Hong Kong Med J 2021 Apr;27(2):106–12 | Epub 25 Mar 2021
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Behavioural insights and attitudes on community
masking during the initial spread of COVID-19 in Hong Kong
Victor CW Tam1, SY Tam1, ML Khaw2, Helen KW Law1, Catherine PL Chan3, Shara WY Lee1
1 Department of Health Technology and Informatics, Faculty of Health and Social Sciences, The Hong Kong Polytechnic University, Hong Kong
2 Tasmanian School of Medicine, University of Tasmania, Hobart Tasmania 7001, Australia
3 Department of Otorhinolaryngology, Head and Neck Surgery, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong
Corresponding author: Dr Shara WY Lee (shara.lee@polyu.edu.hk)
Abstract
Introduction: Community face mask use during the
coronavirus disease 2019 (COVID-19) pandemic has
considerably differed worldwide. Generally, Asians
are more inclined to wear face masks during disease
outbreaks. Hong Kong has emerged relatively
unscathed during the initial outbreak of COVID-19, despite its dense population. Previous infectious
disease outbreaks influenced the local masking
behaviour and response to public health measures.
Thus, local behavioural insights are important for
the successful implementation of infection control
measures. This study explored the behaviour and
attitudes of wearing face masks in the community
during the initial spread of COVID-19 in Hong
Kong.
Methods: We observed the masking behaviour of
10 211 pedestrians in several regions across Hong
Kong from 1 to 29 February 2020. We supplemented
the data with an online survey of 3199 respondents’
views on face mask use.
Results: Among pedestrians, the masking rate
was 94.8%; 83.7% wore disposable surgical masks.
However, 13.0% wore surgical masks incorrectly with
42.5% worn too low, exposing the nostrils or mouth;
35.5% worn ‘inside-out’ or ‘upside-down’. Most
online respondents believed in the efficacy of wearing
face mask for protection (94.6%) and prevention of community spread (96.6%). Surprisingly, 78.9%
reused their mask; more respondents obtained
information from social media (65.9%) than from
government websites (23.2%).
Conclusions: In Hong Kong, members of the
population are motivated to wear masks and believe
in the effectiveness of face masks against disease
spread. However, a high mask reuse rate and errors
in masking techniques were observed. Information
on government websites should be enhanced and
their accessibility should be improved.
New knowledge added by this study
- A high mask reuse rate was observed during the initial spread of coronavirus disease 2019 in Hong Kong.
- Masking errors were observed among 13.0% of the pedestrians wearing surgical masks in this study, while mask reuse was reported by 78.9% of respondents in an online survey.
- Although official government websites were regarded as reliable, they were less popular than social media for the acquisition of health-related information.
- Increased efforts are needed to educate the general public regarding the correct use and handling of masks.
- Manufacturers are encouraged to provide clear instructions on their packaging and print a symbol on each mask to prevent users from wearing masks inside-out.
- Because of the popularity of social media, authorities should utilise these platforms as a supplement to their standard websites for better public exposure and communication concerning health-related information.
Introduction
The rapid and devastating spread of the coronavirus
disease 2019 (COVID-19) pandemic caught the
global community unprepared and overwhelmed
the disease control measures of many nations.
Measures deployed in Hong Kong to control the spread of COVID-19 were less stringent than those
adopted in other nations; however, they proved to be
effective.1 Territory-wide lockdowns, curfews, and
the controversial surveillance of smartphone data for
contact tracing purposes were all avoided. A recent
local study showed that behavioural changes were the key factors associated with limiting the spread of
COVID-19 and seasonal influenza.1
Community masking by healthy individuals
is controversial and opinions on its effectiveness or
necessity differ among health authorities worldwide.2
Since the severe acute respiratory syndrome (SARS)
epidemic in 2003, the population of Hong Kong
has maintained a strong masking culture. Although
masking in crowded areas has always been voluntary
in Hong Kong, rates of 61% and 79% during the SARS
outbreak were recorded in two previous studies.3 4 In
the present study, we aimed to explore the masking
behaviour of pedestrians in crowded areas, as well
as the attitude of the population towards community
masking, during the initial spread of COVID-19 in
Hong Kong.
