Hong
Kong Med J 2020 Dec;26(6):479–85 | Epub 7 Dec 2020
Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Pre-hospital stroke screening and notification
of patients with reperfusion-eligible acute ischaemic stroke using modified Face Arm Speech Time test
William CY Leung, MB, BS1; Kay C Teo, MB, BS1; WM Kwok, MB, BS2, Lawrence HC Lam, MSc3; Olivia MY Choi, MPsych4; Mona MY Tse, MB, BS1; WM Lui, MB, BS4; TC Tsang, MB, BS2; Anderson CO Tsang, MB, BS4
1 Division of Neurology, Department of Medicine, Queen Mary Hospital, The University of Hong Kong, Hong Kong
2 Department of Accident and Emergency, Queen Mary Hospital, Hong Kong
3 Hong Kong Division, Ambulance Command, Hong Kong Fire Services Department, Hong Kong
4 Division of Neurosurgery, Department of Surgery, Queen Mary Hospital, The University of Hong Kong, Hong Kong
Corresponding author: Dr Anderson CO Tsang (acotsang@hku.hk)
Abstract
Objectives: To investigate the effects of pre-hospital
stroke screening and notification on reperfusion
therapy for patients with acute ischaemic stroke.
Methods: Pre-hospital stroke screening criteria
were established based on a modified version of
the Face Arm Speech Time (FAST) test. Screening
was performed during ambulance transport by
emergency medical service (EMS) personnel who
completed a 2-hour training session on stroke
screening. Temporal trends affecting acute ischaemic
stroke investigation and intervention were compared
before and after implementation of the pre-hospital
screening.
Results: From July 2018 to October 2019, 298 patients
with suspected stroke were screened by EMS
personnel during ambulance transport prior to
hospital arrival. Of these 298 patients, 213 fulfilled
the screening criteria, 166 were diagnosed with
acute stroke, and 32 received reperfusion therapy.
The onset-to-door time was shortened by more than
1.5 hours (100.6 min vs 197.6 min, P<0.001). The
door-to–computed tomography time (25.6 min vs
32.0 min, P=0.021), door-to-needle time (49.2 min
vs 70.1 min, P=0.003), and door-to–groin puncture
time for intra-arterial mechanical thrombectomy
(126.7 min vs 168.6 min, P=0.04) were significantly
shortened after implementation of the pre-hospital
screening and notification, compared with historical
control data of patients admitted from January 2018
to June 2018, before implementation of the screening system.
Conclusion: Implementation of pre-hospital stroke
screening using criteria based on a modified version of
the FAST test, together with pre-arrival notification,
significantly shortened the door-to-reperfusion
therapy time for patients with ischaemic stroke.
Pre-hospital stroke screening during ambulance
transport by EMS personnel who complete a 2-hour
focused training session is effective for identifying
reperfusion-eligible patients with stroke.
New knowledge added by this study
- Implementation of pre-hospital stroke screening using criteria based on a modified version of the FAST (Face Arm Speech Time) test, together with pre-arrival notification, significantly shortened the door-to-reperfusion therapy time for patients with acute ischaemic stroke.
- The onset-to-door time, door-to–computed tomography time, door-to-needle time, and door-to–groin puncture time for intra-arterial mechanical thrombectomy were all significantly shortened after implementation of the pre-hospital screening and notification, compared with historical control data.
- Pre-hospital stroke screening during ambulance transport by emergency medical service personnel who complete a 2-hour focused training session is effective for identifying patients with reperfusion-eligible stroke.
- The findings confirm the importance of pre-hospital notification in facilitating downstream management of patients with acute stroke by allowing the Accident and Emergency Department and stroke team to prepare for the patient’s arrival.
- Cost-effectiveness studies are needed to evaluate the impact and sustainability of the system on a territory-wide scale, which will aid in long-term infrastructure development in acute stroke care.
