Hong
Kong Med J 2020 Dec;26(6):538.e1–3
Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Progressive diaphyseal dysplasia: a rare bone
disorder with alarming radiographs
Moses ML Li, MB, ChB, MHKICBSC1; KY Chung, FRCSEd (Orth), FHKAM (Orthopaedic Surgery)1; Alex WH Ng, FRCR, FHKAM (Radiology)2; KH Chiu, FRCS, FHKAM (Orthopaedic Surgery)1
1 Department of Orthopaedics and Traumatology, Prince of Wales Hospital, Hong Kong
2 Department of Imaging and Interventional Radiology, Prince of Wales Hospital, Hong Kong
Corresponding author: Dr Moses ML Li (moseslml@gmail.com)
In March 2017, a 57-year-old man was referred
to our unit for left knee pain after a sprain, which
resolved upon conservative treatment. Plain
radiographs of the knees revealed diffuse sclerosis
of bilateral femurs and tibias. A detailed history
was sought to investigate the alarming skeletal
pathology revealed on the plain radiographs. The
patient had no history of bone pain, fever, weight
loss, nor other constitutional symptoms. There was
no history of malignancy. Physical examination
revealed negative findings in the musculoskeletal,
cardiac, pulmonary, renal, and neurological systems.
Alkaline phosphatase was elevated (176 IU/L) but
other blood parameters were normal, including
white cell count, C-reactive protein, erythrocyte
sedimentation rate, calcium, and phosphate. A
skeletal survey revealed widespread sclerosis of
tubular bone diaphysis of the lower extremities
(Fig 1), upper extremities (Fig 2), and skull (Fig 3).
Bone scintigraphy revealed increased osteoblastic
activity corresponding to the locations of sclerosis
(Fig 4). The characteristic radiographic features
with the clinical and laboratory findings favoured a
diagnosis of progressive diaphyseal dysplasia.
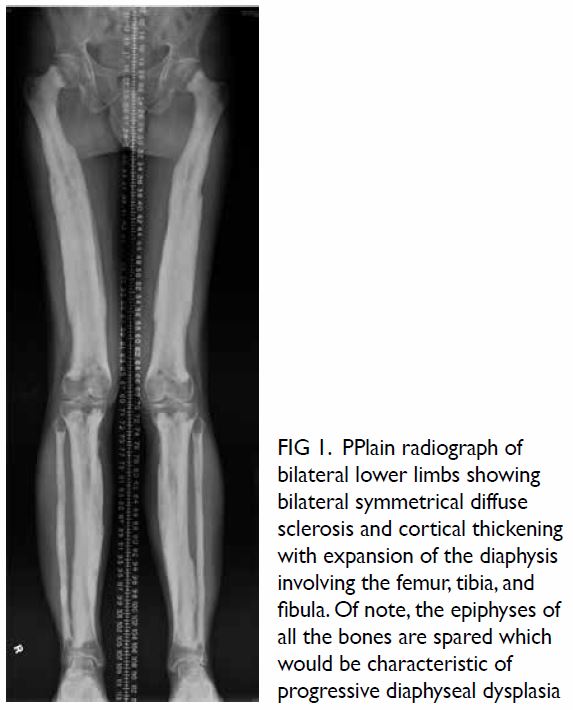
Figure 1. PPlain radiograph of bilateral lower limbs showing bilateral symmetrical diffuse sclerosis and cortical thickening with expansion of the diaphysis involving the femur, tibia, and fibula. Of note, the epiphyses of all the bones are spared which would be characteristic of progressive diaphyseal dysplasia
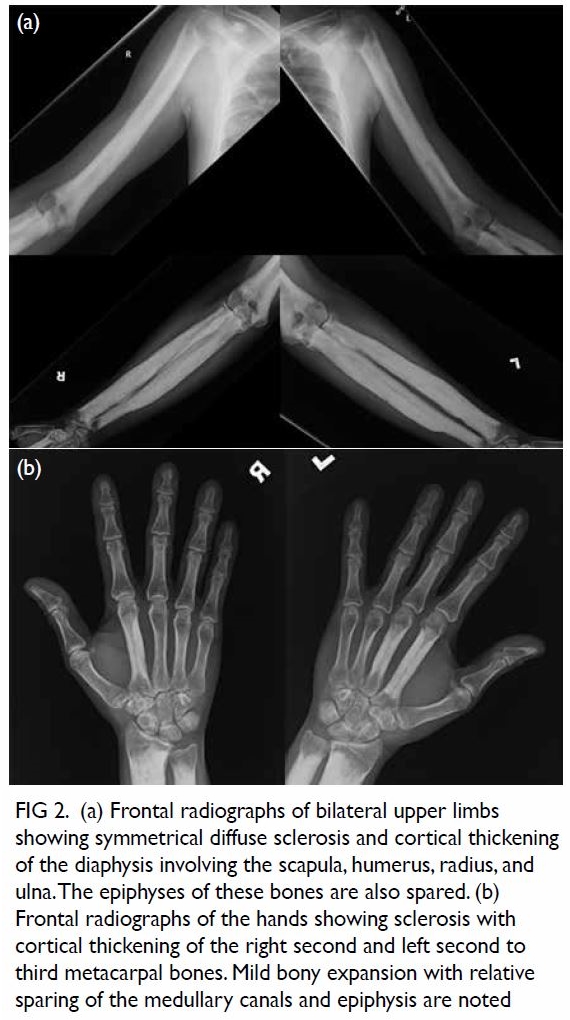