Methods
Study design
This study protocol was approved by the Human
Subjects Ethics Application Review board of The
Hong Kong Polytechnic University and complied with
the Declaration of Helsinki. The Strengthening the
Reporting of Observational Studies in Epidemiology
(STROBE) checklist for cross-sectional studies was
implemented in the drafting of this article. The study
protocol consisted of two parts: an observational
study (Part 1) and an online survey (Part 2).
Part 1: Observational study approach
The masking behaviour of pedestrians in Hong Kong
was observed between 1 and 29 February 2020.
Eleven well-populated locations across Hong Kong
were selected for observation. Observation sites on
the main street of each location were chosen based
on pedestrian throughput, and the ability to observe
pedestrians in a clear, unhindered manner without
interrupting the flow of traffic. Three observation
sessions per day were conducted at 12:00-14:30
(lunch time), 14:30-17:00 (afternoon), and 17:00-19:30 (evening). To reduce selection bias, the location
and observation times were randomly preselected
on the evening before each study by drawing two sets
of shuffled opaque envelopes containing the session
time and locations.
On days with sufficient rain to warrant
umbrella use, further observations were terminated.
The data collected until the occurrence of rain were
included for analysis. One observer was allocated to
each session and the following data were collected:
frequency of masking, type of mask worn, and
number and type of erroneous masking practices.
Only pedestrians walking in one direction were
observed to prevent duplicate counting. The criteria
for seven common types of masking errors were
based on deviations from the surgical mask use
guidelines published by the Hong Kong Centre for
Health Protection.5 The definitions for masking errors were standardised before the study by
consensus among the observers after a field test.
Part 2: Online survey approach
Members of the Hong Kong population were
included in an online survey of behaviour and views
on community masking, which was conducted
between 23 March and 14 April 2020. Consent
was implied in the voluntary participation and
completion of the survey. Personal information was
not collected; however, demographic details (eg, age,
gender, education level, and whether the respondents
were healthcare students or professionals [HCSPs])
were recorded. Short-term visitors were excluded by
targeting only respondents who had lived in Hong
Kong for the preceding 6 months.
A link to the online survey was distributed
via various means such as social media and email.
The survey required approximately 5 minutes to
complete. A 5-point Likert scale was used to grade
respondents’ perceptions of mask efficacy for
protection and the prevention of community spread,
evaluation of mask performance, and confidence in
mask selection and correct use of mask. Respondents
were also asked about mask reuse habits and storage,
and information sources for COVID-19–related
health matters, including their perceived reliability
of those sources. A sample questionnaire is shown in
the online supplementary Appendix.
Statistical analysis
Statistical analysis was performed by an independent
statistician using IBM SPSS Statistics (Windows
version 21.0, IBM Corp. Armonk [NY], United
States). Univariate logistic regression and univariate
ordinal regression were used to explore associations
with binary and ordinal outcomes, respectively.
Crude odds ratios (ORs) for each demographic
variable were calculated from univariate analysis.
Multivariate regression analyses were then
performed, including all demographic variables, and
the adjusted OR was estimated for each demographic
variable. Descriptive statistics were used to provide
an overview of the observations; the findings of
regression analysis were presented as ORs and 95%
confidence intervals (CIs). A P value of <0.05 was
considered statistically significant.
Results
Part 1: Observational study
In total, 10 211 pedestrians were observed over
25 sessions. The masking rate was 94.8%; most
pedestrians wore disposable surgical masks (83.7%),
and a small number wore N95 respirators (0.7%).
The remaining pedestrians wore an assortment of
face masks made of fabric or neoprene rubber; a few
wore gas masks.
Among pedestrians wearing surgical masks,
masking errors were observed in 1113 (13.0%)
individuals (Table 1). The most common errors
observed included: mask worn too low, exposing the
nostrils and mouth (42.5%), or mask worn inside-out/upside-down (35.5%). A less common but
serious error was the absence of hand hygiene after
touching their masks (16.4%).
Part 2: Online survey
A total of 3199 respondents completed the survey.