Introduction
Timely reperfusion for ischaemic stroke with
intravenous thrombolysis (IVT) or mechanical
thrombectomy can substantially improve patient
outcomes.1 Hence, all possible efforts should be made
to shorten the stroke onset-to-treatment time. The
major benchmark for measurement of acute stroke
treatment speed is the door-to-needle time, that
is, the duration between Accident and Emergency
Department (AED) arrival and administration of
IVT. Other benchmarks include duration between
AED arrival and brain computed tomography (door-to-CT time) and duration between AED arrival
and groin puncture for mechanical thrombectomy
(door-to–groin puncture time). The recommended
intervals are within 60 minutes for door-to-needle
time, 25 minutes for door-to-CT time, and
120 minutes for door-to–groin puncture time.
The American Heart Association/American
Stroke Association Target Stroke initiative supports
implementation of strategies to shorten the door-to-needle time. These include advance hospital
notification by emergency medical service (EMS)
personnel, rapid triage protocol in the AED, rapid
acquisition of brain imaging data, and a team-based
approach. These strategies were consolidated in the recent recommendation for establishing a system of
care for patients with stroke.2 3
Before 2018, there was no pre-hospital stroke
notification system in Hong Kong.4 Patients with
ischaemic stroke, including those who are within
the therapeutic window for reperfusion therapy,
are transferred to the nearest AED under the
regular triage system, which may delay reperfusion
treatment. Herein, we investigate the effects of a
team-based pre-hospital stroke notification system
designed to improve the delivery of acute stroke
care.
Methods
Pre-hospital stroke notification system
Our pre-hospital stroke notification system was
established in collaboration between the AED,
stroke neurologists, neurosurgeons, and the
ambulance service. This included an advance
hospital notification by EMS personnel, rapid
triage protocol, advance stroke team notification,
and image acquisition via CT. The EMS personnel
screened patients with suspected stroke using a
locally formulated pre-hospital stroke assessment
scale to identify reperfusion-eligible patients with
stroke. For patients who met all criteria, advance
hospital notification was activated by calling a
designated number in the AED; this call served to
alert the stroke team, triage station, and on-duty
AED medical officer. A CT scan was then arranged
by the AED medical officer in the next available
urgent slot.
Ambulance stroke assessment
Our simple pre-hospital stroke assessment in
Chinese was formulated on the basis of the Los
Angeles Pre-hospital Stroke Screen and the Face
drooping, Arm weakness, Speech difficulty, Time
to call 911 (FAST) screening criteria.5 6 In contrast
to the Los Angeles Pre-hospital Stroke Screen and
FAST criteria, we aimed to identify only patients
eligible for reperfusion therapy, in whom earlier
treatment would provide the greatest benefit. The
inclusion criteria were as follows: (1) ≤4 hours since
onset of symptoms, (2) sudden limb weakness or
speech impairment, (3) age >18 years, (4) stroke
unrelated to recent trauma, (5) Glasgow Coma Scale
score ≥8, (6) systolic blood pressure of >100 mm Hg,
(7) no history of seizures/epilepsy, and (8) absence
of previous wheelchair-bound or bed-ridden status.
Patients who satisfied all eight inclusion criteria
underwent a point-based Chinese FAST screening
(speech disturbance = 2 points; unilateral facial
drooping = 1 point; and unilateral limb weakness = 2 points). Advance hospital notification was
activated for eligible patients with ≥2 points in the
FAST screening.
Emergency medical service personnel
training
All EMS personnel within our hospital’s catchment
area attended a 2-hour stroke training session
delivered by a team of stroke neurologists,
neurosurgeons, and emergency physicians. This
included didactic instruction concerning stroke
subtypes, symptoms, reperfusion therapy pre-hospital
management, and hands-on training for
utilisation of the ambulance stroke assessment scale.
Patients
The pre-hospital stroke screening and notification
system was implemented on 1 July 2018. All patients
with acute stroke admitted via ambulance transfer
from July 2018 to October 2019 were prospectively
included in this study. Data were collected concerning
patient characteristics, stroke severity, and temporal
trends of stroke treatment. Patients admitted via the
AED whose admission had included acute stroke
diagnosis, during the period from January 2018
to June 2018 (6 months before implementation of
the pre-hospital stroke screening and notification
system), were retrospectively identified as historical
controls.