Figure 2. (a) Frontal radiographs of bilateral upper limbs showing symmetrical diffuse sclerosis and cortical thickening of the diaphysis involving the scapula, humerus, radius, and ulna. The epiphyses of these bones are also spared. (b) Frontal radiographs of the hands showing sclerosis with cortical thickening of the right second and left second to third metacarpal bones. Mild bony expansion with relative sparing of the medullary canals and epiphysis are noted
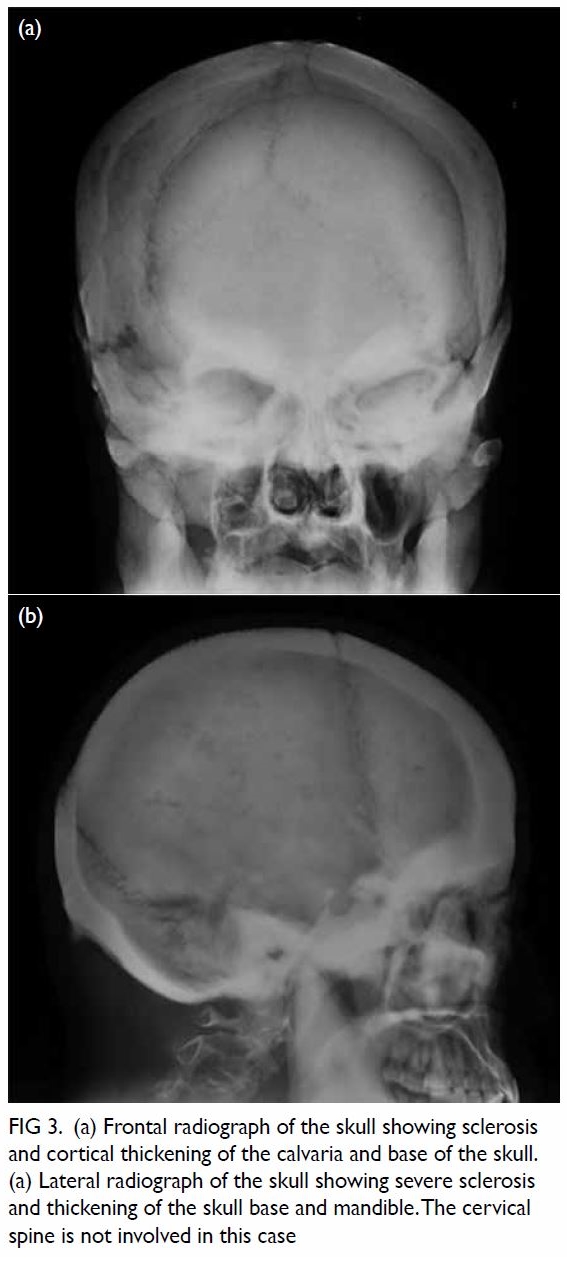
Figure 3. (a) Frontal radiograph of the skull showing sclerosis and cortical thickening of the calvaria and base of the skull. (a) Lateral radiograph of the skull showing severe sclerosis and thickening of the skull base and mandible. The cervical spine is not involved in this case
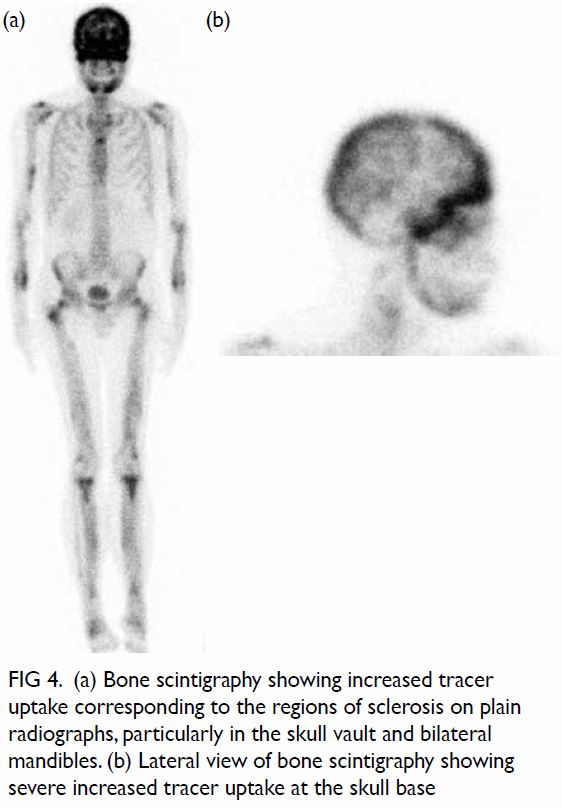
Figure 4. (a) Bone scintigraphy showing increased tracer uptake corresponding to the regions of sclerosis on plain radiographs, particularly in the skull vault and bilateral mandibles. (b) Lateral view of bone scintigraphy showing severe increased tracer uptake at the skull base
Sclerosing bone dysplasia is a heterogeneous group of rare bone disorders with pathognomonic
radiological features, caused by a defective ossification
pathway.1 2 Progressive diaphyseal dysplasia, also
known as Camurati-Engelmann disease, is a
disease belonging to this entity.3 4 5 It is an autosomal
dominant disorder due to mutation in transforming
growth factor–Β1. This in turn leads to a disorder
of intramembranous ossification, and results in
hyperostosis. Characteristic radiological features are
bilateral symmetrical fusiform sclerosis involving
the diaphyses of tubular bones. The epiphyses are
typically spared as these regions are formed by
endochondral ossification. The lower extremities
are more affected than the upper extremities. In
descending order of frequency, the tibia, femur, fibula, humerus, ulna, and radius are affected.3
Occasionally, the calvaria of the skull is involved.
The affected bones show uneven cortical thickening
of the diaphysis with hyperostosis extending in both
periosteal and endosteal directions. Hyperostosis
of the endosteal surface results in medullary canal
narrowing.
Clinical manifestations of progressive
diaphyseal dysplasia include limb pain, muscle
weakness, and easy fatigability. However, our patient
was completely asymptomatic. The disorder was
picked up incidentally during investigation of an
unrelated knee sprain. Detailed systemic review
revealed an absence of extraosseous manifestations of Erdheim-Chester disease that shares similar