Data from 74 non-residents were excluded, and the
remaining 3125 responses were analysed. Female respondents comprised a larger proportion (65.7%),
education status was at diploma level or above for
76.9% of the respondents, and 18.6% were HCSPs
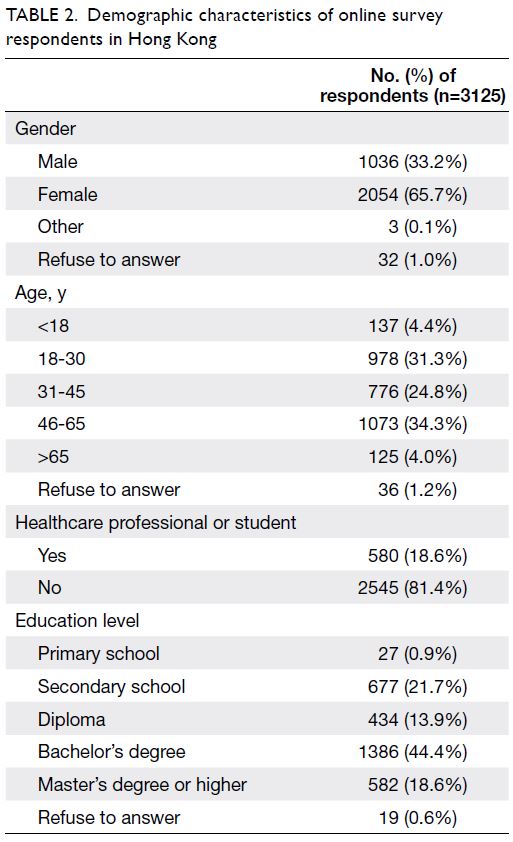
(Table 2).
Views on face mask performance
Most online respondents were confident of using
a face mask correctly (96.9%) and believed in its
efficacy for protection (94.6%) and the prevention
of community spread (96.6%). Most respondents
indicated that they clearly understood the functions
of the different types of masks available (83.6%) and
were confident of their ability to evaluate those masks
(77.1%). Multivariate ordinal regression analyses
showed that HCSPs were associated with greater
confidence (OR=1.62; 95% CI=1.34-1.95; P<0.001)
of using a face mask correctly; while increasing age
was associated with lower confidence (OR=0.87;
95% CI=0.81-0.94; P<0.001 for each successive age-group).
However, no significant associations were
found with education level or gender.
Reuse of mask
In all, 78.9% of the respondents reused their face
masks and stored them using a variety of methods: between tissue papers (74.1%), in paper envelopes
(46.5%), in plastic bags (22.9%), left on table
(6.5%), and in plastic containers (6.0%) [Table 3].
Multivariate logistic regression analyses concerning
reuse of face masks showed greater likelihood among
respondents with higher education level (OR=1.14;
95% CI=1.05-1.24; P=0.003 for each successive
education level), older age (OR=1.48; 95% CI=1.35-1.62;
P<0.001 for each successive age-group), and HCSP status (OR=1.61; 95% CI=1.26-2.07; P<0.001). Gender was not associated with mask reuse.
Sources of health information
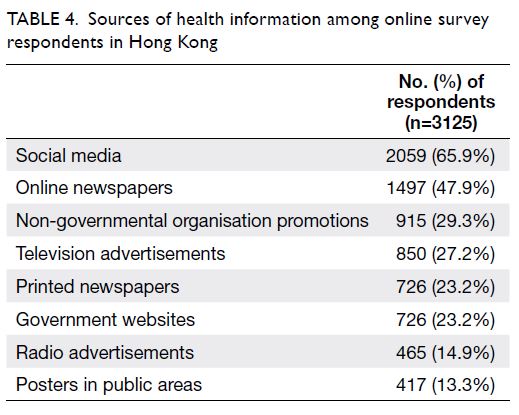
More respondents reported the acquisition of
information on mask usage via social media (65.9%)
and online newspapers (47.9%), compared with
official government websites (23.2%) [Table 4].
Ratings for reliability were highest for government
websites (69.9%), followed by online (64.6%) and
printed (64.5%) newspapers (Table 5).