Statistical Analysis
Categorical variables were compared using Chi
squared analysis, while continuous variables were
compared using independent t tests and one-way
analysis of variance. Univariate analysis was initially
used on all variables; the results were recorded as
odds ratios with 95% confidence intervals. Kaplan–Meier curve and log rank test analyses of door-to-needle
time with and without notification were
performed. Statistical significance was set at P<0.05.
All analyses were performed using SPSS Statistics
for Windows, version 25.0 (IBM Corp, Armonk
[NY], United States).
Results
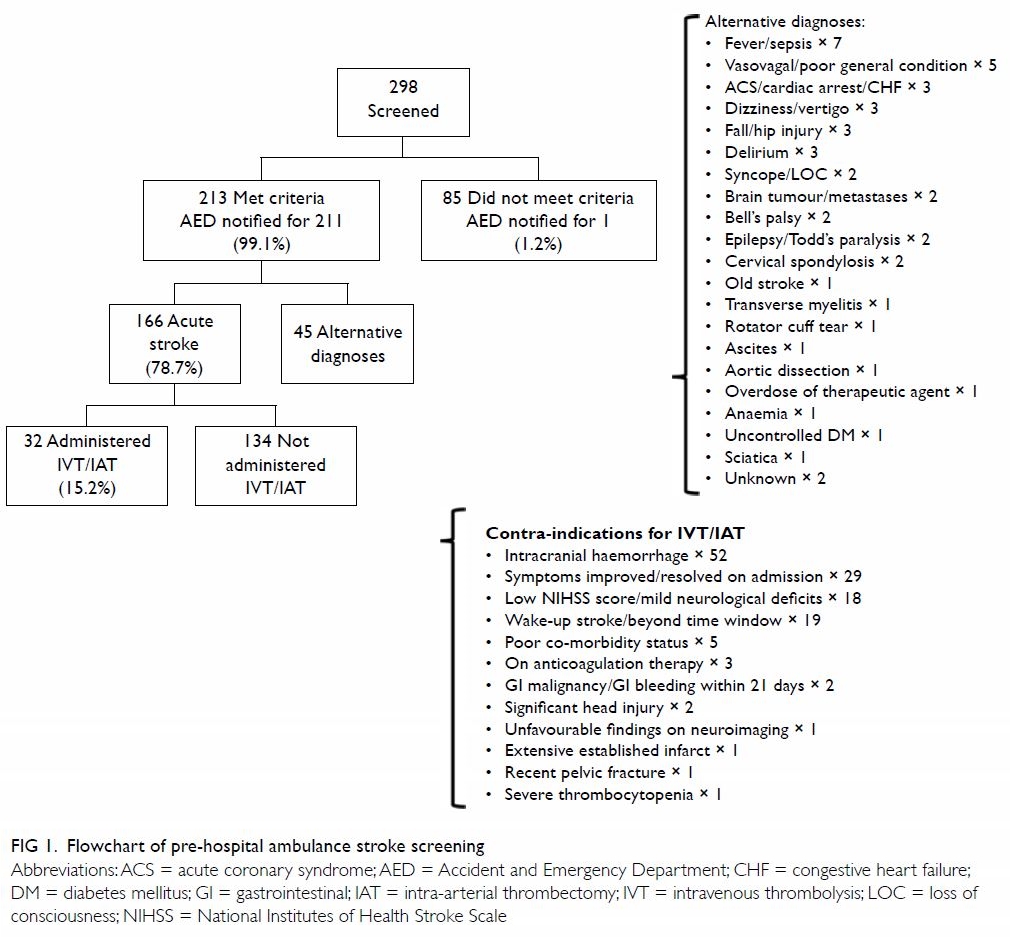
During the study period, 298 patients with suspected stroke were screened by the ambulance staff. Of
these 298 patients, 213 fulfilled the screening criteria
for pre-hospital notification; the AED was notified
for 211 (99.1%), in accordance with study protocol.
