Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Parapharyngeal space lipoma: a case report
Herbert SH Lee, MB, ChB (CUHK); CM Ngai, MB, BS, FHKAM (Otorhinolaryngology)
Department of Otorhinolaryngology, Head and Neck Surgery, Yan Chai Hospital, Kowloon West Cluster, Hong Kong
Corresponding author: Dr Herbert SH Lee (herbertshlee@link.cuhk.edu.hk)
Introduction
Parapharyngeal space (PPS) tumours account for
only around 0.5% of tumours in the head and neck
region.1 Most are benign in nature and salivary
in origin.2 Lipomas in the PPS are rare, despite
being the most common benign mesenchymal
head and neck tumour.3 4 Other lesions that may
be encountered in this area include neurogenic
tumours, chemodectomas, branchial cysts, and
metastatic lesions.
Case report
A middle-aged woman first presented to the
outpatient clinic in April 2019 with a 3-year history
of left painless neck mass, with gradual growth but
no other symptoms. Physical examination revealed a
soft neck mass of around 4 to 5 cm in diameter over
the left level III region. Other ear, nose and throat
examinations, including flexible laryngoscopy, were
unremarkable.
Initial fine-needle aspiration cytology (FNAC)
was inadequate for diagnosis. A second FNAC
revealed sparse adipose tissue. Ultrasound showed a
2.68×1.52×2.41 cm deeply located hypoechoic lesion
on the left submandibular region, with internal
striations resembling those of subcutaneous fat. No vascularity was detected on colour Doppler scan.
Oval lymph nodes with preserved fatty hilum were
seen at bilateral upper cervical regions. They all
had a sub-centimetre short axis, likely reactive in
nature. The overall sonographic impression was of
lipoma. Magnetic resonance imaging (MRI) revealed
a 3.6×4.9×9.2 cm (anteroposterior × transverse ×
craniocaudal planes) well-circumscribed, lobulated
mass in the left PPS. The lesion was of fat signal
intensity, with faint fluffy internal enhancing
septation but no internal enhancing solid nodule
seen, nor frank invasion into the surrounding
structures (Fig 1a). The lesion extended from the
level of C1 to C7 (Fig 1b), bulging medially onto the
left side of the oropharynx and displacing the left
carotid space content posterolaterally (Fig 1c). The
MRI findings were suggestive of a lipomatous lesion.
The overall clinical picture was compatible with a
parapharyngeal lipoma. Although parapharyngeal
lipoma is a benign lesion, gradual growth and
consequent mass effects can occur. As the patient
was only middle-aged, complications such as
dysphagia, shortness of breath, and obstructive sleep
apnoea were possible if the tumour was allowed to
continue growing. After explaining to the patient
the clinical, FNAC and imaging findings, as well as
potential complications arising from the tumour, she was keen to undergo surgical excision.
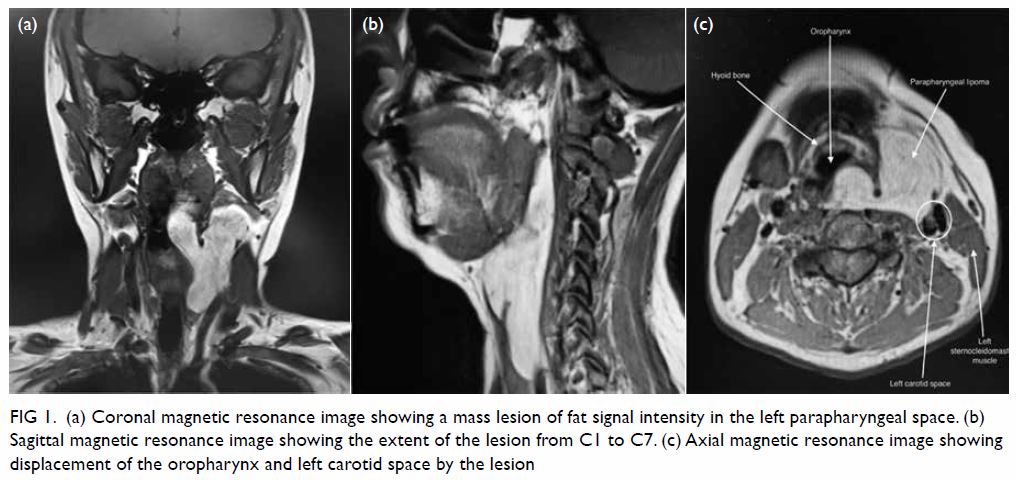
Figure 1. (a) Coronal magnetic resonance image showing a mass lesion of fat signal intensity in the left parapharyngeal space. (b) Sagittal magnetic resonance image showing the extent of the lesion from C1 to C7. (c) Axial magnetic resonance image showing displacement of the oropharynx and left carotid space by the lesion
During out-patient preoperative assessment
in July 2019, the patient complained of recent dull
vague pain in the throat. Physical examination
revealed the hyoid bone to be deviated to the right.
