Hong Kong Med J 2020 Oct;26(5):404–12 | Epub 25 Sep 2020
Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Rapid Estimate of Inadequate Health Literacy
(REIHL): development and validation of a
practitioner-friendly health literacy screening
tool for older adults
Angela YM Leung, PhD, FHKAN (Gerontology)1; Esther YT Yu, FHKCFP, FHKAM (Family Medicine)2; James KH Luk, FHKCP, FHKAM (Medicine)3; PH Chau, PhD4; Diane Levin-Zamir, PhD5,6; Isaac SH Leung, MPhil1; KT Cheung, MPhil7; Iris Chi, DSW8
1 Centre for Gerontological Nursing, School of Nursing, The Hong Kong
Polytechnic University, Hong Kong
2 Department of Family Medicine and Primary Care, Li Ka Shing Faculty of
Medicine, The University of Hong Kong, Hong Kong
3 Department of Medicine, Fung Yiu King Hospital, Hong Kong
4 School of Nursing, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong
5 Department of Health Education and Promotion, Clalit Health Services, Israel
6 School of Public Health, University of Haifa, Israel
7 Centre on Research and Advocacy, Hong Kong Society for Rehabilitation, Hong Kong
8 USC Suzanne Dworak-Peck School of Social Work, University of Southern California, Los Angeles, United States
Corresponding author: Dr Angela YM Leung (angela.ym.leung@polyu.edu.hk)
Abstract
Introduction: This study aimed to develop and
validate a brief practitioner-friendly health literacy
screening tool, called Rapid Estimate of Inadequate
Health Literacy (REIHL), that estimates patients’
health literacy inadequacy in demanding clinical
settings.
Methods: This is a methodological study of 304
community-dwelling older adults recruited from
one community health centre and five district elderly
community centres. Logistic regression models were
used to identify the coefficients of the REIHL score’s
significant factors. Receiver operating characteristic
(ROC) curve analysis was then used to assess the
REIHL’s sensitivity and specificity. Path analysis was
employed to examine the REIHL’s criterion validity
with the Chinese Health Literacy Scale for Chronic
Care and concurrent validity with self-rated health
scale and the Geriatric Depression Scale–15.
Results: The REIHL has scores ranging from 0 to
23. It had 76.9% agreement with the Chinese Health
Literacy Scale for Chronic Care. The area under the
ROC curve for predicting health literacy inadequacy
was 0.82 (95% confidence interval=0.78-0.87,
P<0.001). The ROC curve of the REIHL showed that
scores ≥11 had a sensitivity of 77.8% and specificity of
75.6% for predicting health literacy inadequacy. The
path analysis model showed excellent fit (Chi squared
[2, 304] 0.16, P=0.92, comparative fit index 1.00, root
mean square error of approximation <0.001, 90%
confidence interval=0.00-0.04), indicating that the REIHL has good criterion and concurrent validity.
Conclusion: The newly developed REIHL is a
practical tool for estimating older adults’ inadequate
health literacy in clinical care settings.
New knowledge added by this study
-
This paper contributes to the field of health literacy and primary care by:
- providing a practitioner-friendly tool for estimating individuals’ health literacy inadequacy without interrupting clinical workflow; and
- screening high-risk people in China for comprehensive health literacy assessment with the Chinese Health Literacy Scale for Chronic Care.
- Using this rapid estimation may allow doctors/nurses to avoid asking patients to complete a questionnaire, which may interrupt the clinical workflow or take up substantial time during medical consultations.
- The Rapid Estimate of Inadequate Health Literacy could also encourage practitioners to spend more time with those who have inadequate health literacy in health education and counselling.
Introduction
Health literacy is the ability to obtain, read,
understand, and use healthcare information to make
appropriate health decisions and follow treatment
instructions. Inadequate health literacy (IHL) is a
public health concern that is associated with poor
health outcomes and frequent use of health services.1
Identifying groups at risk for IHL is therefore crucial.
Screening tools such as the Rapid Evaluation of Adult
Literacy in Medicine–Revised (REALM-R),2 Rapid
Evaluation of Adult Literacy in Medicine–Short
form,3 Wide Range Achievement Test (WRAT-4),4
Newest Vital Sign (NVS),5 and Single-Item Literacy
Screener6 have been developed for assessment of
patients’ health literacy. Nonetheless, each of those
tools has limitations, hindering the extensive use of
rapid health literacy screening in clinical settings.
The REALM-R, Rapid Evaluation of Adult
Literacy in Medicine–Short form, and WRAT-4 focus
only on word recognition,7 representing a narrow
concept of health literacy and failing to address two
other crucial dimensions: ‘interpretation of health
information’ and ‘health decision making’.7 8 The
REALM-R and WRAT-4 health literacy assessments
require 2 to 3 and 3 to 5 minutes, respectively, to
administer. Thus, using the REALM-R or WRAT-4
demands special arrangements in clinical settings:
patients may be required to complete them prior
to consultation, and they may interrupt the usual
clinical workflow. An alternative is for the doctor to conduct the assessment, but the typical out-patient
clinical consultation period is about 7 minutes for
each patient, and adequate health literacy assessment
would occupy multiple minutes of this period.
The NVS is another recommended tool for
quick health literacy screening that compensates for
the shortcomings of previous tools by addressing the
need to understand and interpret health information
from a designated nutritional label. After reading the
label, the client answers six questions about it. The
assessment of these capacities by the NVS is both a
strength and a shortcoming, as it requires more time
to complete.9 Notably, older adults take 11.7 minutes
(range, 6-28 minutes) to complete the NVS, so its
practicality for quick assessment of elderly patients’
health literacy is limited.10
Another rapid health literacy assessment
tool is the Short-Form Test of Functional Health
Literacy in Adults, a 36-item tool that assesses
clients’ comprehension and numeracy abilities.11 It
is recommended to allot 7 minutes to complete the
assessment, and clients should stop when that time
is up. However, time-limited assessments can be
challenging for older adults because of their delayed
cognitive processing or age-related slowness. These
effects are typical but not pathological with age,
rendering the Short-Form Test of Functional Health
Literacy in Adults inappropriate for this population.12
Further, most of its contents were based on the US
healthcare system, making its generalisability to
other countries questionable.