Among patients for whom the AED was notified,
166 (78.7%) were eventually diagnosed with acute
stroke. The final diagnoses of patients without stroke
included vasovagal syncope, fever/sepsis, and acute
coronary syndrome (Fig 1).
Among the 211 patients for whom pre-arrival
notification was performed, 32 (15.2%) received
reperfusion therapy (IVT and/or intra-arterial
endovascular thrombectomy [IAT]). Reperfusion
therapy was not administered to the remaining
134 patients for reasons such as intracranial haemorrhage, resolution of symptoms after arrival,
and mild neurological deficits. Among the 85 patients
who did not fulfil the screening criteria, one eventually
received thrombectomy. Stroke notification was not
performed for this patient due to uncertain time of
symptom onset.
We compared the temporal trends in provision
of acute stroke care after the implementation of
ambulance stroke screening with a historical cohort
from the period prior to implementation (Table 1).
The door-to-CT time (25.6 min vs 32.0 min, P=0.021),
door-to-needle time (49.2 min vs 70.1 min, P=0.003)
[Fig 2], and door-to–groin puncture time for IAT
(126.7 min vs 168.6 min, P=0.04) were significantly
shortened after implementation of the pre-hospital
stroke screening and notification system, compared
with the historical control cohort. The proportions
of patients who underwent CT within 25 minutes
(68.6% vs 51.6%, P=0.001) and groin puncture
within 120 minutes were also increased (72.3% vs
18.2%, P=0.008). Notably, the onset-to-door time
was shortened by more than 1.5 hours (100.6 min
vs 197.6 min, P<0.001) after implementation of our
system.
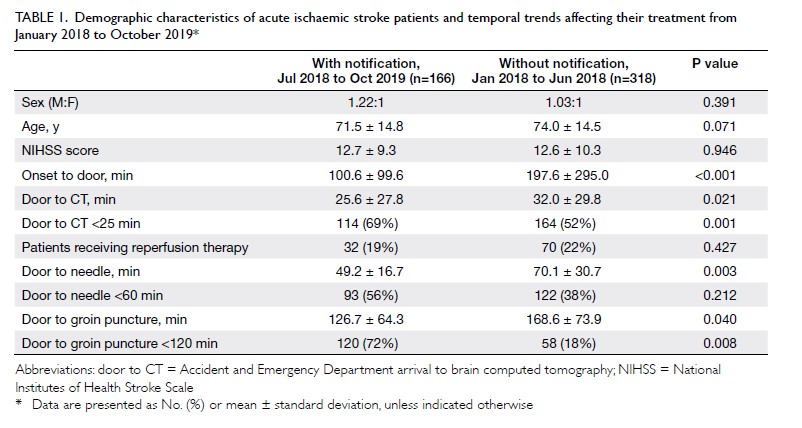
Table 1. Demographic characteristics of acute ischaemic stroke patients and temporal trends affecting their treatment from January 2018 to October 2019
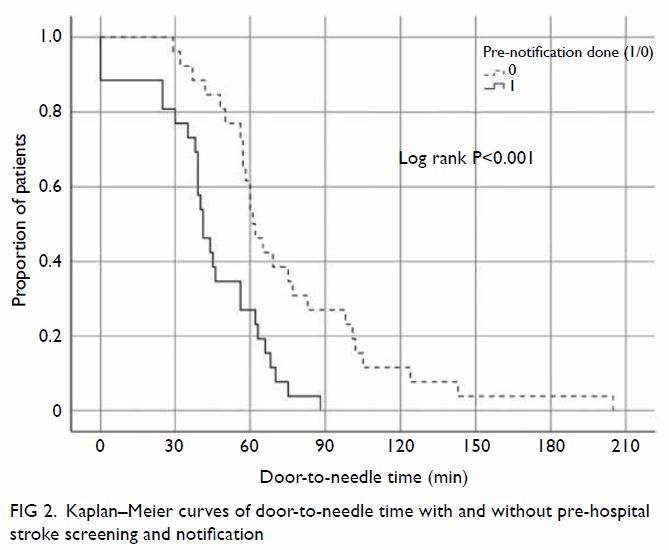
Figure 2. Kaplan–Meier curves of door-to-needle time with and without pre-hospital stroke screening and notification
Furthermore, we compared the temporal
trends in patients who received reperfusion therapy
(ie, IVT and IAT) during the study period between
patients who underwent pre-notification screening
and those who did not (Table 2). The door-to-needle
time was significantly reduced with pre-notification
screening (49.2 min vs 75.2 min, P=0.005). The door-to-CT time and door-to–groin puncture time also
tended to be shorter with pre-notification, although
these differences were not statistically significant.