Subsequent flexible laryngoscopy demonstrated a
swelling on the left lateral oropharyngeal wall.
Surgery under general anaesthesia
was performed in August 2019 and the
sternocleidomastoid muscle was dissected from
the lipoma. The lipoma was subsequently dissected
from the internal jugular vein and the carotid artery
and completely excised (Fig 2). Haemostasis was
achieved and a drain inserted prior to skin closure.
The entire operation took about 2 hours with intra-operative
blood loss of around 50 mL. The patient
was discharged 5 days later with no complications
noted.
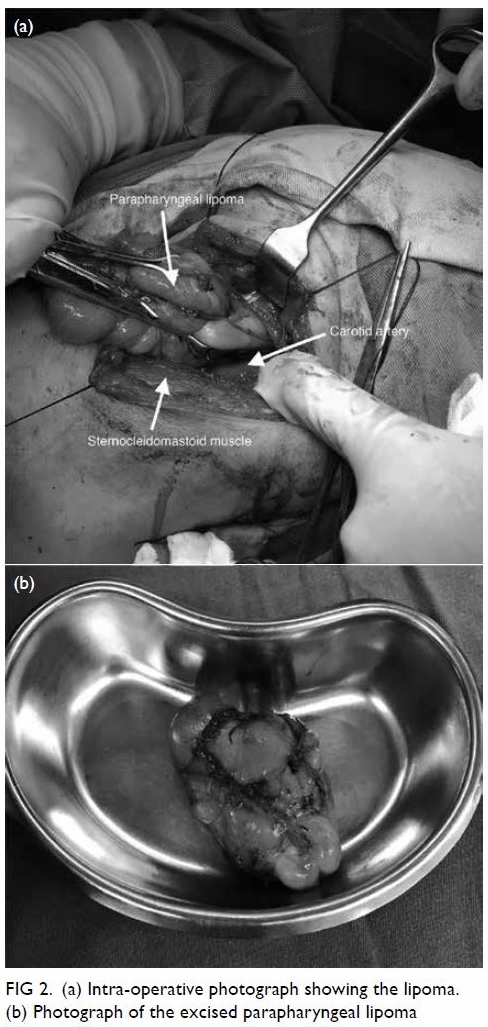
Figure 2. (a) Intra-operative photograph showing the lipoma. (b) Photograph of the excised parapharyngeal lipoma
At postoperative follow-up 9 days later the
patient was clinically well with no active complaints.
She was tolerating an oral diet and the wound had
healed well. Flexible laryngoscopy showed no more
oropharyngeal wall swelling. Pathology results
confirmed that the left parapharyngeal lesion was a
lipoma and the excised left level III lymph node had
no evidence of malignancy.
Discussion
The PPS is anatomically described as an inverted
pyramid with the apex and the base at the greater
cornu of the hyoid and the skull base, respectively.
The posterior boundary is the vertebral column and
paravertebral muscles. Anteriorly, it is limited by
the junction of pterygoid fascia to the buccinator
muscle fascia, the pterygomandibular raphe, and
the submandibular gland. The medial boundary is
formed by the superior constrictor muscle and the
tonsillar fossa. The lateral boundary is formed by the
medial pterygoid muscle, the ramus of mandible,
parotid gland, and the posterior belly of the digastric
muscle. The PPS can be subdivided into pre-styloid
and post-styloid compartments by the styloid
process. The post-styloid compartment consists
of several vital structures including the 9th to 11th
cranial nerves, internal carotid artery, internal jugular
vein, and cervical sympathetic trunk. The pre-styloid
compartment may contain the deep lobe of the
parotid gland or accessory salivary tissues, as well
as lymph nodes. A lipoma found in the pre-styloid
compartment of the PPS is indeed very rare.
