Hong Kong Med J 2020 Jun;26(3):248–9.e1–3 | Epub 29 Apr 2020
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
High-resolution computed tomography in a patient with COVID-19 with non-diagnostic serial radiographs
HM Kwok, MB, BS# 1; SC Wong, MB, BS# 1TF Ng, MB, BS, FHKAM (Radiology)1; KS Yung, MB, BS1; WH Luk, MB, BS, FHKAM (Radiology)1KF Ma, MB, BS, FHKAM (Radiology)1; Thomas SH Chik, MRCP (UK), FHKAM (Medicine)2
1 Department of Radiology, Princess Margaret Hospital, Hong Kong
2 Infectious Disease Team, Princess Margaret Hospital, Hong Kong
# The first two authors contributed equally to the work
Corresponding author: Dr HM Kwok (hmkwok15@hotmail.com)
Case
A 63-year-old Chinese man from Wuhan, China, presented to the emergency department of Princess Margaret Hospital, Hong Kong, in January 2020 with coryzal symptoms.
He was afebrile with unremarkable respiratory examination results. He was admitted to an isolation ward for further investigation. He subsequently developed a fluctuating fever up to 38.5°C after admission and passed loose stool intermittently. His oxygen saturation levels were normal throughout hospitalisation. Supportive treatment and empirical antibiotics (amoxicillin-clavulanate) were administered.
Coronavirus disease 2019 (COVID-19) was suspected, and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection was confirmed the next day by throat swab and nasopharyngeal aspirate tests. Stool culture was negative for SARS-CoV-2 and other pathogens.
Blood test results revealed lymphopoenia (0.6 × 109/L). Total white blood cell count (4.4 × 109/L), absolute neutrophil count (3.4 × 109/L), monocyte count (0.3 × 109/L), and eosinophil count (0.0 × 109/L) were normal. Liver and renal function test results, C-reactive protein level, and serum calcium and phosphate levels were normal.
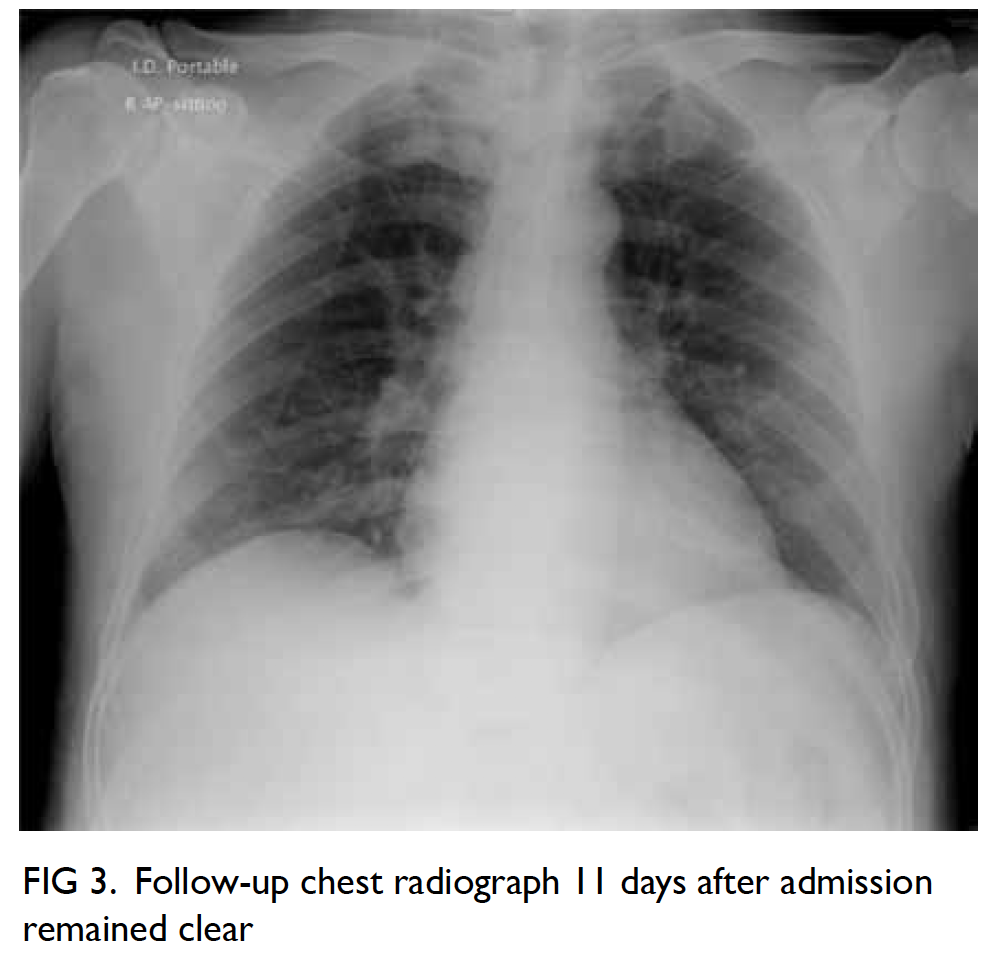
Daily portable chest radiographs over the next 5 days were unremarkable (Fig 1). Chest high-resolution computed tomography (HRCT) was performed to assess for pulmonary involvement. High-resolution computed tomography performed 6 days after admission (Fig 2) demonstrated a few patchy subpleural ground-glass opacities in both lungs. No other abnormalities were detected. Subsequent follow-up chest radiograph (Fig 3) remained clear.