The Single-Item Health Literacy Screening is
the simplest health literacy assessment, containing
only one item. Its key limitation is possible self-report
bias, as it assesses clients’ perceived ability to
read and understand health information from written
material, which may not reflect their actual abilities.6
Given the shortcomings of existing rapid
health literacy screening tools and the need to assess
patients’ health literacy in clinical settings, there
is a need to develop a rapid tool for non-English-speaking
older adults that can be used in different
healthcare systems and is based on available patient
data. The project team has developed several health
literacy tools for Chinese populations, including the
Chinese Health Literacy Scale for Diabetes,13 Chinese
Health Literacy Scale for Chronic Care (CHLCC),14
and Chinese Health Literacy Scale for Diabetes–Multiple Choice version.15 Although these tools
can be used in Chinese-speaking populations, they
require several minutes for clients to complete,
which may not be ideal for rapid screening in
busy clinics. Therefore, in this study, we aimed to
develop and validate a brief practitioner-friendly
health literacy screening tool, the Rapid Estimate of
Inadequate Health Literacy (REIHL), which employs
a multivariable prediction model to determine
patients’ risk for IHL in a demanding clinical setting.
Methods
Study design and participants
This is a cross-sectional, methodological study
that was conducted from August 2010 to January
2011. The Transparent Reporting of a Multivariable
Prediction Model for Individual Prognosis or
Diagnosis guidelines were also followed.16
Older adults from one community health
centre and five district elderly community centres
in Hong Kong were recruited. The inclusion criteria
were: (1) age ≥50 years; (2) cognitively capable (Short
Portable Mental Status Questionnaire Chinese
version score ≥7); and (3) able to communicate in
Cantonese. The sample size calculation was derived
from a receiver operating characteristic (ROC)
power calculation using the ‘power.roc.test’ function
under the ‘pRCO’ library in R version 3.6. Assuming
that the newly developed tool’s area under the curve
0.60, type 1 error 0.05, power 0.8, and attrition 20%,
at least 298 subjects should be recruited.17
Recruitment strategies included posters
at community centres, monthly meetings, and
in-person contact. All participants were interviewed
to assess their eligibility to participate. Ethical
approval was obtained from the Institutional Review
Board of The University of Hong Kong/Hospital
Authority Hong Kong West Cluster (Ref UW 09-033).
Procedure for developing the Rapid Estimate
of Inadequate Health Literacy
The newly developed REIHL screening tool was
devised using model estimation. Unlike other scale
development, we did not create the items for the
REIHL but collected socio-demographic data (age,
gender, education level, types of chronic illness) and
conducted the CHLCC on the subjects. Scores on
the CHLCC were used to determine which subjects
had IHL. People with CHLCC scores of <36 were
considered as having IHL. We then created a dummy
variable representing IHL (1: IHL; 0: adequate
health literacy). Socio-demographic factors (eg,
age, education level, types and number of chronic
illnesses) associated with IHL were identified, and
these became the items of the REIHL. Chronic
illnesses refer to conditions that last 1 year or more
and lead to limitations in activities of daily living
and/or require ongoing medical attention.18
Measurement
People with IHL were more likely to have more
depressive symptoms19 20 and poor self-rated health
(SRH).21 22 We therefore checked the criterion
validity and concurrent validity of REIHL with the
following validated scales.
The CHLCC was used to check the criterion
validity of REIHL. The CHLCC is a 24-item tool for measuring health literacy in Chinese populations
with four subscales (remembering, understanding,
applying, and analysing). It has good internal
(Cronbach’s alpha, 0.91) and test-retest (intraclass
correlation coefficient, 0.77; P<0.01) reliability.14
The Geriatric Depression Scale–15 (GDS-15)
and the SRH scale were used to check the REIHL’s
concurrent validity. The GDS-15 is used to assess
older adults’ depressive symptoms,23 and it has been
translated into Chinese and validated in Hong Kong
with good psychometric properties (Cronbach’s
alpha, 0.82; item-total correlation, 0.23-0.66).24 25 Its
total score ranges from 0 to 15, with higher values
representing increased depression levels. The SRH
is a validated single-item scale for assessing general
health status.26 It is a subjective assessment of general
health, asking ‘In the last 3 months, how would you
describe your health status?’ Five options are given:
‘very good’, ‘good’, ‘fair’, ‘poor’, or ‘very poor’, coded as
integers from 1 (very good) to 5 (very poor).
Statistical analyses
There were a few items of missing data, which
comprised about 2% of all data. Missing values
were filled in using multiple imputation in SPSS
(Windows version 25.0; IBM Corp, Armonk
[NY], US). Chi squared tests were used to assess
the bivariate relationships between demographic
variables and IHL. Logistic regression analyses were
used to further assess the multivariate relationships
among the factors that were significantly associated
with IHL. Model adequacy was evaluated
by Nagelkerke’s R2.27 To obtain an optimistic
assessment of the model’s prediction performance
and avoid overfitting, 10-fold cross-validation was
used, and error mean square (EMS) was reported.
