Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
COMMENTARY
Proliferation of syndromes and acronyms in
paediatric critical care: are we more or less confused?
KL Hon, MB, BS, MD1; Alexander KC Leung, FRCP(UK), FRCPCH2; Jeff CP Wong, MB, BS, MRCPCH1
1 Department of Paediatrics and Adolescent Medicine, The Hong Kong Children’s Hospital, Hong Kong
2 Department of Pediatrics, University of Calgary and Alberta Children’s Hospital, Calgary, Canada
Corresponding author: Dr KL Hon (ehon@hotmail.com)
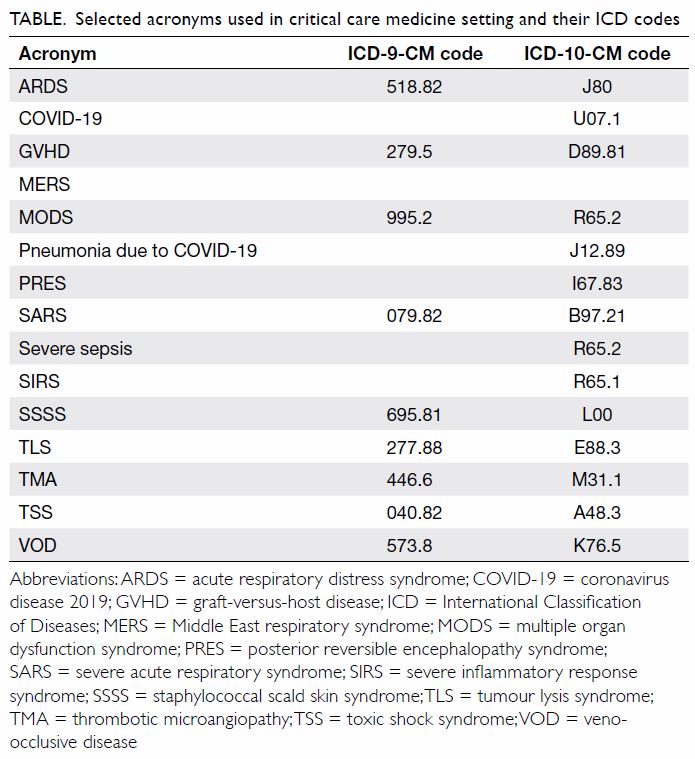
As with many disciplines in medicine, syndromes,
abbreviations, and acronyms have been coined to
aid diagnosis and prognostication in paediatric
intensive or critical care medicine (CCM). Although
these acronyms are commonly used, they remain
controversial. In clinical practice, CCM syndromes
are clinical patterns resulting from the interaction
between insult and host response. They are closely
correlated to organ system failures and are common
presentations of diverse aetiologic factors. Therefore,
it is important to search for underlying aetiologies
and subtypes. In research, the role of acronyms and
syndromes is limited in epidemiological studies and
clinical trials enrolling patients meeting syndrome criteria, unless underlying subtypes and aetiologies
are considered. As a result, study outcomes are often
negative. Hence, we advocate that both syndrome
codes and underlying aetiologic diagnoses be
provided in International Classification of Diseases
(ICD) coding to record prognostic and therapeutic
significance (Table). Last, non-standardised
acronyms contribute to confusion and should be
used sparingly. Herein, we review some examples
of syndromes and acronyms in use in CCM settings
and consider whether their use is justified.
Acute respiratory distress syndrome (ARDS)
is an important cause for CCM admission.1 2
Ashbaugh et al3 first described ARDS as an adulttype
respiratory distress for a group of patients
with progressive respiratory failure, refractory
hypoxaemia, decreased functional residual capacity
and lung compliance, and diffuse infiltration on
chest radiography. In 1994, the American-European
Consensus Conference introduced ARDS as a disease
with acute-onset hypoxaemia, PaO2/FiO2 ratio ≤200,
bilateral infiltrates on chest radiographs, and the
absence of left atrial hypertension.4 The international
consensus criteria for ARDS were updated in 2012
and are known as the Berlin definition.5 However,
ARDS is not a specific disease entity; it is a clinical
syndrome which may be triggered by various
pathologies such as trauma, pneumonia, and sepsis.
As with many other syndromes, the term essentially
describes non-cardiogenic pulmonary oedema of
various aetiologies.