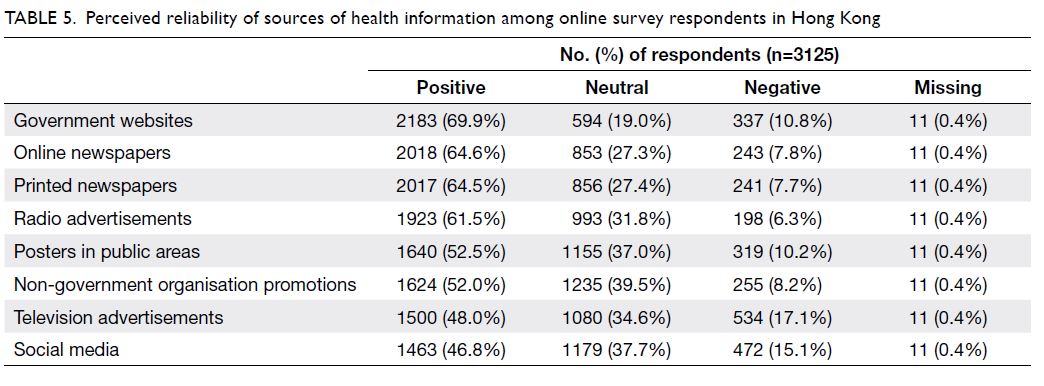
Table 5. Perceived reliability of sources of health information among online survey respondents in Hong Kong
Subanalysis of healthcare students or
professionals
Compared with other respondents, HCSPs had a
better understanding of mask types and indications
for each type (multivariate ordinal regression:
OR=1.93; 95% CI=1.60-2.34; P<0.001). They were
more likely to choose surgical masks (multivariate
logistic regression: OR=2.43; 95% CI=1.04-5.72;
P=0.041) and less likely to choose N95 respirators
(OR=0.54; 95% CI=0.44-0.68; P<0.001) for
community use. They were also more likely to reuse
their face masks (OR=1.61; 95% CI=1.26-2.07;
P<0.001) and store them between tissues (OR=1.80;
95% CI=1.47-2.21; P<0.001), but less likely to use
paper envelopes (OR=0.80; 95% CI=0.65-0.98;
P=0.030).
Discussion
Our study investigated pedestrian mask use and
public perceptions of community masking during
the initial spread of COVID-19 in Hong Kong. The
masking rate was high, and the public was confident
in mask efficacy for protection and the prevention
of community spread. Most pedestrians wore a
surgical mask, but a small proportion of these masks
were worn incorrectly. Surprisingly, the mask reuse
rate was high, and varying methods were used
for storage. Although government websites were
considered reliable, social media was more popular
as the source of information regarding masking and
health-related matters.
Face mask use in Hong Kong: general
perceptions and behaviours
Population-level behavioural insights are essential
for coordinating an effective and coherent
infection control strategy.6 Previous events and
disease outbreaks have considerably influenced
the masking culture in Hong Kong. Similar to
covering up when coughing or sneezing, wearing a
mask in the community or workplace when unwell
became a part of recent social etiquette following
the SARS outbreak. During the SARS epidemic,
a public hospital became a source of community
spread, prompting the government to enforce and promote community protective behaviour
thereafter, particularly in public hospitals. These
efforts included strong recommendations for
hospital visitors to wear masks, as well as the
widespread availability of hand sanitisers in strategic
areas. Whilst evidence supporting these practices
remains controversial, these recommendations have
positively influenced the attitude and behaviour of
the general public towards mass masking and hand
hygiene for protection during disease outbreaks.
These events may explain the high voluntary
masking rate that we have recorded in this study. A
high masking rate was also previously noted during
the SARS outbreak in Hong Kong.2 3 Notably, face
masks are also commonly used to protect against
air pollution, particularly during hazy weather and
within high traffic areas.