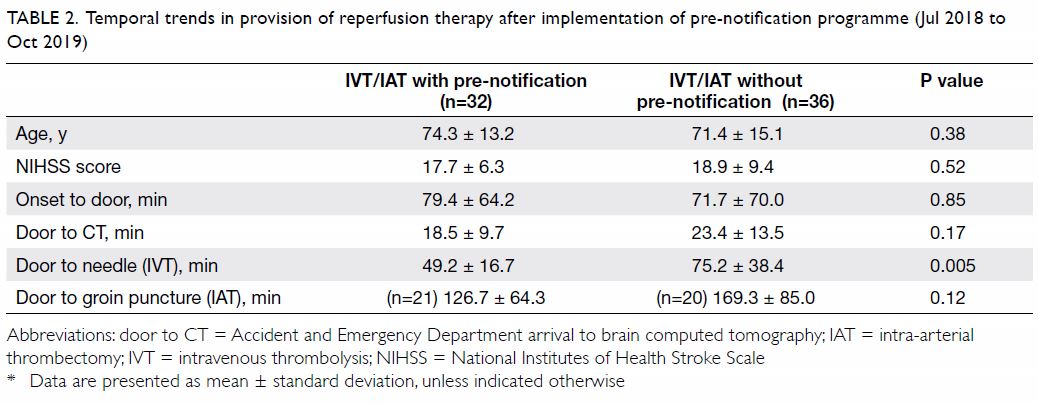
Table 2. Temporal trends in provision of reperfusion therapy after implementation of pre-notification programme (Jul 2018 to Oct 2019)
Discussion
The typical patient with stroke loses 1.9 million
neurons per minute while the stroke remains
untreated.7 Each minute saved between onset of
stroke and treatment grants 1.8 days of extra healthy
life.1 Timely reperfusion therapy with thrombolysis
or thrombectomy has been demonstrated to reduce
long-term disability when administered early to
eligible patients. Earlier thrombolysis also lowers
the risks of complications such as haemorrhagic
transformation.8 9 Our study demonstrated that the
implementation of a simple yet effective pre-hospital
screening notification system significantly shortened
time to diagnosis of acute stroke and subsequent
intervention. This confirms the importance of pre-hospital
notification in facilitating downstream
management of patients with acute stroke by
allowing the AED and stroke team to prepare for the
patient’s arrival in advance.
The efficiency of the acute stroke treatment
pathway was improved by the notification system
for the following reasons. First, early notification
by the ambulance team allowed the AED and stroke physicians to assess the patient’s medical history,
including their eligibility and contra-indications for
emergency reperfusion therapy, before patient arrival
at the hospital. Second, the triage process at the AED
was streamlined and patients with suspected stroke
could be prioritised and immediately attended by
the medical team. Moreover, the CT-suite staff
were alerted to ensure the availability of a CT scan
slot upon patient arrival. Third, the acute stroke
nurse was consulted early to standby for patient
arrival at the AED. Finally, the stroke alert created
a sense of urgency among all medical and allied
health professionals involved in stroke care, thereby
enhancing the speed of the entire care pathway. Our
experience is consistent with the reports from other
medical systems that have implemented stroke alert
systems to reduce door-to-needle time.10 11 12
Notably, the present study demonstrated that
the door-to–groin puncture time for thrombectomy
candidates was also markedly reduced by pre-arrival
notification, enabling the majority of patients to
undergo groin puncture within 120 minutes. This is
likely due to the longer time required to coordinate
the neurointerventionist, interventional suite,
and anaesthesiology care team; this process was
initiated early with pre-arrival stroke notification.
