Hong
Kong Med J 2020 Oct;26(5):450.e1–2
Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Skin testing for hypersensitivity and
cross-reactivity between proton pump inhibitors
Philip H Li, MRCP, FHKCP
Division of Rheumatology and Clinical Immunology, Department of Medicine, The University of Hong Kong, Queen Mary Hospital, Pokfulam, Hong Kong
Corresponding author: Dr Philip H Li (liphilip@hku.hk)
A 44-year-old woman presented to our anaphylaxis
clinic with first episode of anaphylaxis. She had
no known prior food or drug allergies. She was
previously prescribed esomeprazole 20 mg daily
as required for dyspepsia by her private physician,
but took it only very occasionally. Two months
previously she took one tablet of esomeprazole
(20 mg) and one of paracetamol (500 mg) together
with a slice of plain bread for abdominal discomfort
and influenza-like symptoms. Within 10 minutes,
she experienced generalised pruritus and collapsed
at home. She awoke after hitting the floor and
telephoned for an ambulance. She was treated with
intramuscular adrenaline in the ambulance because
systolic blood pressure had fallen to <80 mm Hg.
Initial investigations revealed a significant rise in
acute tryptase (12.3 ng/mL) with a normal baseline
level (2.1 ng/mL). Initially wheat or wheat-dependent
cofactor augmented anaphylaxis was suspected.
She was advised to avoid wheat, cyclooxygenase
inhibitors, and proton pump inhibitors (PPI) until
review.
Results for specific immunoglobulin E to wheat
and omega-5-gliadin were negative. Skin prick test
(SPT) to wheat solution (Inmunotek, Madrid, Spain)
and prick-to-prick with the index bread slice was also
negative. Skin prick test and intradermal tests (IDT)
to paracetamol (both 100 mg/mL, GlaxoSmithKline,
London, United Kingdom) were also negative. The
patient tolerated an oral challenge with 500 mg of
paracetamol together with a slice of the same index
bread with no adverse reaction.
The SPT (8 mg/mL) and IDT (8 mg/mL,
0.8 mg/mL and 0.08 mg/mL; AstraZeneca,
Bedfordshire, United Kingdom) were performed and
are shown in the Figure. Skin prick test to histamine
(positive control) and normal saline (negative
control) was positive at 5 mm and negative at
0 mm, respectively. Skin prick test to esomeprazole
was borderline positive with a 3-mm wheal and
flare. Intradermal test to esomeprazole was positive
at concentrations of 8 mg/mL, 0.8 mg/mL and
0.08 mg/mL; with 18-mm, 8-mm and 3-mm wheal
expansion, respectively. The SPT and IDT with
8 mg/mL and 0.8 mg/mL were negative in a healthy
control (the author) as shown in the Figure. To assess
for potential cross-reactivity, SPT (4 mg/mL) and
IDT (4 mg/mL and 0.4 mg/mL) to pantoprazole were
also performed and are also shown in the Figure. The
SPT was negative, but IDT was positive with 4 mg/mL and 0.4 mg/mL dilutions with 7-mm and 4-mm wheal expansion, respectively.
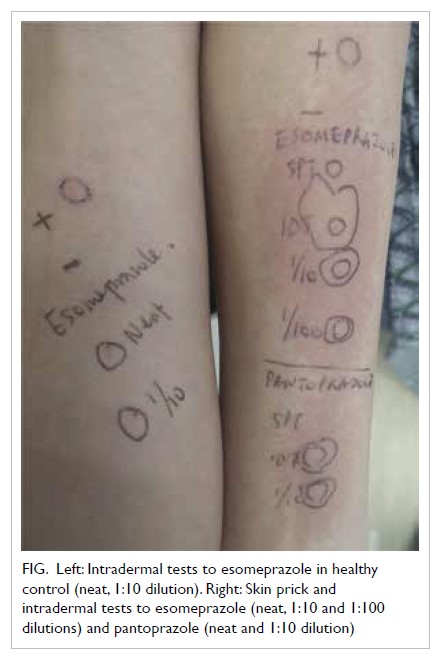
Figure. Left: Intradermal tests to esomeprazole in healthy control (neat, 1:10 dilution). Right: Skin prick and intradermal tests to esomeprazole (neat, 1:10 and 1:100 dilutions) and pantoprazole (neat and 1:10 dilution)
She was diagnosed with severe type I
hypersensitivity to esomeprazole with cross-sensitisation
to pantoprazole. Drug provocoation
testing was not indicated in view of the compatible
clinical history, strongly positive skin tests, and high
risk of anaphylaxis. The patient declined testing with
other PPI and was advised to avoid the entire class
until further workup. She was prescribed famotidine
20 mg twice a day for her dyspepsia with no adverse
effects.
This is the first reported case in Hong Kong of
PPI anaphylaxis and demonstrates the utility of skin
testing to assess potential cross-reactivity. Although
relatively uncommon, reports of hypersensitivity to
PPI are increasing, in parallel with their increasing
use worldwide. The majority of hypersensitivity reactions appear to be of the immediate type.1
Previous exposure to esomeprazole may have
been initial sensitising events. Despite common
misconception, clinicians should bear in mind that
prior tolerance of a certain drug does not preclude it
as a future cause of drug allergy. Although patterns
of cross-reactivity among various PPIs have been
reported, these remain controversial and a thorough
allergological workup should be performed for every
patient.2 Clinicians are reminded to be vigilant of
this uncommon cause of anaphylaxis and beware
of potential cross-reactivity. The SPT and IDT
have high specificity, but patients with suspected
PPI hypersensitivity and negative skin tests should
undergo drug provocation tests to confidently
exclude this important diagnosis.3
Author contributions
The author contributed to the concept or design, acquisition
of data, analysis or interpretation of data, drafting of the
manuscript, and critical revision for important intellectual
content. The author had full access to the data, contributed
to the study, approved the final version for publication, and
takes responsibility for its accuracy and integrity.
Conflicts of interest
The author has disclosed no conflicts of interest.
Funding/support
This pictorial medicine paper received no specific grant from any funding agency in the public, commercial, or not-forprofit
sectors.
Ethics approval
The patient consented to this publication.
References
1. Otani IM, Banerji A. Immediate and delayed
hypersensitivity reactions to proton pump inhibitors:
evaluation and management. Curr Allergy Asthma Rep
2016;16:17. Crossref
2. Tourillon C, Mahe J, Baron A, et al. Immediate-type
hypersensitivity cross-reactions to proton pump
inhibitors: a descriptive study of data from the French
National Pharmacovigilance Database. Int Arch Allergy
Immunol 2019;178:159-66. Crossref
3. Kepil Özdemir S, Yilmaz I, Aydin Ö, et al. Immediate-type
hypersensitivity reactions to proton pump inhibitors:
usefulness of skin tests in the diagnosis and assessment of
cross-reactivity. Allergy 2013;68:1008-14. Crossref