The issue of community masking was
controversial particularly during the early stages
of the COVID-19 pandemic, such that conflicting
recommendations were issued by various health
authorities and public figures worldwide. At the
time of this study, the World Health Organization
recommended against community masking because
of insufficient evidence regarding its effectiveness,
the potential for a false sense of security, and the
stressed supply of surgical masks for hospital use.7
However, this stance on effectiveness should have
been considered in the context of clinical outcome
studies,8 which were based largely on the spread of
influenza and would not necessarily be applicable to
the spread of COVID-19. Furthermore, reports of
disease spread involving pre-symptomatic carriers
of COVID-19 were not considered.
Although the surgical mask was originally
designed for the protection of patients during
surgery, its role in reducing wound infection is not
fully established and has been contentious.9 The
rationale for masking later shifted to protection
for the wearer, although evidence to support this
perspective is equally tenuous.10 Under standardised
simulated conditions, laboratory studies have shown that surgical masks are effective in limiting both
inbound and outbound transmission of aerosol
particles.11 Thus, wearing a face mask will limit the
spread of droplets during coughing or sneezing from
both symptomatic and asymptomatic carriers; it will
also protect the mucosa of the nostrils and mouth of
the wearer from droplets and aerosols.12 Contrary to
the claims by the World Health Organization7 that
wearing a mask may create a false sense of security
leading to the abandonment of other protective
behaviours, voluntary mask use in crowded areas
was shown to encourage protective behaviour and
performance of hand hygiene.13 The high masking
rate in Hong Kong may be an intangible factor
that enabled indirect control of community spread
by preventing viral shedding from asymptomatic
carriers. Multiple clusters of infections have
occurred in locations with poor masking or social
distancing,14 15 suggesting that these measures are
important. Since April 2020, the World Health
16 has updated its guidelines to
recommend the use of non-medical masks among
the general public when there is a limited capacity to
implement other containment measures.
Errors, reuse, and storage
A substantial proportion of pedestrians (13.0%) wore
their surgical face masks incorrectly, which may have
limited the protective efficacy of these masks. Most
commonly, they were worn too low, ‘upside-down’
or ‘inside-out’. A surgical mask consists of an inner
water-absorbing layer and an outer water-repelling
filter, which are horizontally pleated to create rows
of gutters for expansion and to catch moisture. A
mask worn inside-out accumulates moisture on the
facial side, which is uncomfortable. This increases
the likelihood that users will touch and rub their
faces, leading to self-contamination or temporary
mask removal. Additionally, a mask worn inside-out
may trap droplets from surrounding people
within the outward-facing water-absorbing layer. A
mask worn too low on the face exposes the nostrils or mouth, which are mucosal surfaces vulnerable
to droplets and airborne contamination. Although
unlikely, this error may arise from semantics—the
Chinese term for ‘face mask’ literally means ‘mouth
cover’, which may have misled users into believing
that this type of coverage was its sole purpose. We
examined the packaging of various brands of surgical
masks sold locally and found that very few provided
instructions for correct use. Instructions were
previously considered unnecessary because surgical
masks were intended for use by HCSPs; however,
many users now are members of the general public.
Manufacturers are encouraged to provide clear
instructions on their packaging and print a symbol
on each mask to prevent users from wearing masks
inside-out.
We were alarmed by the high reuse rate of
disposable masks. Some reasons were obvious, such
as a supply shortage, compounded by panic buying
that leads to price inflation. However, the masking
rate might have been lower if the masks were not
reused. Many users were probably aware that the
masks should not be reused, but our findings should
serve as a ‘reality check’.17 Surprisingly, mask reuse
was more common among HCSPs; this may have
been related to greater confidence in their ability
to handle a potentially contaminated mask, as well
as the belief that the causative virus (severe acute
respiratory syndrome coronavirus 2) will degrade on
non-living surfaces over time.18 Although there is no
evidence of increased disease spread, the potential
for contamination from poor handling is obvious.
