Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Traumatic epidural pneumorrhachis: a case
report
YY Yang, MB, BS1; CB Chua, MD1; CW Hsu, MD, PhD1,2; KH Lee, MD, PhD1,2
1 Department of Emergency Medicine, E-Da Hospital, I-Shou University, Kaohsiung, Taiwan
2 School of Medicine for International Students, I-Shou University, Kaohsiung, Taiwan
Corresponding author: Dr KH Lee (peter1055@gmail.com)
Case report
A 62-year-old man with no known systemic disease
was brought to an emergency department by
ambulance. He was found trapped in a car after
colliding with a bridge and was found to have been
driving under the influence of alcohol. On arrival,
he complained of headache, neck pain, and chest
pain. Physical examination revealed blood pressure
of 133/71 mm Hg, heart rate 71 beats per minute,
respiratory rate 22 breaths per minute, and oxygen
saturation on air of 93%. He appeared intoxicated
and was disorientated with a score of 13 (E3V4M6)
on the Glasgow Coma Scale. His pupil size was
3.5 mm with bilateral normal reaction to light.
A thorough neurological examination could not
be performed but the patient was able to move all
four limbs without limitation. Nonetheless a scalp
laceration, upper back tenderness and left lower
cervical crepitus were evident during palpation.
Chest examination revealed bilateral equal breath
sounds but some basal crackles and a left flank
abrasion about 3 × 4 cm in size. Haemogram and
biochemistry test results were within normal limits
but serum alcohol level was elevated at 2.48 g/L. Chest radiography revealed a posterior fracture at
the left fourth to sixth ribs and right ninth rib as well
as left cervical subcutaneous emphysema that raised
the suspicion of barotrauma associated with chest
trauma (Fig 1). In view of the possibility of barotrauma
and intracranial injuries, further evaluation with
computed tomography (CT) of the brain and chest
was arranged. The former was normal and the latter
confirmed right first to second posterior ribs and
left third to sixth posterior ribs fractures, as well as a
small left-sided pneumothorax, bilateral pulmonary
contusions, and pneumomediastinum. Notably, free
air accumulated in the posterior epidural spaces
of the cervical and thoracic spine as well as in the
left retrospinal and paraspinal muscle layers with
accompanying left second and third thoracic spine
posterior neural arch fracture in cervical spine CT
scan (Fig 2); these findings were compatible with
epidural pneumorrhachis. Additionally, air was
seen dissecting from the posterior neck into the
epidural space. A neurosurgeon recommended close observation rather than surgical intervention for
both the epidural pneumorrhachis and thoracic spine
fracture. The patient was admitted to the thoracic
surgical ward where he received conservative
therapy for rib fractures, pneumothorax and
pneumomediastinum including meperidine for pain
control and oxygen therapy via a nasal cannula at
3 L/min. New chest radiographs were taken on day 4
after surgery. Cervical emphysema had mostly
resolved but there was progression of pulmonary
contusion with bilateral minimal pleural effusions.
The patient also exhibited wheezing and dyspnoea
that warranted inhaled bronchodilators and systemic
steroid therapy. The patient was discharged on day
12 after surgery with symptom improvement; no
neurological sequelae were noted during follow-up
at the out-patient department.
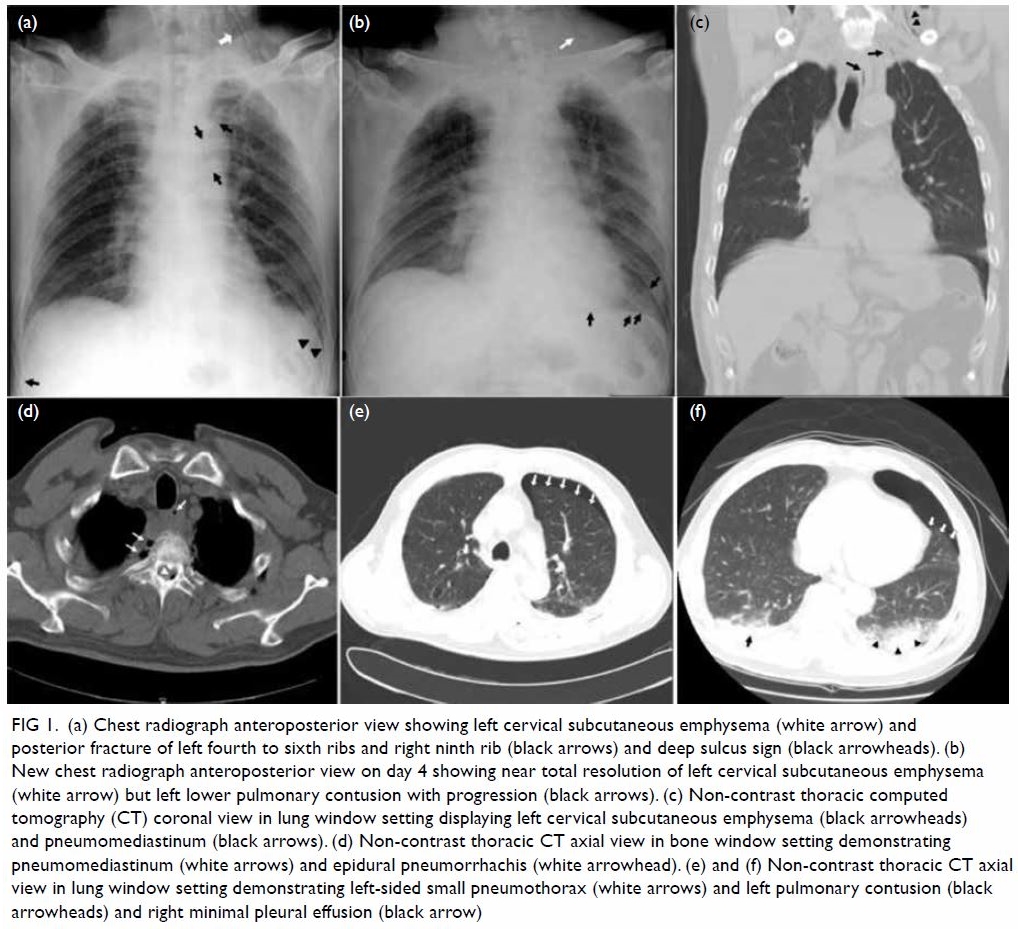
Figure 1. (a) Chest radiograph anteroposterior view showing left cervical subcutaneous emphysema (white arrow) and posterior fracture of left fourth to sixth ribs and right ninth rib (black arrows) and deep sulcus sign (black arrowheads). (b) New chest radiograph anteroposterior view on day 4 showing near total resolution of left cervical subcutaneous emphysema (white arrow) but left lower pulmonary contusion with progression (black arrows). (c) Non-contrast thoracic computed tomography (CT) coronal view in lung window setting displaying left cervical subcutaneous emphysema (black arrowheads) and pneumomediastinum (black arrows). (d) Non-contrast thoracic CT axial view in bone window setting demonstrating pneumomediastinum (white arrows) and epidural pneumorrhachis (white arrowhead). (e) and (f) Non-contrast thoracic CT axial view in lung window setting demonstrating left-sided small pneumothorax (white arrows) and left pulmonary contusion (black arrowheads) and right minimal pleural effusion (black arrow)