To select the best model, we chose the model with
the smallest EMS and lowest Bayesian information
criterion (BIC) values. We derived the point scores
for REIHL with reference to the Framingham Study
Risk Score.16 The score for each item of the REIHL is
calculated by dividing its coefficient by the smallest
coefficient and then rounding up to the next highest
integer. The total REIHL score is the sum of the
scores of all items in the REIHL.
To test the reliability of the REIHL, we used
ROC curve analysis28 to assess its sensitivity and
specificity. We choose the optimum sensitivity
and specificity based on maximisation of Youden’s
index.29 We assessed the corresponding sensitivity
and specificity of each potential cut-off point. The
chosen cut-off point was the one with the largest
Youden’s index (ie, sensitivity + specificity − 1). We
also assessed the criterion validity and concurrent
validity of REIHL. Criterion validity refers to the
stated criterion, that is, the correspondence between
the results of this newly developed scale and those
of a validated health literacy scale. Concurrent validity is the extent to which a test relates to
another previously validated metric. Here, we tested
the REIHL’s criterion validity with the CHLCC and
the REIHL’s concurrent validity with two health
outcomes (depression and SRH). Path analysis30 was
also used to examine the criterion and concurrent
validity of REIHL with a validated health literacy
scale (CHLCC) and two health outcomes (depressive
symptoms and SRH) using MPlus version 7.31 We
assessed three fit indices to determine the goodness
of fit of the model: a model with non-significant Chi
squared value (P>0.05), comparative fit index ≥0.95,
and root mean square error of approximation ≤0.10
was considered to be a well-fitting model.32 33 We
also inspected the direction and significance of the
standardised estimate coefficients to determine the
effects of one variable on another.
Results
A total of 304 subjects were included in the analysis,
of whom 220 (72.4%) were female. In all, 185 (60.9%)
subjects were shown to have IHL when assessed by
the health literacy scale (CHLCC score <36). Age, gender, education level, and number of chronic
illnesses were significantly associated with CHLCC
(Table 1).
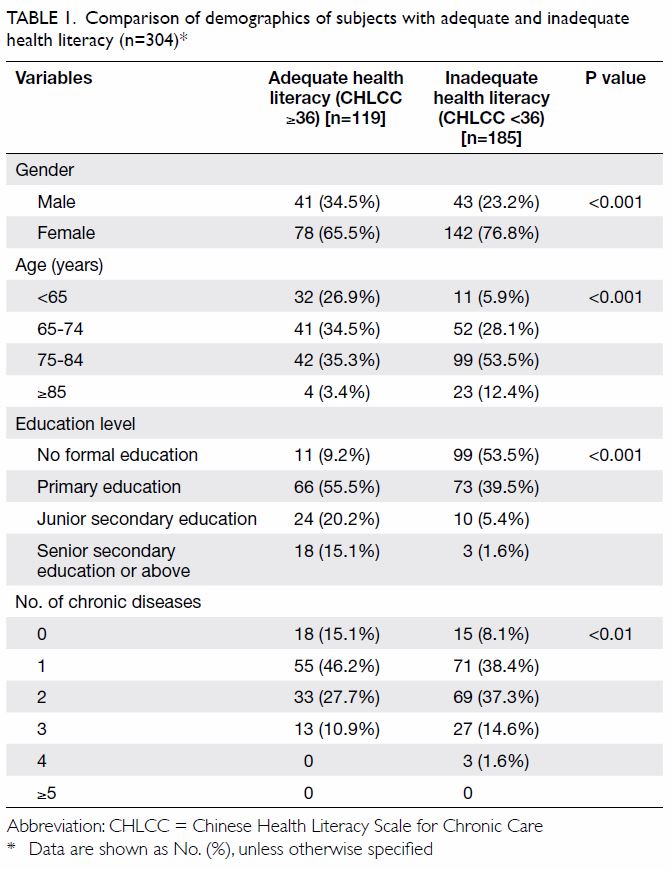
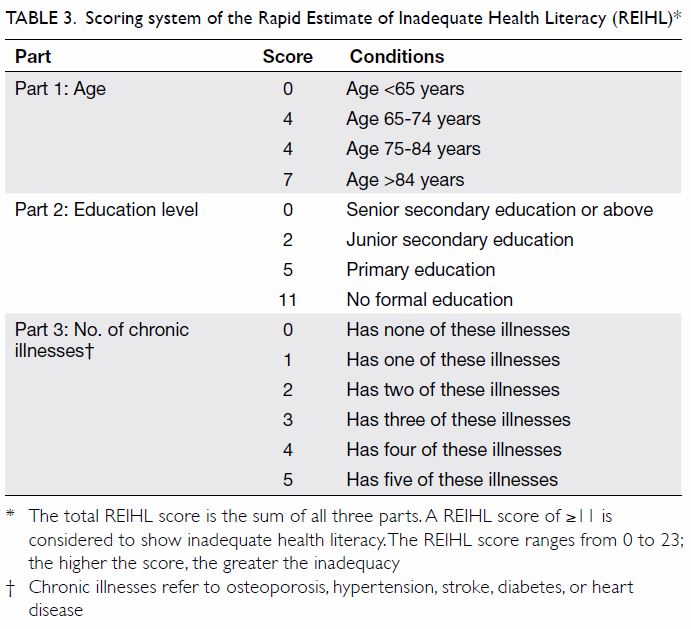
Table 1. Comparison of demographics of subjects with adequate and inadequate health literacy (n=304)
Because gender was significantly correlated
with education, we selected education level as the
representative variable used in the regression models
(Table 2). Model 1 employed a regression model that
incorporated age and education, and the results
were: Nagelkerke’s R2 0.39, EMS 0.15, and BIC 347.