Various mask storage methods, such as within
tissue papers, in paper envelopes, in plastic bags,
and in containers, were described. Recent evidence
suggests that the severe acute respiratory syndrome
coronavirus 2, which causes COVID-19, is more
stable on smooth non-porous surfaces; thus, it may
be safer to store masks in paper material (eg, tissues
or envelopes) where it will dry effectively.18 19 It has
also been reported that the virus can be inactivated
at 70°C in approximately 5 to 30 minutes.18 20 This
information will be useful should the reuse of
surgical masks be necessary during an exceptional
shortage; moreover, input from infectious disease
experts on the appropriate handling techniques is
likely to provide considerable value. Recently, Hong
Kong residents were issued reusable face masks with
antimicrobial properties for community use.19 21
Despite the high cost of such masks, this may be
the solution to face mask shortage issues; it may
also preserve medical face masks for hospital use, as
recommended by the World Health Organization.16
Sources of information regarding face masks
Social media was the most common source of health
information but was regarded as the least reliable
source. Although official government websites were regarded as the most reliable sources, many
respondents chose convenience over perceived
reliability when sourcing health information.
However, the potential for misinformation is an
important concern and conflicting advice may create
distrust, thereby interfering with the establishment
of a coherent response to the pandemic. Because
of the popularity of social media, authorities
should utilise these platforms as a supplement to
their standard websites for better public exposure
and communication concerning health-related
information. There is a clear need to address the
issues that we have identified. Correct masking
technique will reduce wastage and prevent self-contamination
through mishandling.
Limitations
There were several limitations to this study. First,
because of its observational nature, we were unable
to determine why some pedestrians did not wear
masks (eg, whether this was related to availability
or choice). Second, our findings may not be
sufficiently representative of other less crowded
areas in Hong Kong. Third, the respondents to our
online survey were limited to those with internet
access, which might have prevented inclusion of
individuals who were older, less educated, or more
vulnerable. Telephone and face-to-face interviews
may provide sufficient data concerning older people
and individuals with low socio-economic status.
Lastly, we did not identify the respondents of our
survey; thus, multiple responses could have been
submitted by some users. Nevertheless, this is the
largest behavioural study thus far to explore some of
the issues on the use of face masks during the initial
spread of COVID-19 in Hong Kong.
Conclusion
This study provided behavioural insights and
attitudes on community masking in a region that has
successfully managed the initial spread of COVID-19 through a combination of public health and
behavioural interventions. Members of the Hong
Kong population are highly motivated to engage in
masking practices and believe in its effectiveness
for protection and the prevention of disease spread.
However, a high face mask reuse rate and incorrect
masking techniques were observed. Information on
government websites should be enhanced and linked
to social media to improve accessibility and provide
suitable guidance for the general public.
Author contributions
Concept or design: VCW Tam, CPL Chan, HKW Law, SWY Lee.
Acquisition of data: VCW Tam, HKW Law, SWY Lee.
Analysis or interpretation of data: VCW Tam, SWY Lee.
Drafting of the manuscript: VCW Tam, SY Tam, ML Khaw, SWY Lee.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: VCW Tam, HKW Law, SWY Lee.
Analysis or interpretation of data: VCW Tam, SWY Lee.
Drafting of the manuscript: VCW Tam, SY Tam, ML Khaw, SWY Lee.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
We thank Miss Abbie Chan, Department of Health Technology
and Informatics, The Hong Kong Polytechnic University, for
her assistance in data collection throughout the study; Mr Alex
Nicol for his professional advice with manuscript preparation
and statistical analysis; and Dr Wai-kwong Poon for his expert
advice with research design and manuscript revision.
Declaration
A letter reporting preliminary findings of part of the present
study was published in Tam VC, Tam SY, Poon WK, Law
HK, Lee SW. A reality check on the use of face masks during
the COVID-19 outbreak in Hong Kong. EClinicalMedicine.
2020 Apr 24;22:100356. https://doi.org/10.1016/j.eclinm.2020.100356
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study was approved by the Human Subjects Ethics Application Review Board of Hong Kong Polytechnic
University (Ref HSEARS20200213002-01). Participation
in the survey was voluntary, and consent was implied from
completion of the survey.
References
1. Cowling BJ, Ali ST, Ng TW, et al. Impact assessment of
non-pharmaceutical interventions against coronavirus
disease 2019 and influenza in Hong Kong: an observational
study. Lancet Public Health 2020;5:e279-88. Crossref
2. Cheng KK, Lam TH, Leung CC. Wearing face masks in the
community during the COVID-19 pandemic: altruism and
solidarity. Lancet 2020 Apr 16. Epub ahead of print. Crossref
3. Leung GM, Quah S, Ho LM, et al. A tale of two cities:
community psychobehavioral surveillance and related
impact on outbreak control in Hong Kong and Singapore
during the severe acute respiratory syndrome epidemic.