Figure 2. (a) Cervical spine computed tomography (CT) scan sagittal view in soft tissue window setting revealing air distributed in the epidural space (epidural pneumorrachis) at C-spine C3, C5 to C7 level (white arrows), posterior cervical subcutaneous emphysema (white arrowheads) and (black arrow) pointing out air dissecting from posterior neck into the epidural space; free air within the epidural space is located at the corner or peripherally. (b) Cervical spine CT scan sagittal view in bone window setting demonstrating epidural pneumorrhachis at C-spine C3 and C6 level (white arrows), posterior cervical subcutaneous emphysema (white arrowheads) and (black arrows) pointing out air dissecting from posterior neck into epidural space at the level of T2. (c) Cervical CT coronal view revealing epidural pneumorrhachis (white arrows), left cervical subcutaneous emphysema (white arrowheads) and pneumomediastinum (black arrow). (d) and (e) Cervical spine CT scan axial view at C3 level and C5 level in soft tissue window setting demonstrating epidural pneumorrhachis (white arrows) and air within the prevertebral layer of deep cervical fascia, especially in the paraspinal portion (white arrowheads). (f) Non-contrast thoracic CT coronal view in bone window setting showing air entry through the fractured neural arch of the left thoracic spine T2-3 resulting in epidural pneumorrhachis (white arrows)
Discussion
Pneumorrachis (PRS) is characterised by the
presence of air within the spinal canal and
can be classified according to its location as
subarachnoid or epidural PRS. Each is associated
with different pathophysiological mechanisms
and causes. It may result non-traumatically from
spinal degeneration, gas-producing infections,
or spontaneous pneumomediastinum in patients
with asthma. Iatrogenic PRS may occur following
a surgical procedure, epidural anaesthesia, or
lumbar puncture but PRS following trauma is rare.1
Almost all types of PRS are found in association
with air distribution in other compartments and
cavities of the body. For example, PRS is observed in
conjunction with pneumocephalus, pneumothorax,
pneumomediastinum, pneumopericardium, or
subcutaneous emphysema. Pneumorrachis following
trauma is rare and arises from the presence of air
in the posterior mediastinum or retropharyngeal
space dissecting along the fascial planes from the
posterior mediastinum or retropharyngeal space
through the neural foramina into the epidural space
under the driving pressure of a pneumothorax and
pneumomediastinum and low resistance of loose
connective tissue.2
Epidural PRS has been reported to occur most commonly secondary to traumatic
pneumomediastinum. Neurological deficits have
not been reported in epidural PRS secondary to
trauma. In contrast, traumatic subarachnoid PRS
is almost always secondary to major trauma and
skull bone fractures, and indicates severe injury
and possible association with complications
such as tension pneumocephalus or meningitis.3
Various neurological deficits, such as acute lumbar
root compression, chronic radiculopathy, and
cauda equina syndrome may occur. It is therefore
important to identify air in the epidural space and
subarachnoid space to enable prompt and adequate
management.4 The possible mechanism of PRS in our
patient was air entry into the epidural space because
of pneumomediastinum, left-sided pneumothorax
and subcutaneous emphysema extending through
the fractured neural arch of the thoracic spines into
the epidural space; these conditions fulfil the criteria
for benign traumatic PRS. Criteria for a diagnosis of benign traumatic epidural PRS include substantial
pneumomediastinum with extensive subcutaneous
emphysema due to thoracic trauma.4 There may also
be incidental findings of small amounts of epidural
air demonstrable only on CT and unrelated to spinal
trauma. “Benign” epidural PRS can be managed
conservatively with spontaneous resolution of
epidural air.4 Repeat or further neuroimaging studies
are not routinely provided in cases of epidural PRS,
provided there is no new or progressive neurological
deficit. Three cases have been reported with complete
resolution of PRS on follow-up CT scan after 4 to
14 days.5 6 7
The PRS is usually asymptomatic and an
accidental finding on CT images while evaluating
other severe or life-threatening torso injuries.
