,2
these policies could disrupt couples’ delivery plans.
The reduced delivery rate could represent a shift of
childbirth from public hospitals to private ones that did not manage suspected or confirmed COVID-19
patients. Non-Chinese women might have returned
to their home countries out of fear of COVID-19.
Women who deliver in public hospitals now
increasingly have to face the challenge of childbirth
without the companionship of family members and
complete their hospital stay without visitors. All of
these could account for the reduced delivery rate in
the public sector.
Another important finding was the increased
proportion of women with high EPDS scores in
the post-alert period. We observed an increase
in EPDS scores shortly after delivery during the
post-alert period. This aligns with the findings of a
multicentre study conducted in China following the
announcement of human-to-human transmission.6
The COVID-19 pandemic could cause health
anxiety and postpartum depression.7 11 Women of
reproductive age in Hong Kong experienced
the severe adult respiratory syndrome
epidemic in 2002 to 2003. Thus, these women are potentially more
stressed than those in other countries. An emergency
response was raised in Hong Kong even before the
declaration of a pandemic by the World Health
Organization. The practice of mask wearing has been
widely adopted previously, and supplies have been
in huge demand in the past.1 The memories
of severe acute respiratory syndrome coupled with
the abrupt changes in social behaviour during the
post-alert period might have triggered more stress
in pregnant women and been reflected in their EPDS
scores. Moreover, those who remained in the public
system might not have had alternative delivery
options elsewhere. Pregnant women are vulnerable to postpartum depression, and early identification
and effective intervention from Comprehensive
Child Development Service might help to relieve
these women’s stress. These adverse effects could also
potentially be ameliorated by the provision of online
education materials, a lactation support hotline,
early postnatal discharge, and family support.
Childbirth is a major life event for a family.
Companions can provide information about
childbirth, bridge communication gaps between
healthcare workers and women, and facilitate
non-pharmacological pain relief. They can also
provide practical support, including encouraging
women in labour to move around, providing
massages, and holding their hands.12 The overall
usage of non-pharmacological pain relief was similar
between the pre- and post-alert periods. However,
a significantly lower proportion of women used
a birthing ball for pain relief during labour in the
post-alert period, probably secondary to the
suspension of childbirth companionship. Fewer
women received childbirth massages, as they are
usually provided by companions. Contrary to
this, more women needed pethidine injections
during labour. This indicates the contributory role
of childbirth companionship to women’s overall
birthing experience.
The present study illustrates the impact of
COVID-19 on pregnant women’s delivery plans and
the need for attention to their emotional disturbance.
This is important information for obstetricians
to consider during the revision and adjustment
of service provision. Remedial measures like
teleconferencing and early postnatal discharge can
facilitate speedy recovery from distress. Although we noted increased levels of postnatal depression
in the post-alert period, this study was not designed
to study the contributory effects of COVID-19,
cessation of childbirth companionship, or
elimination of visiting hours to postnatal depression.
Another limitation is the lack of data on anxiety
levels, which could provide a more comprehensive
picture of the pregnant women’s emotional health.
Moreover, this review is limited to the assessment
of women who ultimately delivered in our hospital.
Such women might be more adaptive and prepared
for the altered environment than those who chose
to give birth in the private sector or abroad. As
the study was restricted to one public hospital, the
findings might not be generalisable to hospitals in
other catchment areas, which may have different
population characteristics. The policies of restricted
gathering and social distancing might affect the
arrangements of family celebrations, baby showers,
and the cultural practice of ‘doing the month’. It will
be of interest to examine whether women’s stress
and anxiety levels change during the later postnatal
period. Further study is warranted to examine the
social and psychological responses of pregnant
women during the COVID-19 pandemic.
Conclusion
Measures to limit the spread of COVID-19 have
resulted in fewer deliveries in our public hospital
and more symptoms of postpartum depression.
Obstetricians should be aware of these effects on
the psychosocial well-being of pregnant women and
offer timely intervention to provide stress relief.
Author contributions
Concept or design: All authors.
Acquisition of data: PW Hui, G Ma, MTY Seto.
Analysis or interpretation of data: PW Hui.
Drafting of the manuscript: PW Hui.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: PW Hui, G Ma, MTY Seto.
Analysis or interpretation of data: PW Hui.
Drafting of the manuscript: PW Hui.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank all midwives and nurses for their contributions to the assessment of postnatal depression in
women who delivered at Queen Mary Hospital.
Funding/support
This research received no specific grant from any funding
agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This research has been approved by the Institutional Review
Board of the University of Hong Kong/Hospital Authority
West Cluster (HKU/HA HKW IRB; Ref UW 20-419).
References
1. Leung GM, Cowling BJ, Wu JT. From a sprint to a marathon in Hong Kong. N Engl J Med 2020;382:e45. Crossref
2. To KK, Yuen KY. Responding to COVID-19 in Hong Kong. Hong Kong Med J 2020;26:164-6. Crossref
3. Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak.
Asian J Psychiatr 2020;51:102076. Crossref
4. Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-
Gorrochategui M, Idoiaga-Mondragon N. Stress, anxiety,
and depression levels in the initial stage of the COVID-19
outbreak in a population sample in the Northern Spain [in
English, Spanish]. Cad Saude Publica 2020;36:e00054020. Crossref
5. Wang C, Pan R, Wan X, et al. Immediate psychological
responses and associated factors during the initial stage
of the 2019 coronavirus disease (COVID-19) epidemic
among the general population in China. Int J Environ Res
Public Health 2020;17:1729. Crossref
6. Wu Y, Zhang C, Liu H, et al. Perinatal depressive and
anxiety symptoms of pregnant women along with COVID-19 outbreak in China. Am J Obstet Gynecol 2020;223:240.
e1-9. Crossref
7. Corbett GA, Milne SJ, Hehir MP, Lindow SW, O’Connell MP.
Health anxiety and behavioural changes of pregnant
women during the COVID-19 pandemic. Eur J Obstet
Gynecol Reprod Biol 2020;249:96-7. Crossref
8. Leung WC, Kung F, Lam J, Leung TW, Ho PC. Domestic
violence and postnatal depression in a Chinese community.
Int J Gynaecol Obstet 2002;79:159-66. Crossref
9. Cox JL, Holden JM, Sagovsky R. Detection of postnatal
depression. Development of the 10-item Edinburgh
Postnatal Depression Scale. Br J Psychiatry 1987;150:782-6. Crossref
10. Lee DT, Yip SK, Chiu HF, et al. Detecting postnatal
depression in Chinese women. Validation of the Chinese
version of the Edinburgh Postnatal Depression Scale. Br J
Psychiatry 1998;172:433-7. Crossref
11. Rashidi Fakari F, Simbar M. Coronavirus pandemic and
worries during pregnancy; a letter to editor. Arch Acad
Emerg Med 2020;8:e21.
12. Bohren MA, Berger BO, Munthe-Kaas H, Tunçalp Ö.
Perceptions and experiences of labour companionship:
a qualitative evidence synthesis. Cochrane Database Syst
Rev 2019;(3):CD012449. Crossref