Infect Control Hosp Epidemiol 2004;25:1033-41. Crossref
4. Tang CS, Wong CY. Factors influencing the wearing
of facemasks to prevent the severe acute respiratory
syndrome among adult Chinese in Hong Kong. Prev Med
2004;39:1187-93. Crossref
5. Centre for Health Protection, Department of Health,
Hong Kong SAR Government. Use mask properly. 2015. Available from: https://www.chp.gov.hk/files/pdf/use_mask_properly.pdf. Accessed 12 Aug 2020.
6. Sadique MZ, Edmunds WJ, Smith RD, et al. Precautionary
behavior in response to perceived threat of pandemic
influenza. Emerg Infect Dis 2007;13:1307-13. Crossref
7. World Health Organization. Advice on the use of masks
in the context of COVID-19: interim guidance. 5 June
2020. Available from: https://apps.who.int/iris/bitstream/handle/10665/332293/WHO-2019-nCov-IPC_Masks-2020.4-eng.pdf. Accessed 5 Jun 2020.
8. Orr NW. Is a mask necessary in the operating theatre? Ann
R Coll Surg Engl 1981;63:390-2.
9. Romney MG. Surgical face masks in the operating theatre: re-examining the evidence. J Hosp Infect 2001;47:251-6. Crossref
10. Lipp A. The effectiveness of surgical face masks: what the literature shows. Nurs Times 2003;99:22-4.
11. van der Sande M, Teunis P, Sabel R. Professional and home-made
face masks reduce exposure to respiratory infections
among the general population. PloS One 2008;3:e2618. Crossref
12. Leung NH, Chu DK, Shiu EY, et al. Respiratory virus
shedding in exhaled breath and efficacy of face masks. Nat
Med 2020;26:676-80. Crossref
13. Wada K, Oka-Ezoe K, Smith DR. Wearing face masks
in public during the influenza season may reflect other
positive hygiene practices in Japan. BMC Public Health
2012;12:1065. Crossref
14. Centre for Health Protection, Department of Health, Hong
Kong SAR Government. CHP investigates 10 additional
cases of novel coronavirus infection. 2020. Updated 9
Feb 2020. Available from: https://www.info.gov.hk/gia/general/202002/09/P2020020900704p.htm. Accessed 20
Mar 2020.
15. Centre for Health Protection, Department of Health, Hong
Kong SAR Government. CHP investigates 43 additional
cases of COVID-19. 2020. Updated 26 Mar 2020. Available
from: https://www.info.gov.hk/gia/general/202003/26/P2020032600765p.htm. Accessed 10 Apr 2020.
16. World Health Organization. Advice on the use of masks
in the community, during home care and in health care
settings in the context of the novel coronavirus (2019-nCoV)
outbreak: interim guidance, 29 January 2020. Available
from: https://apps.who.int/iris/handle/10665/330987. Accessed 17 Aug 2020.
17. Tam VC, Tam SY, Poon WK, Law HK, Lee SW. A
reality check on the use of face masks during the
COVID-19 outbreak in Hong Kong. EClinicalMedicine
2020;22:100356. Crossref
18. Chin AW, Chu JT, Perera MR, et al. Stability of SARS-CoV-2
in different environmental conditions. Lancet Microbe
2020;1:e10. Crossref
19. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol
and surface stability of SARS-CoV-2 as compared with
SARS-CoV-1. N Engl J Med 2020;382:1564-7. Crossref
20. Nathan N. Waste not, want not: re-usability of N95 masks. Anesth Analg 2020;131:3. Crossref
21. Hong Kong SAR Government. Government to distribute
free reusable masks to all citizens. 2020. Updated 5 May
2020. Available from: https://www.info.gov.hk/gia/general/202005/05/P2020050500692.htm. Accessed 3 Aug
2020.