A lipoma is an encapsulated, benign,
subcutaneous, and submucosal tumour composed
of mature adipose tissue cells. Most PPS lipomas
grow insidiously and cause symptoms only when
exerting mass effects as seen in any other benign
tumours, for example, dysphagia, shortness of
breath, and obstructive sleep apnoea. Occasionally,
due to obstruction of the Eustachian tube by the
tumour, otitis media with effusion and conductive
hearing loss may occur. Hoarseness and tongue
muscle weakness resulting from compression of the
lower cranial nerves, as well as Horner’s syndrome
and trismus owing to involvement of the cervical
sympathetic trunk and medial pterygoid respectively
are all suggestive of malignancy.
Diagnostic FNAC is often technically difficult
as the PPS lipoma is deep-seated. Most of the time,
imaging such as computed tomography (CT) and
MRI has significant diagnostic significance. On
computed tomography scan, a lipoma is revealed
as a homogenous and hypodense mass with no
enhancement. In contrast, MRI scan is the most ideal
imaging modality due to its excellent delineation
of soft tissue and multiplanar capability. Lipomas
appear as hyperintense on T1- and T2-weighted
sequences with internal septations. T1-weighted sequences with fat suppression demonstrate even
more obvious contrast with the surrounding soft
tissues.
Surgical excision is the treatment of choice.
The surgical approach depends on tumour size,
location, and relationship to major vessels. A
transcervical approach is most widely applied and
is particularly suitable for smaller PPS tumours.
Some literature suggests a transcervical approach
for tumours as large as 8 cm,5 6 but there is no
consensus on the cut-off size. Our case demonstrates
that the transcervical approach can achieve good
exposure for a parapharyngeal tumour extending
from level C1 to C7, 9.2 cm at its greatest dimension.
Advantages of a transcervical approach include
adequate exposure of vital structures and a lower
risk of damage to the facial nerves. A transcervical
approach is combined with a transmandibular
approach when dealing with larger lesions involving
the skull base and the aforementioned lower cranial
nerves for better exposure, while an infratemporal
approach is used when access to the lateral part of
the skull base is necessary. A transoral approach,
which was used in the past, is now out of favour as
the exposure offered by this route is very poor. There
is also a higher risk of vascular and neural injury that
makes this approach unsafe.
Conclusion
Parapharyngeal space lipomas are rarely seen in
our daily practice but deserve more of our attention
since they are easily missed in the early stages and
seen as a non-specific neck mass as in this case.
Magnetic resonance imaging scan is useful not
only in terms of diagnostic superiority, but also for
preoperative planning. A transcervical approach
is most commonly adopted for PPS tumours as it
is associated with lower surgical risk by providing
excellent exposure of vital neurovascular structures.
Author contributions
Concept or design: CM Ngai.
Acquisition of data: HSH Lee.
Analysis or interpretation of data: HSH Lee.
Drafting of the manuscript: HSH Lee.
Critical revision of the manuscript for important intellectual content: CM Ngai.
Acquisition of data: HSH Lee.
Analysis or interpretation of data: HSH Lee.
Drafting of the manuscript: HSH Lee.
Critical revision of the manuscript for important intellectual content: CM Ngai.
All authors had full access to the data, contributed to the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Funding/support
This case report received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
The study was conducted in accordance with guidelines by the Kowloon West Cluster ethics committee. Informed consent was obtained from the patient.
References
1. Carrau RL, Johnson JT, Myers EN. Management of tumors
of the parapharyngeal space. Oncology (Williston Park)
1997;11:633-40.
2. Batsakis JG, Sneige N. Parapharyngeal and retropharyngeal
space diseases. Ann Otol Rhinol Laryngol 1989;98:320-1. Crossref
3. Abdullah BJ, Liam CK, Kaur H, Mathew KM.
Parapharyngeal space lipoma causing sleep apnoea. Br J
Radiol 1997;70:1063-5. Crossref
4. Ulku CH, Uyar Y. Parapharyngeal lipoma extending to
skull base: a case report and review of the literature. Skull
Base 2004;14:121-5. Crossref
5. Smith JC, Snyderman CH, Kassam AB. Giant
parapharyngeal space lipoma: case report and surgical
approach. Skull Base 2002;12:215-20. Crossref
6. Carrau RL, Myers EN, Johnson JT. Management of
tumors arising in the parapharyngeal space. Laryngoscope
1990;100:583-9. Crossref