To form Model 2, we added five chronic illnesses (ie,
diabetes, hypertension, stroke, heart disease, and
osteoporosis) into the regression; Nagelkerke’s R2
increased to 0.43, EMS to 0.16, and BIC to 359. In
Model 3, the selected chronic illnesses were replaced
by the number of chronic illnesses, and Nagelkerke’s
R2 became 0.40, EMS 0.15, and BIC 346. Because
Model 3 had the lowest BIC and EMS values, and its
Nagelkerke’s R2 was comparable to those of the other
two models, we considered Model 3 as the best and
final model.
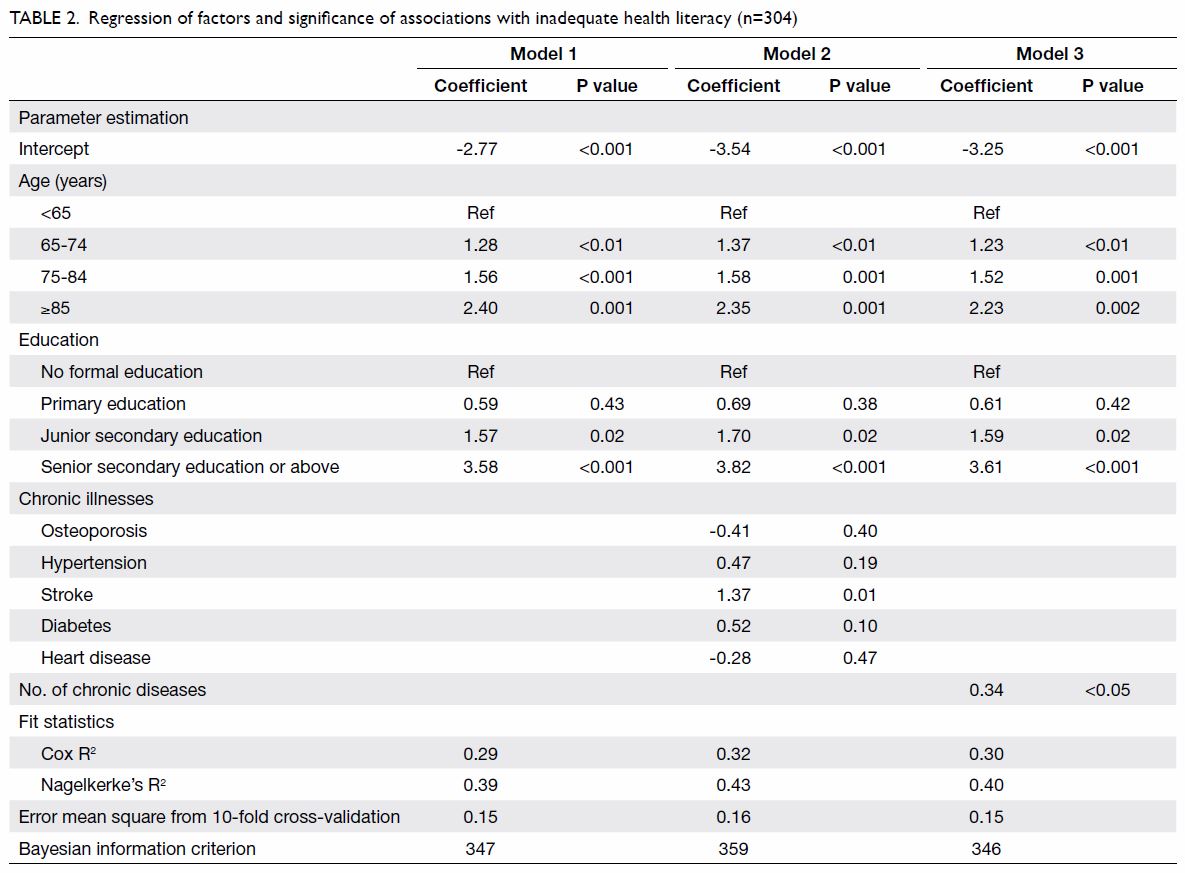
Table 2. Regression of factors and significance of associations with inadequate health literacy (n=304)
The coefficients of age, education level, and
number of chronic illnesses were identified in Model
3. The smallest coefficient was 0.34, and that value
was used as the denominator to calculate the score
for each item. Age was categorised and scored as
0, 4, 4, or 7; education level was scored as 0, 2, 5,
or 11; and chronic illnesses were scored from 0 to
5 depending on their number (Table 3). Therefore,
the total REIHL score ranged from 0 to 23. The
REIHL had 76.9% agreement with the CHLCC, the
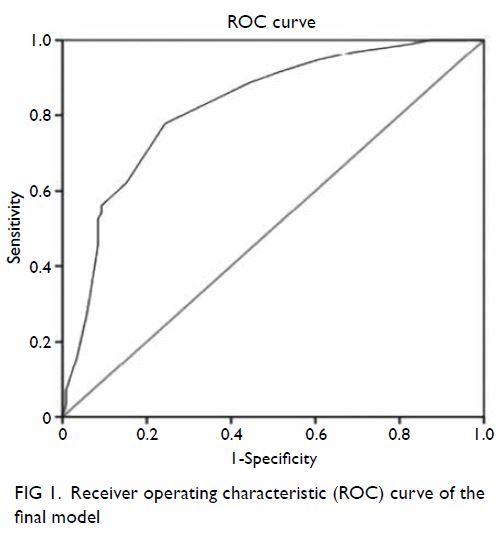
validated, reliable health literacy scale. The area
under the ROC curve for predicting IHL was 0.82
(95% confidence interval=0.78-0.87, P<0.001; Fig 1).
The curve for the REIHL showed that scoring ≥11
had a sensitivity of 77.8% and specificity of 75.6% for
predicting IHL. This criterion identified 60.9% of the
participants as having IHL.