Acute respiratory distress syndrome also
occurs in children, and is no longer restricted to
adults.6 In 2015, the Paediatric Acute Lung Injury
Consensus Conference proposed a definition for
paediatric ARDS.7 This definition identified more
patients with ARDS than did the Berlin criteria,
but there were no differences in clinical outcomes.8
However, the Berlin definition offers no room for
stratifying and identifying true ARDS patients
because there is no re-evaluation of hypoxaemia
under standard ventilator setting in a specific time
period.9
The current (2015) ICD code for ARDS is 518.82. This code is seldom used in paediatric
hospital records in Hong Kong because many cases
are diagnosed as pneumonia rather than ARDS. As
a result, the hospital admission database might not
accurately reflect the epidemiology of the disease in
Hong Kong.10
Acute lung injury (ALI) was previously
considered as a mild form of ARDS with PaO2/FiO2
of 200 to 300 mg Hg in the setting of a wedge pressure
<18 mg Hg, bilateral infiltrates radiographically
consistent with pulmonary oedema, and no clinical
evidence of cardiac failure. It follows that patients
with ARDS have ALI. However, the acronym has
fallen into disuse and has been removed from Berlin
definition to minimise confusion.11
In 2003, the World Health Organization
(WHO) coined a new term severe acute respiratory
syndrome (SARS) for an outbreak of pneumonitis
that was later found to be a novel coronavirus
pneumonia and a form of ARDS.12 Subsequently,
there was an outbreak of acute pneumonitis due
to another coronavirus in the Middle East, which
the WHO coined severe acute respiratory illness
(SARI) and later changed to Middle East respiratory
syndrome (MERS).12 These acronyms (SARI and
MERS) are widely used but essentially represent
a form of ARDS or atypical pneumonia causing
ARDS, making them unnecessary and potentially
confusing.13 14 Some of these outbreaks were not
so severe or had extra-respiratory symptoms,
rendering the term SARS equivocal. No further
novel syndromes or acronyms for ARDS have been
coined by WHO to date. Nevertheless, COVID-19
has been coined to represent the current outbreak of
coronavirus disease that started in December 2019.
Most cases are mild but there have been patients
who died of respiratory failure and ARDS.12
Multiple organ dysfunction syndrome (MODS),
also known as multiple organ failure, total organ
failure, or multisystem organ failure, refers to altered
organ function in an acutely ill patient requiring
medical intervention to achieve homeostasis.15 16 The
definition of MODS is less controversial than that
of ARDS, and MODS is also applied in paediatric
CCM settings. Typically, MODS results from
infection, accident, surgery, hypoperfusion, and
hypermetabolism. The primary underlying aetiology
triggers an uncontrolled inflammatory response.
Sepsis is the most common cause of MODS. The
altered organ function in patients with MODS
is such that homeostasis cannot be maintained
without intervention, and typically involves two or
more organ systems.15 Management of MODS is
mostly supportive, primarily maintaining adequate
tissue oxygenation. The current ICD-10-CM code
for MODS is 995.92. Prognosis is proportionate to
the number of organ systems involved and is worse
if cardiopulmonary and neurologic involvements are present. Mortality varies from 30% to 100% where
the chance of survival is diminished as the number
of organs involved increases.
Sepsis is a major disease in CCM settings.17
Various grading terms have been used such as sepsis,
severe inflammatory response syndrome (SIRS),
severe sepsis, septic shock, and recalcitrant septic
shock.18 Confirmation of an aetiological pathogen is
not required, and SIRS can be easily defined using
physiological parameters only. The current 2019
ICD-10-CM code for SIRS is R65.1 for that of non-infectious
origin and R65.11 for that with acute
organ dysfunction. Prognosis for SIRS is based on the
underlying diagnosis and co-morbidities. The Third
International Consensus Definitions for Sepsis and
Septic Shock (Sepsis-3) criteria define septic shock
as a subset of sepsis in which particularly profound
circulatory, cellular, and metabolic abnormalities
are associated with a greater risk of mortality than
with sepsis alone.16 Patients with septic shock can be
clinically identified by a vasopressor requirement to
maintain a mean arterial pressure of ≥65 mm Hg and
serum lactate level >2 mmol/L (>18 mg/dL) in the
absence of hypovolaemia.16 Many cases of paediatric
sepsis are underdiagnosed and likely coded in
hospital records in alternative diagnoses such as
febrile seizure, encephalitis, urinary tract infection,
or myocarditis.
Toxic shock syndrome (TSS) and staphylococcal
scald skin syndrome (SSSS) are sepsis syndromes that
are used only occasionally.19 20 Bacterial toxins such
as the streptococcal or staphylococcal enterotoxins
are implicated in their pathogenesis.21 Prognosis
depends mainly on the promptness in diagnosis and
treatment instituted. However, neither the organism
nor the toxins (eg toxic shock syndrome toxin 1) are
commonly or routinely isolated, therefore limiting
the usefulness of these terminologies. In paediatrics,
there have been keen proliferations of novel
acronyms in the recent COVID-19 pandemic due
to the virus SARS-CoV-2. Paediatric multisystem
inflammatory syndrome (PMIS), multisystem
inflammatory syndrome in children (MIS-C), and
paediatric inflammatory multisystem syndrome
temporally associated with SARS-CoV-2 (PIM-TS)
are all recently coined acronyms for a systemic disease
involving persistent fever, inflammation, and organ
dysfunction following exposure to SARS-CoV-2.
This syndrome has been considered to resemble
Kawasaki disease and SIRS and associated with the
hyperinflammation in cytokine release syndrome
and cytokine storm syndrome.22
Conclusion
The acronym syndromes encountered in CCM
settings are descriptive terminologies that should
remain simple in definition. However, such syndromes may not necessarily aid diagnosis and
prognostication. Users of these acronyms must
understand the limitations and confusions behind
these terminologies. Terms such as SARI, ALI,
TSS, and SSSS are used infrequently and should
be eliminated to avoid confusion. The underlying
aetiologies of any syndrome must be explored and
treated. For disease coding and prognostication
analyses, all relevant aetiological factors must be
considered.
