Hong Kong Med J 2021 Feb;27(1):70–2 | Epub 2 Feb 2021
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
COMMENTARY
COVID-19 primary care response and challenges
in Singapore: a tale of two curves
Y Liow, MB, BS, MMed1,2; Victor WK Loh, MMed, MHPE2; LH Goh, MB, BS, MMed2; David HY Tan, MB, BS, MMed1,2 TL Tan, FRCPE, FCFPS2,3; CK Leong, MMed, FAMS2,4; Doris YL Young, MB, BS, MD2
1 National University Polyclinics, National University Health System, Singapore
2 Division of Family Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
3 The Edinburgh Clinic, Singapore
4 Mission Medical Clinic, Singapore
Corresponding author: Dr Y Liow (yiyang_liow@nuhs.edu.sg)
Introduction
As global cities with comparable healthcare systems
and shared experience of the 2003 Severe Acute
Respiratory Syndrome outbreak, Hong Kong
and Singapore have had contrasting fortunes in
flattening their respective coronavirus disease
2019 (COVID-19) epidemic curves. Both reported
their first cases 1 day apart in late January 2020 and
quickly implemented border entry restrictions and
quarantine orders to limit imported cases. Hong
Kong adopted other aggressive interventions such as
school closures,1 whereas Singapore opted for a more
measured initial approach that included advising
only those unwell to wear face masks.2 Hong Kong
flattened its curve by the end of March; despite early
success, Singapore grappled with the emergence of
two distinct curves: one representing the Singapore community population and another representing the
migrant worker dormitory population (Fig3). This
commentary presents the duality of the COVID-19
situation in Singapore and discusses the related
primary care response and challenges.
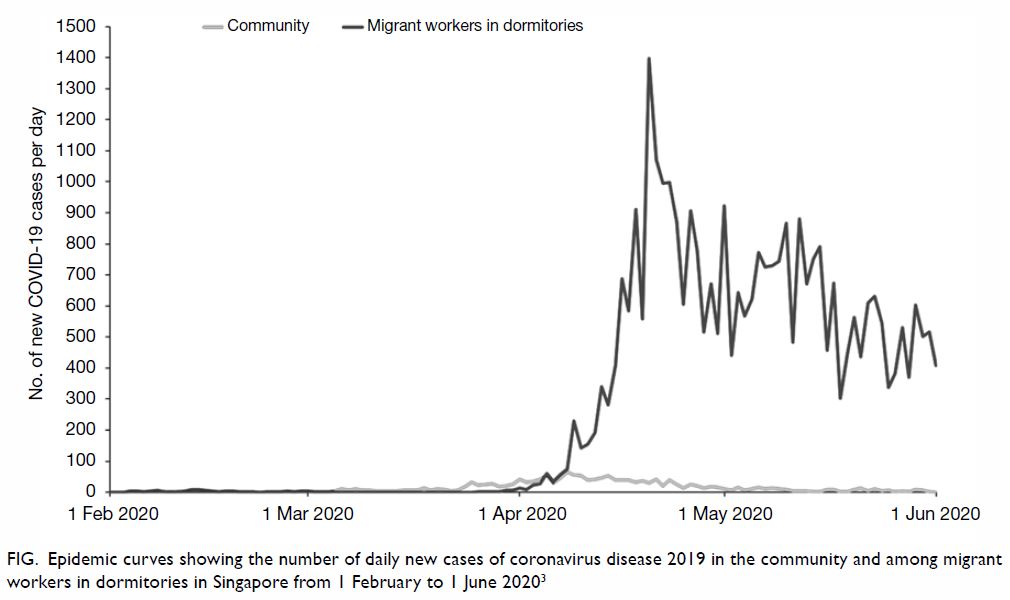
Figure. Epidemic curves showing the number of daily new cases of coronavirus disease 2019 in the community and among migrant workers in dormitories in Singapore from 1 February to 1 June 20203
Primary care in Singapore
Located in Southeast Asia, Singapore is an island
city-state with a population of more than 5.7 million.