All of the REIHL items had unique scores
except for two items under ‘Age’ that had the same
score (ie, 4) after rounding up. The actual score for
those aged 65 to 74 years was 3.71 (=1.27/0.34),
whereas that for those aged 75 to 84 years was
4.44 (=1.55/0.34). Because the difference between
the actual scores (3.71 and 4.44) was almost 1, we
considered the possibility of adjusting the score of
the item ‘aged 75 to 84 years’ to 5. The sensitivity
and specificity of the REIHL were 72.4% and 79.8%,
respectively, when adjusted accordingly. These
results were not significantly different from those
before adjustment. The agreement between REIHL
and CHLCC in the adjusted model was 75.3%, which
was lower than that before adjustment. The area
under the ROC curve of the adjusted REIHL was
0.83 (ie, very close to the corresponding value of
the unadjusted version). In view of the insignificant
improvement in psychometric properties, we
propose to not adjust the scoring of the item ‘aged
75 to 84 years’, leaving it as 4.
The path analysis model showed excellent fit
(Chi squared [2, 304] 0.16, P=0.92, comparative fit
index 1.00, root mean square error of approximation
<0.001, 90% confidence interval=0.00-0.04),
indicating the criterion validity and concurrent
validity of the REIHL (Fig 2). The path between
the REIHL and CHLCC (β= −32.69, P<0.001) was
statistically significant, implying that the REIHL was
significantly negatively associated with the CHLCC.
This shows the criterion validity of REIHL with a
validated health literacy instrument. A negative
association between the two scales is reasonable and
expected because the REIHL measures inadequacy,
unlike the CHLCC, which measures adequacy. The
path between the REIHL and the GDS-15 (β = 0.13,
P<0.01) was also statistically significant, but the path
between the REIHL and SRH was not. This implies
that there was a significant relationship between IHL
and depressive symptoms. The path between the
GDS-15 and SRH (β=1.02, P<0.001) was statistically
significant, indicating a strong relationship between
depression and poor SRH.
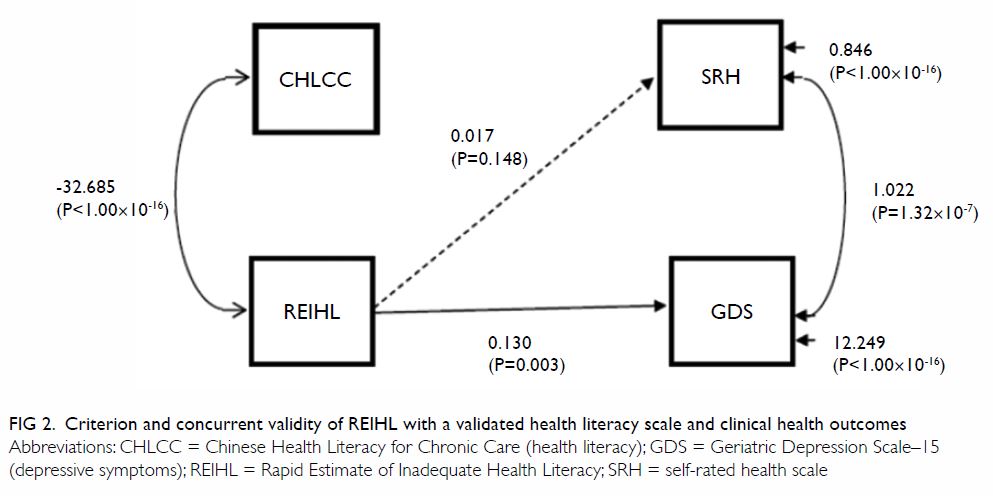
Figure 2. Criterion and concurrent validity of REIHL with a validated health literacy scale and clinical health outcomes
Discussion
The newly developed REIHL is a reliable screening
tool for estimating IHL among older adults in clinical
settings. Although REIHL is an estimation tool, it had
very good agreement with a validated health literacy
measure (CHLCC). This implies that if clinicians
have limited time to assess patients’ health literacy,
they could estimate it using the REIHL rather than
actually measuring patients’ health literacy levels.
The strengths of the REIHL are its reliability
and simplicity. We used several methods to test the
tool’s reliability. For instance, ROC analysis found
that the area under the curve was more than 80%,
and the sensitivity and specificity of the REIHL with a cut-off point of 11 reached an acceptable
level, indicative of an accurate assessment tool.
The relationships between REIHL and CHLCC
were well illustrated in the path analysis, indicating
that REIHL has reasonably good criterion validity.
Previous literature showed that adults with IHL were
more likely to have depressive symptoms19 20 and
poor SRH.21 22 The path analysis showed that REIHL
was significantly associated with GDS-15 but not
with SRH; however, the GDS-15 was significantly
associated with SRH, and the model showed good
fit. These findings confirmed the concurrent validity
of REIHL, as estimated IHL was significantly
associated with depression. This result provides
some added value, as IHL was indirectly associated
with poor SRH via depression. This means that older
adults’ poor SRH was caused not directly by IHL, but
by the presence of depression.