Consistent with our findings, pre-arrival notification
is now recommended for all patients with suspected
stroke, according to the 2019 guidelines of the
American Stroke Association.3 Future efforts should
focus on pre-hospital screening of thrombectomy-eligible
patients with large vessel occlusion and
establishment of a diversion system to ensure
patients are transported to thrombectomy-capable
hospitals.10
One concern related to pre-hospital stroke
screening was the potential for over-calling and
thus overloading the acute stroke treatment
pathway, thereby negatively affecting the AED
service for patients with non-stroke emergencies. To
maximise cost-effectiveness, the screening criteria were tailored to reduce notification for patients
with stroke mimics and to exclude patients who
were unlikely to benefit from acute reperfusion
therapy. The addition of criteria such as the time
of onset and pre-morbid functional status enabled
efficient detection of reperfusion-eligible patients
without excessively overloading the acute stroke
treatment pathway. These approaches are known to
prioritise patients with salvageable stroke for timely
reperfusion therapy and are especially relevant in
resource-limited public healthcare systems with
restricted capacity to expeditiously manage all
patients with stroke.13 As capacity improves, the
criteria can be modified to include patients with
delayed presentation after stroke onset.
Our study also validated the use of a Chinese
version of the FAST criteria for screening of patients
with suspected acute stroke. An important criticism
of the FAST criteria is that they are not universally
applicable in Chinese-speaking populations because
there is no direct translation of “Face Arm Speech
Time” to a memorable phase.14 15 In Hong Kong, the
FAST mnemonic has been modified to “談笑用兵”,
which is a well-recognised Chinese idiom where the
characters represent Speech, Smile (Face), Mobilise
(Arm), and Troop (Time to call for help). This version
has been promoted widely by local healthcare
professionals and stroke awareness organisations in
the past decade. This concise screening algorithm
is easily learned and rapidly performed, as reflected
by the high accuracy in stroke detection by our
ambulance staff after a 2-hour education session.
To the best of our knowledge, this is the first study
concerning the clinical utility of this modified
screening algorithm. Recently, Chinese versions
of similar scales, such as “Stroke 1-2-0” (China)
and “Stroke 112” (Taiwan), have been proposed
in other Chinese-speaking countries; each has
achieved satisfactory acceptance among healthcare
professionals.14 15 However, these scales have not
achieved widespread recognition by the general
populations of those countries. Improved versions
that aim to stratify large vessel occlusion strokes
(ie, BE-FAST) or a new score developed specifically
for use by ambulance staff may be introduced in the
future. Comparative studies of these different scales
and their applicability among Chinese-speaking
countries will provide useful information to unify
stroke awareness efforts across these populations.
Further cost-effectiveness studies to evaluate
the impact and sustainability of the system on a
territory-wide scale will be beneficial for long-term
infrastructure development in acute stroke care.
This study had some limitations. First, because
of logistical considerations, symptom onset time of
≤4 hours was used as a screening criterion. This was
established on the basis of the practical expected
times required to institute thrombolysis (30 min)
or coordinate thrombectomy (120 min) at the time
of study initiation. Because the time window for
thrombectomy has been expanded from 6 to 24 hours
in patients with favourable penumbra demonstrated
with CT perfusion imaging, the cut-off time of
symptom onset can be extended accordingly. Second,
EMS personnel may serve multiple catchment areas.
Hence, patients with stroke may be transported
by ambulances with EMS personnel who did not
undergo the additional training; these patients may
not be screened and hospitals may not be notified
before patient arrival. Third, clinical outcome data
were not consistently available for the historical
cohort, precluding analysis of clinical benefits due to
improved stroke treatment times. This issue might be resolved through territory-wide adoption of a
stroke screening protocol.
Conclusion
Implementation of pre-hospital stroke screening
using criteria based on a modified version of the
FAST test, together with pre-arrival notification,
significantly shortened the door-to-reperfusion
therapy time for patients with acute ischaemic stroke.