Primary care forms the foundation of its healthcare
system. Similar to Hong Kong, the majority (about
80%) of primary care services are provided by 1700
privately run clinics, which range from sole proprietor
to large group practices. The remaining demand
is met by 20 community-based healthcare centres
known as ‘polyclinics’, which are similar to General
Outpatient Clinics in Hong Kong. These operate with government subvention to provide subsidised care
based on citizenship status.4 Whereas the private
sector handles almost 90% of acute visits, polyclinics
see more than 40% of chronic disease attendances.5
Community curve
When local transmission was detected in Singapore in
early February 2020, authorities activated the Public
Health Preparedness Clinics (PHPC), an island-wide
network of more than 900 primary care clinics and
polyclinics. Patients with acute respiratory symptoms
received subsidised treatments at these clinics, which
increased accessibility to care. This resulted in more
than 70% of confirmed cases visiting a clinic within
2 days of symptom onset.6 Those who met suspect
case criteria were tested under the ‘Swab-and-Send-Home’ (SASH) programme. The SASH facilitated out-patient
management, increased testing capacity, and
reduced the burden on tertiary centres. The network
also served an epidemiological role by gathering data
on community transmission including performing
sentinel surveillance swabs. Together with other
public health measures and the ‘circuit breaker’,
which was an enhanced set of social distancing
measures introduced by the Singapore Government
in early April including closure of schools and non-essential
workplaces, the PHPC helped to flatten the
community curve by end May 2020.7
The immediate challenge faced by primary care
physicians from the PHPC was introducing infection
control measures, including creating segregation
protocols and well-ventilated isolation areas. These
were operational challenges, particularly for smaller
practices with limited resources. A global shortage
of personal protective equipment also meant that
clinics had to ration supplies. Keeping abreast of new
advisories and workflows was another challenge. For
instance, SASH was initially restricted to patients
with clinical or radiological features of community-acquired
pneumonia. However, as evidence emerged
of pre-symptomatic transmission8 and mild disease
in the early stages, the SASH criteria were expanded
accordingly. At activated PHPC centres, physicians
encountered patients who had visited other clinics
and had not improved. More than 20% of the first
160 confirmed cases visited more than one clinic.9
‘Doctor hopping’ disrupted continuity of care
and risked cross contamination between clinics.
Proper messaging through mainstream and social
media channels helped reduce such behaviour.10 As
COVID-19 emerged, cases of dengue fever, which is
endemic in Singapore, were at a 4-year high.11 Both
viral infections have significant overlap in clinical and
laboratory features.6 Primary care physicians had to
be mindful of this dual outbreak as well as ‘covert’
COVID-19 masquerading as false-positive dengue
serology.12
Migrant worker dormitory curve
Originating mainly from India, Bangladesh, and
China, migrant workers in Singapore are employed in
industries such as construction and manufacturing.
There are about 323 000 residing in close proximity
to each other in 43 purpose-built dormitories.13
Worksites often engage workers living in different
dormitories and hence a single case can lead to
multiple clusters. Despite precautions taken to
restrict socialisation, more than 35 000 such workers
have been infected. Outposts in dormitories were
erected to screen workers and meet their medical
needs. Facilities island-wide including hotels and
exhibition centres were converted to isolation centres
to house those affected. Primary care physicians, who
are trained to provide care across multiple settings in
the community, were mobilised to these sites. Many
from public and private sectors, as well as locum and
retired practitioners, volunteered their efforts. Some
brought essential experience, having previously cared
for migrant workers as designated workplace doctors
or practising in industrial areas and non-profit clinics
catered to migrant workers.
One of the first challenges faced by primary
care physicians delivering care on-site was the
language barrier. Many workers spoke little or no
English, the working language of Singapore, which
impaired communication. Physicians overcame this
through visual aids, translators, and smartphone
applications.14 Although the majority of workers
are young and healthy, some are middle-aged with
chronic conditions such as hypertension and diabetes
mellitus. Some were being managed by physicians in
their home countries with care invariably affected by
disruption due to the pandemic. These conditions
had to be managed carefully with given resources.
The workers’ mental health also had to be monitored
closely with concerns of ‘cabin fever’ from prolonged
isolation progressing to more serious depressive and
anxiety disorders. New cases are still being recorded
daily and with authorities’ plans to test every worker,
primary care physicians will continue playing an
important role in flattening this curve.15
Conclusion
Singapore’s tale of two curves has important lessons.
Firstly, containment and mitigation strategies are
effective in flattening COVID-19 epidemic curves.16
As borders and economies reopen, measures with
the most benefit and least cost to society may need
reinstating. Secondly, accessible and coordinated
primary care continues to be a key arm of the
response to public health emergencies. Authorities
must continue to engage physicians and other
stakeholders regularly and should do so even during
‘peace time’. Lastly, every precaution must be taken to protect groups who live communally, such as migrant
workers. Singapore must look again at how these
workers are housed. The magnitude of the dormitory
curve should be a stark warning to other nations with
similar groups.