Three of the REIHL’s items (age, education,
and number of chronic illnesses) may be risk factors
for depression, so testing the tool’s association with
depression might be a challenge analogous to testing
the relationship between risk factors and poor
health outcomes. However, we are confident that
the inclusion of these items in the REIHL is a good
design choice to highlight the heterogeneity of older
adults and remind practitioners to be sensitive to the
differentiation among clients. People of advanced
age and low education are more likely to have
poor health outcomes (including depression), but
the age and education level at which practitioners
should be mindful of IHL remains unclear. The
REIHL is a reminder to practitioners to pay proper
attention to these important aspects so that they
can communicate with patients to self-manage
their health issues. Advocating the use of REIHL
is not intended to replace the concept of universal precaution in health literacy and its adoption, but it
highlights a population that needs special attention
regarding health literacy. In clinics where most
clients are older adults, practitioners could thereby
direct their limited time and resources to those in
the greatest need. By contrast, when encountering
less-educated clients, some practitioners do not
attempt to educate them, assuming they are unable
to understand or apply the information. In such
situations, the REIHL may encourage practitioners
to adopt strategies such as referring clients with IHL
to training. In one US study, people with IHL were
referred to regular telephone counselling provided
by health coaches (trained nurses, health educators,
and diabetes educators) for 12 months.34 The health
coaches delivered health advice/messages in simple
sentences over the phone. In a Hong Kong study,
multi-component nurse-led group meetings derived
from the concept of photovoice were arranged for
patients with diabetes, hypertension, and limited
health literacy.35 In these meetings, participants
used photos to express barriers to and facilitators
of physical activity and developed plans to improve
their health status.35 These two examples illustrate
how people with IHL have been supported to
communicate with healthcare professionals to make
their health decisions.
The REIHL can be used easily by clinicians
provided that they know the clients’ age, education
level, and number of chronic illnesses. Its scoring
system is simple, with the sum of all items forming
the total score. The different levels within each item
have unique scores, except for two age categories
(65-74 and 75-84 years), to both of which the score
4 was assigned. We investigated the possibility of
adding one more point to the latter category’s score,
but this did not contribute additional sensitivity or
specificity; therefore, we decided to keep the status
quo.
The REIHL could contribute to the hands-on
1-minute estimation of patients’ health literacy
levels that is sometimes performed in clinical areas.
Such a swift assessment allows practitioners to make
decisions in health education, such as avoiding the
use of jargon, providing simplified information and
illustrations, using the ‘teach-back’ method, and
encouraging patients’ questions. These strategies can
improve health behaviours among those with IHL.36
As IHL is a common phenomenon in clinical settings,
the Agency for Healthcare Research and Quality and
the Institute for Healthcare Improvement of the US
recommend that practitioners use the teach-back
method as a strategy of taking universal precautions
for health literacy (ie, applying such precautions to
all patients).37 In the teach-back method, patients
are asked to repeat the instructions they receive
from doctors and nurses, allowing healthcare
professionals to check patients’ understanding of the health messages and then re-teach or modify
the method of presentation if the patients do not
demonstrate comprehension. Throughout the
process, it is recommended that doctors and nurses
have a caring attitude and use plain language in
communication.38
Unlike other rapid estimation tools for health
literacy, such as the REALM-R, the REIHL does
not require clients to read aloud. This enables
practitioners to estimate patients’ health literacy
without embarrassing them, which is particularly
suitable to Chinese culture in view of the concept of
‘saving face’. Its application is highly recommended in
the management of geriatric patients, as such patients
are a heterogeneous group in terms of health literacy
adequacy. Older patients’ literacy problems may not
be obvious, as some may conceal their problems
out of shame or may not recognise their difficulties
with reading. Such individuals may be unable to ask
relevant health questions or may misunderstand
healthcare providers’ recommendations. As older
patients tend to have many co-morbidities, they
need to navigate the health care system and interpret
complex information, which are challenging for
people with IHL. Understanding patients’ health
literacy could allow the implementation of strategies
that could potentially improve their health and
reduce emergency attendance and hospital
admissions. Two strategies have been proven effective
to facilitate medication adherence and health
literacy. A self-management education programme
(two 30- to 40-minute weekly meetings followed
by four phone-based educational sessions) tailored
to health literacy was shown to increase adherence
to antihypertensive medication.39 Another strategy
is the use of a tailor-made comic book to facilitate
medication counselling sessions (two 45-minute
face-to-face meetings) administered by trained
volunteers.40 41 Because people with IHL are more
likely to have low confidence in medicine taking,33 42
health education of this kind can be beneficial to
people with chronic illnesses.
The REIHL is a screening tool for health literacy.
Because of its estimated nature and capacity for rapid
implementation, it is best used in ambulatory care or
out-patient care clinics. The REIHL cannot replace
the CHLCC, which assesses health literacy levels
accurately and directly. However, the REIHL is good
at identifying members of the high-risk population
on whom the administration of the CHLCC or other
health literacy tests is warranted. The prevalence of
IHL in this sample was high (61%), and this result is
comparable to those found in other populations: in
the Netherlands, the prevalence of IHL in patients
with arterial vascular disease was 76.7%,43 whereas
in Brazil, more than half of people with hypertension
(54.6%) had IHL.44 As the prevalence of IHL is
high across various populations, there should be no problems with the generalisation of this health
literacy tool. However, to determine whether the
REIHL can be applied in other populations or
nations, a cross-national study should be carried out
in future.45
Several limitations of this study should be
acknowledged. First, the cross-sectional design did
not allow us to investigate the causal relationship
between health literacy and health outcomes.
Second, because only Chinese subjects were
included, the threshold is only valid for Chinese older
adults, and whether the results can be generalised to
other non-Chinese populations is not known. Future
studies should investigate the scale’s psychometric
properties in other populations. Third, we recruited
volunteers from community district elderly centres,
so there is some selection bias based on interest and
motivation. Further, the tool measures the risk for
IHL based on patients’ background information;
thus, it is not sensitive to changes in an individual’s
personal health literacy level. Previous studies have
shown that cognitive impairment is strongly related
to low health literacy. However, we restricted the
inclusion criteria to those without impaired cognitive
function.46 Fourth, the REIHL relies on self-reported
items, so under-reporting or over-reporting are
possible. Inaccurate reporting may be the result of
stigma or the potential for embarrassment associated
with low education levels or literacy abilities. Caution
should be applied when interpreting REIHL scores.