radiological features.3 Ribbing disease (hereditary
multiple diaphyseal sclerosis) usually presents
with unilateral or asymmetrical involvement of
the bones, and does not involve the skull vault.
Osteopetrosis has epiphysis involvement and
usually presents with fracture and extramedullary
haematopoiesis. Although the differential diagnoses
for bone sclerosis are extensive, characteristic
radiographic distribution in association with clinical
and laboratory findings can substantially narrow the
possibilities and allow the diagnosis to be made. The
age at which the diagnosis of progressive diaphyseal
dysplasia is reached, the clinical manifestations of
disease and the extent of radiological evidence of
sclerosis are variable.4 5 Disease progression is slow
and unpredictable. Treatment of the disease aims
for symptomatic relief, with losartan reported
to be effective in relieving limb pain based on the
mechanism of down-regulation of transforming
growth factor–Β1 receptor expression.
Author contributions
All authors contributed to the concept of the study, acquisition
and analysis of the data, drafting of the manuscript, and
critical revision of the manuscript for important intellectual
content. All authors had full access to the data, contributed to
the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This pictorial medicine paper received no specific grant from any funding agency in the public, commercial, or not-for-profit
sectors.
Ethics approval
The patient was treated in accordance with the principles
outlined in the Declaration of Helsinki.
References
1. Boulet C, Madani H, Lenchik L, et al. Sclerosing bone
dysplasias: genetic, clinical and radiology update of
hereditary and non-hereditary disorders. Br J Radiol
2016;89:20150349. Crossref
2. Ihde LL, Forrester DM, Gottsegen CJ, et al. Sclerosing
bone dysplasias: review and differentiation from other
causes of osteosclerosis. Radiographics 2011;31:1865-82. Crossref
3. Uezato S, Dias G, Inada J, Valente M, Fernandes E. Imaging
aspects of Camurati-Engelmann disease. Rev Assoc Med
Bras (1992) 2016;62:825-7. Crossref
4. Van Hul W, Boudin E, Vanhoenacker FM, Mortier G.
Camurati-Engelmann disease. Calcif Tissue Int
2019;104:554-60. Crossref
5. Yuldashev AJ, Shin CH, Kim YS, et al. Orthopedic
manifestations of type I Camurati-Engelmann disease.
Clin Orthop Surg 2017;9:109-15. Crossref