Author contributions
All authors contributed to the concept of the study, acquisition
and analysis of the data, drafting of the manuscript, and
critical revision of the manuscript for important intellectual
content. All authors had full access to the data, contributed to
the study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
As an editor of the journal, KL Hon was not involved in the
peer review process. Other authors declare that they have no
other conflict of interest.
Funding/support
This commentary received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
1. Dellinger RP, Levy MM, Carlet JM, et al. Surviving sepsis
campaign: international guidelines for management
of severe sepsis and septic shock: 2008. Crit Care Med
2008;36:296-327. Crossref
2. Cornfield DN. Acute respiratory distress syndrome in
children: physiology and management. Curr Opin Pediatr
2013;25:338-43. Crossref
3. Ashbaugh DG, Bigelow DB, Petty TL, Levine BE. Acute
respiratory distress in adults. Lancet 1967;2:319-23. Crossref
4. Bernard GR, Artigas A, Brigham KL, et al. The American-European Consensus Conference on ARDS. Definitions,
mechanisms, relevant outcomes, and clinical trial
coordination. Am J Respir Crit Care Med 1994;149(3 Pt
1):818-24. Crossref
5. ARDS Definition Task Force, Ranieri VM, Rubenfeld GD,
et al. Acute respiratory distress syndrome: the Berlin
Definition. JAMA 2012;307:2526-33. Crossref
6. Li CY, Luk MP, Hon KL. Paediatric acute respiratory distress
syndrome: a review of recent advances in management. J
Paediatr Respirol Crit Care 2016;12:4-9.
7. The Pediatric Acute Lung Injury Consensus Conference
Group. Pediatric acute respiratory distress syndrome: consensus recommendations from the Pediatric Acute
Lung Injury Consensus Conference. Pediatr Crit Care Med
2015;16:428-39. Crossref
8. Gupta S, Sankar J, Lodha R, Kabra SK. Comparison of
prevalence and outcomes of pediatric acute respiratory
distress syndrome using pediatric acute lung injury
consensus conference criteria and berlin definition. Front
Pediatr 2018;6:93. Crossref
9. Villar J, Kacmarek RM. The American-European
Consensus Conference definition of the acute respiratory
distress syndrome is dead, long live positive end-expiratory
pressure! Med Intensiva 2012;36:571-5. Crossref
10. To KK, Hung IF, Li IW, et al. Delayed clearance of viral
load and marked cytokine activation in severe cases of
pandemic H1N1 2009 influenza virus infection. Clin Infect
Dis. 2010;50:850-9. Crossref
11. López-Fernández Y, Azagra AM, de la Oliva P, et al. Pediatric
acute lung injury epidemiology and natural history study:
incidence and outcome of the acute respiratory distress
syndrome in children. Crit Care Med 2012;40:3238-45. Crossref
12. Hon KL, Leung KK. Severe acute respiratory symptoms
and suspected SARS again 2020. Hong Kong Med J
2020;26:78-9. Crossref
13. Hon KL, Li AM, Cheng FW, Leung TF, Ng PC. Personal
view of SARS: confusing definition, confusing diagnoses.
Lancet 2003;361:1984-5. Crossref
14. Hon KL. MERS = SARS? Hong Kong Med J 2015;21:478. Crossref
15. Ames SG, Workman JK, Olson JA, et al. Infectious
etiologies and patient outcomes in pediatric septic shock. J
Pediatric Infect Dis Soc 2017;6:80-6.
16. Singer M, Deutschman CS, Seymour CW, et al. The third
international consensus definitions for sepsis and septic
shock (Sepsis-3). JAMA 2016;315:801-10. Crossref
17. Tusgul S, Carron P-N, Yersin B, Calandra T, Dami F. Low
sensitivity of qSOFA, SIRS criteria and sepsis definition
to identify infected patients at risk of complication in
the prehospital setting and at the emergency department
triage. Scand J Trauma Resusc Emerg Med 2017;25:108. Crossref
18. Rhee C, Klompas M. New sepsis and septic shock
definitions: clinical implications and controversies. Infect
Dis Clin North Am 2017;31:397-413. Crossref
19. Resnick SD. Staphylococcal toxin-mediated syndromes in
childhood. Semin Dermatol 1992;11:11-8.
20. Leung AK, Barankin B, Leong KF. Staphylococcal-scalded
skin syndrome: evaluation, diagnosis, and management.
World J Pediatr 2018;14:116-20. Crossref
21. Leung TN, Hon KL, Leung AK. Group A Streptococcus
disease in Hong Kong children: an overview. Hong Kong
Med J 2018;24:593-601. Crossref
22. Hon KL, Leung KK, Leung AK, et al. Overview: The history
and pediatric perspectives of severe acute respiratory
syndromes: novel or just like SARS. Pediatr Pulmonol 2020
Jun 1. Epub ahead of print. Crossref