Finally, the present dataset is too small to be split
into training and validation datasets. Future studies
with larger datasets should be used to validate this
scale.
Conclusion
The REIHL is a practitioner-friendly tool for
screening older adults’ risk for IHL, which can be
applied in clinical settings to identify at-risk groups.
This tool is particularly useful in demanding clinical
areas where older adults constitute the majority of
patients. Future studies should assess how using the
REIHL in a community clinical setting encourages
healthcare providers to relate better to patients with
lower health literacy and improves communication
with them.
Author contributions
Concept or design of study: AYM Leung, PH Chau, I Chi.
Acquisition of data: ISH Leung, KT Cheung.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: ISH Leung, KT Cheung.
Critical revision of the manuscript for important intellectual content: AYM Leung, EYT Yu, JKH Luk, D Levin-Zamir, I Chi.
Acquisition of data: ISH Leung, KT Cheung.
Analysis or interpretation of data: All authors.
Drafting of the manuscript: ISH Leung, KT Cheung.
Critical revision of the manuscript for important intellectual content: AYM Leung, EYT Yu, JKH Luk, D Levin-Zamir, I Chi.
All authors had full access to the data, contributed to the
study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, JKH Luk was not involved in the
peer review process of the article. Other authors have
disclosed no conflicts of interest.
Acknowledgement
The authors would like to acknowledge the invaluable
contribution of the study participants. Special thanks go to
the anonymous reviewers for their thoughtful review and
guidance.
Declaration
The findings of this study were presented in part as a poster
at the 10th International Symposium on Healthy Aging, Hong
Kong. Leung ISH, Leung AYM, Chau PH (2015, March 7-8).
Rapid Estimate of Inadequate Health Literacy (REIHL) for
community-dwelling Chinese older adults.
Data availability
The data that support the findings of this study are available
on request from the corresponding author. The data are not
publicly available because of privacy or ethical restrictions.
Funding/support
This project was funded by Seed Funding for Basic Research, HKU 2010-11 (Project No: 200911159075) of the University of Hong Kong.
Ethics approval
Approval was obtained from the Institutional Review Board of The University of Hong Kong/Hospital Authority Hong Kong
West Cluster (Ref UW 09-033).
References
1. Berkman ND, Sheridan SL, Donahue KE, Halpem DJ,
Crotty K. Low health literacy and health outcomes: an
updated systematic review. Ann Int Med 2011;155:97-107. Crossref
2. Davis TC, Long SW, Jackson RH, et al. Rapid estimate
of adult literacy in medicine: a shortened screening
instrument. Fam Med 1993;25:391-5.
3. Arozullah AM, Yarnold PR, Bennett CL, et al. Development
and validation of a short-form, rapid estimate of adult
literacy in medicine. Med Care 2007;45:1026-33. Crossref
4. Wilkinson GS, Robertson GJ. Wide Range Achievement
Test–Fourth Edition (WRAT-4). Lutz, FL: Psychological
Assessment Resources; 2006. Crossref
5. Weiss BD, Mays MZ, Martz W, et al. Quick assessment of
literacy in primary care: the newest vital sign. Ann Fam
Med 2005;3:514-22. Crossref
6. Morris NS, MacLean CD, Chew LD, Littenberg B. The
Single Item Literacy Screener: evaluation of a brief
instrument to identify limited reading ability. BMC Fam
Pract 2006;7:21. Crossref
7. Haun JN, Valerio MA, McCormack LA, Sørensen K,
Passche-Orlow MK. Health literacy measurement: an
inventory and descriptive summary of 51 instruments. J
Health Comm 2014;19 Suppl 2:302-33. Crossref
8. Carpenter CR, Kaphingst KA, Goodman MS, Lin MJ,
Melson AT, Griffey RT. Feasibility and diagnostic
accuracy of brief health literacy and numeracy screening
instruments in an urban emergency department. Acad Emerg Med 2014;2:137-46. Crossref
9. Shah LC, West P, Bremmeyr K, Savoy-Moore RT. Health
literacy instrument in family medicine: the “newest vital
sign” ease of use and correlates. J Am Board Fam Med
2010;23:195-203. Crossref
10. Patel PJ, Joel S, Rovena G, et al. Testing the utility of the
newest vital sign (NVS) health literacy assessment tool
in older African-American patients. Patient Educ Couns
2011;85:505-7. Crossref
11. Baker DW, Williams MV, Parker RM, Gazmararian JA,
Nurss J. Development of a brief test to measure functional
health literacy. Patient Educ Couns 1999;38:33-42. Crossref
12. Robinson S, Moser D, Pelter MM, Besbitt T, Paul SM,
Dracup K. Assessing health literacy in heart failure
patients. J Card Fail 2011;17:887-92. Crossref
13. Leung AY, Lou VW, Cheung MK, Chan SS, Chi I.
Development and validation of Chinese health literacy
scale for diabetes. J Clin Nurs 2013;22:2090-9. Crossref
14. Leung AY, Cheung MK, Lou VW, et al. Development and
validation of the Chinese Health Literacy Scale for chronic
care. J Health Comm 2013;18 Suppl 1:205-22. Crossref
15. Leung AY, Lau HF, Chau PH, Chan EW. Chinese Health
Literacy Scale for Diabetes–multiple-choice version
(CHLSD-MC): a validation study. J Clin Nurs 2015;24:2679-82. Crossref
16. Sullivan LM, Massaro JM, D’Agostino RB Sr. Presentation
of multivariate data for clinical use: The Framingham Study
risk score functions. Stat Med 2004;23:1631-60. Crossref
17. Li F, He H. Assessing the accuracy of diagnostic tests.
Shanghai Arch Psychiatry 2018;30:207-12.