Pre-hospital stroke screening during ambulance
transport by EMS personnel who complete a 2-hour
focused training session is effective for identifying
reperfusion-eligible patients with stroke.
Author contributions
Concept or design: KC Teo, MMY Tse, WM Lui, TC Tsang, ACO Tsang.
Acquisition of data: WCY Leung, WM Kwok, LHC Lam, OMY Choi, ACO Tsang.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: WCY Leung, KC Teo, OMY Choi, ACO Tsang.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: WCY Leung, WM Kwok, LHC Lam, OMY Choi, ACO Tsang.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: WCY Leung, KC Teo, OMY Choi, ACO Tsang.
Critical revision of the manuscript for important intellectual content: All authors.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have no conflicts of interest to disclose.
Acknowledgement
We would like to acknowledge the ambulance staff of the Ambulance Command (Hong Kong Division), Fire Services
Department for the support in this project and in improving
stroke patient care in Hong Kong.
Funding/support
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The study was approved by The University of Hong Kong/Hospital Authority Hong Kong West Cluster Research Ethics
Committee (Ref UW20-442). The patients provided written
informed consent for all treatments and procedures.
References
1. Meretoja A, Keshtkaran M, Saver JL, et al. Stroke
thrombolysis: save a minute, save a day. Stroke
2014;45:1053-8. Crossref
2. Adeoye O, Nyström KV, Yavagal DR, et al.
Recommendations for the establishment of stroke systems
of care: a 2019 update. Stroke 2019;50:e187-210. Crossref
3. Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines
for the early management of patients with acute ischemic
stroke: 2019 update to the 2018 guidelines for the early
management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart
Association/American Stroke Association. Stroke
2019;50:e344-418. Crossref
4. Tsang AC, Yeung RW, Tse MM, Lee R, Lui WM. Emergency
thrombectomy for acute ischaemic stroke: current
evidence, international guidelines, and local clinical
practice. Hong Kong Med J 2018;24:73-80. Crossref
5. Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL.
Identifying stroke in the field. Prospective validation of
the Los Angeles prehospital stroke screen (LAPSS). Stroke
2000;31:71-6. Crossref
6. Harbison J, Hossain O, Jenkinson D, Davis J, Louw SJ,
Ford GA. Diagnostic accuracy of stroke referrals from
primary care, emergency room physicians, and ambulance
staff using the face arm speech test. Stroke 2003;34:71-6. Crossref
7. Saver JL. Time is brain—quantified. Stroke 2006;37:263-6. Crossref
8. Saver JL, Fonarow GC, Smith EE, et al. Time to treatment
with intravenous tissue plasminogen activator and outcome
from acute ischemic stroke. JAMA 2013;309:2480-8. Crossref
9. Lees KR, Bluhmki E, von Kummer R, et al. Time to
treatment with intravenous alteplase and outcome in
stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet 2010;375:1695-703. Crossref
10. Chiu YC, Tang SC, Sun JT, et al. Using G-FAST to
recognize emergent large vessel occlusion: a training
program for a prehospital bypass strategy. J Neurointerv
Surg 2020;12:104-8. Crossref
11. Tan BY, Ngiam NJ, Sunny S, et al. Improvement in door-to-needle time in patients with acute ischemic stroke via a simple stroke activation protocol. J Stroke Cerebrovasc Dis
2018;27:1539-45. Crossref
12. Zhang S, Zhang J, Zhang M, et al. Prehospital notification
procedure improves stroke outcome by shortening onset to
needle time in Chinese urban area. Aging Dis 2018;9:426-34. Crossref
13. Tsang AC, Yang IH, Orru E, et al. Overview of endovascular
thrombectomy accessibility gap for acute ischemic stroke
in Asia: a multi-national survey. Int J Stroke 2020;15:516-20. Crossref
14. Zhao J, Eckenhoff MF, Sun WZ, Liu R. Stroke 112: a
universal stroke awareness program to reduce language
and response barriers. Stroke 2018;49:1766-9. Crossref
15. Zhao J, Liu R. Stroke 1-2-0: a rapid response programme
for stroke in China. Lancet Neurol 2017;16:27-8. Crossref