Author contributions
Concept or design: Y Liow, WKV Loh, DYL Young.
Acquisition of data: Y Liow.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: Y Liow.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: All authors.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgement
The authors would like to thank Ms Monica Ashwini Lazarus, Department of Family Medicine, Yong Loo Lin School of
Medicine, National University of Singapore, for editing a draft
of this manuscript.
Funding/support
The authors received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors, in relation to this commentary.
References
1. Cowling BJ, Ali ST, Ng TW, et al. Impact assessment of
non-pharmaceutical interventions against coronavirus
disease 2019 and influenza in Hong Kong: an observational
study. Lancet Public Health 2020;5:e279-88. Crossref
2. Goh T. Wuhan virus: Masks should be used only by those
who are unwell. The Straits Times. 31 Jan 2020. Available
form: https://www.straitstimes.com/singapore/health/masks-should-be-used-only-by-those-who-are-unwell.Accessed 31 Jan 2020.
3. Ministry of Health, Singapore Government. COVID-19
interactive situation report. 2020. Available from: https://www.moh.gov.sg/covid-19/situation-report. Accessed 9
Jun 2020.
4. Ministry of Health, Singapore Government. Primary
healthcare services. 2018. Available from: https://www.moh.gov.sg/home/our-healthcare-system/healthcare-services-and-facilities/primary-healthcare-services. Accessed 9 Jun 2020.
5. Ministry of Health, Singapore Government. Primary Care
Survey 2014 Report. Available from: https://www.moh.gov.sg/resources-statistics/reports/primary-care-survey-2014-report. Accessed 8 Jun 2020.
6. Lam LT, Chua YX, Tan DH. Roles and challenges of
primary care physicians facing a dual outbreak of
COVID-19 and dengue in Singapore. Fam Pract
2020;37:578-9. Crossref
7. Ministry of Health, Singapore Government. Circuit
breaker to minimise further spread of COVID-19. 3 Apr
2020. Available from: https://www.moh.gov.sg/news-highlights/details/circuit-breaker-to-minimise-further-spread-of-covid-19. Accessed 9 Jun 2020.
8. Wei WE, Li Z, Chiew CJ, Yong SE, Toh MP, Lee VJ. Presymptomatic transmission of SARS-CoV-2–Singapore,
January 23-Mar 16, 2020. MMWR Morb Mortal Wkly Rep
2020;69:411-5. Crossref
9. Singapore Government. COVID-19 spread caused by
socially irresponsible behaviour. 11 Mar 2020. Available from: https://www.gov.sg/article/covid-19-spread-caused-by-socially-irresponsible-behaviour. Accessed 9 Jun 2020.
10. Singapore Government. Steps to take when you’re unwell.
23 Mar 2020. Available from: https://www.gov.sg/article/steps-to-take-when-youre-unwell. Accessed 9 Jun 2020.
11. Ng JS. Dengue cases at four-year high. Today Online.
Available from: https://www.todayonline.com/singapore/dengue-cases-four-year-high. Updated 12 Feb 2020. Accessed 11 Feb 2020.
12. Yan G, Lee CK, Lam LT, et al. Covert COVID-19 and falsepositive
dengue serology in Singapore. Lancet Infect Dis
2020;20:536. Crossref
13. Ministry of Manpower, Singapore Government. List
of foreign worker dormitories. 2020. Available from:
https://www.mom.gov.sg/passes-and-permits/work-permit-
for-foreign-worker/housing/foreign-workerdormitories#/?page=1&q. Accessed 9 Jun 2020.
14. Yip C. ‘Your website will save lives’: NUS graduate builds
translation portal for medical teams treating migrant
workers. Channel News Asia: International Edition.
CNA Insider. 17 Apr 2020. Available from: https://www.channelnewsasia.com/news/cnainsider/covid-19-nus-medical-graduate-bengali-translators-workers-12650406.Accessed 17 Apr 2020.
15. Sin Y. All foreign workers in dorms to be tested for
Covid-19. The Straits Times. 13 May 2020. Coronavirus
pandemic. Available from: https://www.straitstimes.com/singapore/all-foreign-workers-in-dorms-to-be-tested-for-covid-19. Accessed 13 May 2020.
16. Walensky RP, Del Rio C. From mitigation to containment
of the COVID-19 pandemic: putting the SARS-CoV-2
genie back in the bottle. JAMA 2020;323:1889-90. Crossref