18. Center for Disease Control and Prevention, US
Government. About chronic diseases. Available from:
https://www.cdc.gov/chronicdisease/about/index.htm. Accessed 17 May 2020.
19. Rhee TG, Lee HY, Kim NK, Han G, Lee J, Kim K. Is health
literacy associated with depressive symptoms among
Korean adults? Implications for mental health nursing.
Perspect Psychiatr Care 2017;53:234-42. Crossref
20. Puente-Maestu L, Calle M, Rodríguez-Hermonsa JL, et al.
Health literacy and health outcomes in chronic obstructive
pulmonary disease. Respir Med 2016;115:78-82. Crossref
21. Protheroe J, Whittle R, Bartlam B, Estacio EV, Clark L,
Kurth J. Health literacy, associated lifestyle and
demographic factors in adult population of an English city:
a cross-sectional survey. Health Expect 2017;20:112-9. Crossref
22. Liu YB, Liu L, Li YF, Chen YL. Relationship between health
literacy, health-related behaviors and health status: a
survey of elderly Chinese. Int J Environ Res Public Health
2015;12:9714-25. Crossref
23. Sheik JI, Yesavage JA. Geriatric Depression Scale (GDS):
recent evidence and development of a shorter version. Clin
Gerontol 1986;5:165-73. Crossref
24. Lee HC, Chiu HF, Kwok WY, et al. Chinese elderly and
the GDS short form: a preliminary study. Clin Gerontol
1993;14:37-42.
25. Boey KW, Chiu HF. Assessing psychological well-being of
the old-old: a comparative study of GDS-15 and GHQ-12.
Clin Gerontol 1998;19:65-75. Crossref
26. Lundberg O, Manderbacka K. Assessing reliability of a
measure of self-rated health. Scand J Soc Med 1996;24:218-24. Crossref
27. Nagelkerke NJ. A note on a general definition of the
coefficient of determination. Biometrika 1991;78:691-2. Crossref
28. Zweig MH, Campbell G. Receiver-operating characteristic
(ROC) plots: a fundamental evaluation tool in clinical
medicine. Clin Chem 1993;39:561-77. Crossref
29. Ruopp MD, Perkins NJ, Whitcomb BW, Schisterman EF.
Youden Index and optimal cut-point estimated from
observations affected by a lower limit of detection. Biom
J 2008;50:419-30. Crossref
30. Garson GD. Path analysis. Asheboro (NC): Statistical
Associates Publishers; 2014.
31. Muthén LK, Muthén BO. MPlus (version 6) [computer
software]. Los Angeles (CA): Muthén & Muthén; 2010.
32. Bentler PM. Comparative fit indexes in structural models.
Psychol Bull 1990;107:238-46. Crossref
33. Raykov T, Marcoulides GA. A First Course in Structural
Equation Modeling. 2nd ed. Mahwah (NJ): Erlbaum; 2006.
34. Hadden KB, Arnold CL, Curtis LM, et al. Barriers and
solutions to implementing a pragmatic diabetes education
trial in rural primary care clinics. Contemp Clin Trials
Commun 2020;18:100550. Crossref
35. Leung AY, Chau PH, Leung IS, et al. Motivating diabetic
and hypertensive patients to engage in regular physical
activity: a multi-component intervention derived from
the concept of photovoice. Int J Environ Res Public Health
2019;16:1219. Crossref
36. Nouri SS, Rudd RE. Health literacy in the “oral exchange”:
an important element of patient-provider communication.
Patient Educ Couns 2015;98:565-71. Crossref
37. Yen PH, Leasure AR. Use and effectiveness of the teach-back
method in patient education and health outcomes.
Fed Pract 2019;36:284-9.
38. Warde F, Papadakos J, Papadakos T, Rodin D, Salhia M,
Giuliani M. Plain language communication as a priority
competency for medical professionals in a globalized
world. Can Med Educ J 2018;9:e52-9. Crossref
39. Delavar F, Pashaeypoor S, Negarandeh R. The effects of
self-management education tailored to health literacy on
medication adherence and blood pressure control among
elderly people with primary hypertension: a randomized
controlled trial. Patient Educ Couns 2020;103:336-42. Crossref
40. Leung AY, Leung IS, Liu JW, Ting S, Lo S. Improving
health literacy and medication compliance through comic
books: a quasi-experimental study in Chinese community-dwelling
older adults. Glob Health Promot 2018;25:67-78.Crossref
41. Wu SW, Tse DT, Chui JC, et al. Educational comic book
versus pamphlet for improvement of health literacy in
older patients with type II diabetes mellitus: a randomized
controlled trial. Asian J Gerontol Geriatr 2017;12:60-4.
42. Lee YM, Yu HY, You MA, Son YJ. Impact of health literacy
on medication adherence in older people with chronic
diseases. Collegian 2017;24:11-8. Crossref
43. Strijbos RM, Hinnen JW, van den Haak RF, Verhoeven BA,
Koning OH. Inadequate health literacy in patients with
arterial vascular disease. Eur J Vasc Endovasc Surg
2018;56:239-45. Crossref
44. Costa VR, Costa PD, Nakano EY, Apolinário D, Santana AN.
Functional health literacy in hypertensive elders at primary
health care. Rev Bras Enferm 2019;72 Suppl 2:266-73. Crossref
45. Sharma S, Weathers D. Assessing generalizability of
scales used in cross-national research. Int J Res Mark
2003;20:287-95. Crossref
46. Federman AD, Sano M, Wolf MS, Siu AL, Halm EA. Health
literacy and cognitive performance among older adults. J
Am Geriatr Soc 2009;57:1475-80. Crossref
sref