Although CT is the gold standard for diagnosis, it
is difficult to differentiate epidural and subarachnoid
PRS. Nonetheless in the former, air is collected at
the corner or peripherally unlike subarachnoid PRS where it is distributed more centrally in the canal
based on normal anatomy. Magnetic resonance
imaging or intrathecal contrast CT can distinguish
intradural from extradural air.7 In most cases of
epidural PRS, the air reabsorbs spontaneously
without recurrence and the patient can be managed
conservatively.1 In subarachnoid PRS, timely
consultation with a neurosurgeon for decompression
of nerve root injuries, tension pneumocephalus and
exploratory surgery by a chest surgeon to detect
severe thoracic trauma is vital. Impressively, Avci
et al5 reported a case of complete resolution of
subarachnoid PRS on the fifth day of admission
with recovery of neurological deficit after chest tube
insertion. They concluded that the negative pressure
of the chest drain to withdraw the air supported the
hypothesis of a one-way valve mechanism in which
high pressure air travels through fascial layers but
is unable to return. The routine use of antibiotic is not recommended in either type unless meningitis develops.1
Conclusion
Traumatic PRS is rare and an incidental radiological
finding. Epidural PRS is often self-limiting with a
good prognosis. Although most patients can be
managed conservatively, prompt recognition of
subarachnoid PRS with neurological deficits and
other concurrent life-threatening torso injuries is
vital.
Author contributions
Concept or design: KH Lee.
Acquisition of data: YY Yang.
Analysis or interpretation of data: CB Chua.
Drafting of the manuscript: YY Yang and KH Lee.
Critical revision of the manuscript for important intellectual content: CW Hsu.
Acquisition of data: YY Yang.
Analysis or interpretation of data: CB Chua.
Drafting of the manuscript: YY Yang and KH Lee.
Critical revision of the manuscript for important intellectual content: CW Hsu.
All authors had full access to the data, contributed to the
study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
We would like to extend our special thanks to Dr Cheng-yang
Lee, Department of Medical Imaging, Chi Mei Medical Center,
Tainan, Taiwan who provided insight and expertise on the
image interpretation that greatly improved our manuscript.
Funding/support
All authors have no commercial association, such as
consultancies, stock ownership or other equity interests or
patent-licensing arrangements.
Ethics approval
The patient was treated in accordance with the tenets of the Declaration of Helsinki. The patient provided written
informed consent for all treatments and procedures.
References
1. Oertel MF, Korinth MC, Reinges MH, Krings T, Terbeck S, Gilsbach JM. Pathogenesis, diagnosis and management of
pneumorrhachis. Eur Spine J 2006;15 Suppl 5:636-43. Crossref
2. Defouilloy C, Galy C, Lobjoie E, Strunski V, Ossart M. Epidurual pneumatosis: A benign complication of benign
pneumomediastinum. Eur Respir J 1995;8:1806-7. Crossref
3. Goh BK, Yeo AW. Traumatic pneumorrhachis. J Trauma
2005;58:875-9. Crossref
4. Willing SJ. Epidural pneumatosis: a benign entity in trauma patients. AJNR Am J Neuroradiol 1991;12:345.
5. Avci İ, Başkurt O, Şirinoğlu D, Aydin MV. Rapid
disappearance of pneumorrhachis after chest tube
placement. Turk J Emerg Med 2019;19:146-8. Crossref
6. Kim SW, Seo HJ. Symptomatic epidural pneumorrhachis: a rare entity. J Korean Neurosurg Soc 2013;54:65-7. Crossref
7. Pfeifle C, Henkelmann R, von der Höh N, et al. Traumatic pneumorrhachis. Injury 2020;51:267-70. Crossref