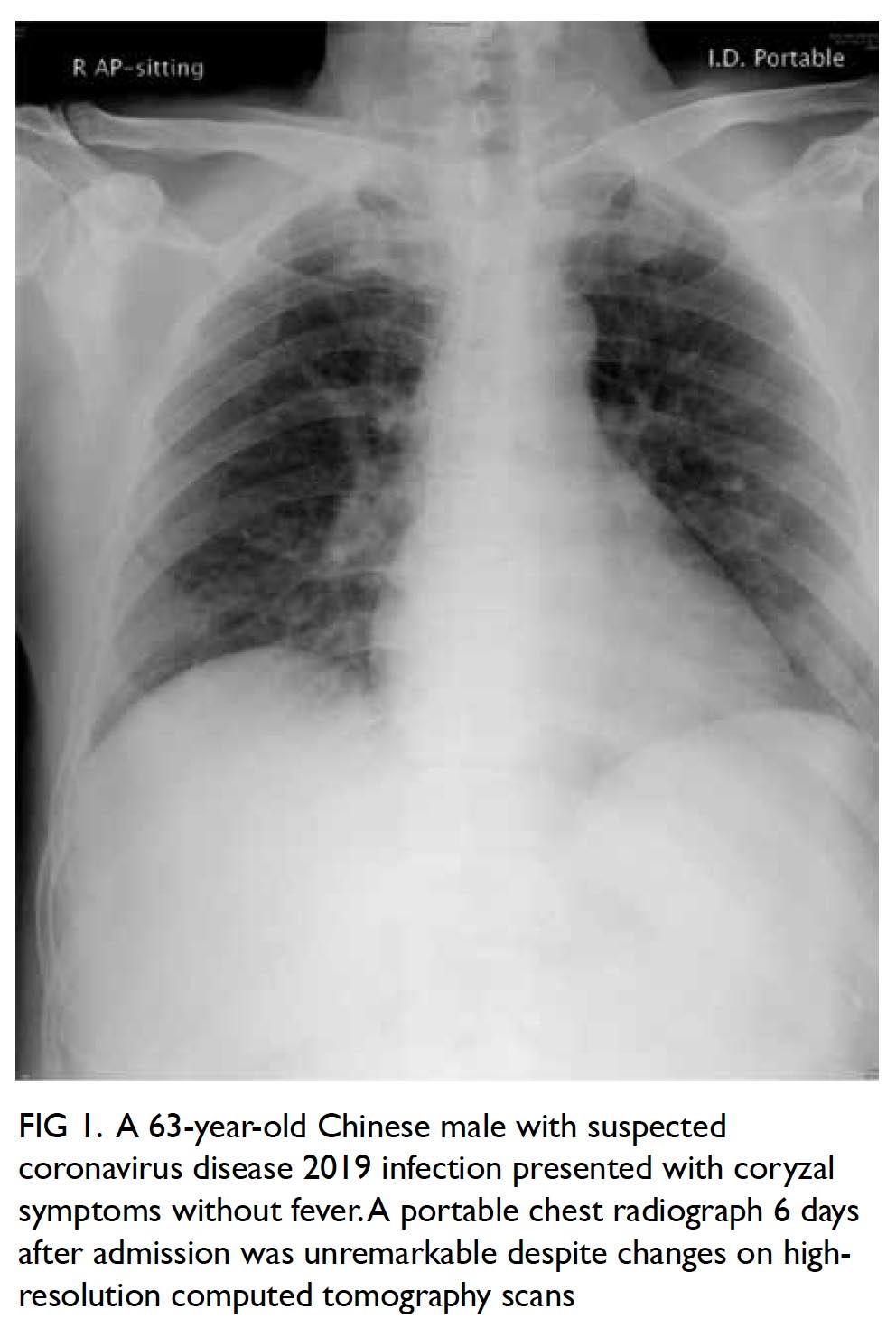
Figure 1. A 63-year-old Chinese male with suspected coronavirus disease 2019 infection presented with coryzal symptoms without fever. A portable chest radiograph 6 days after admission was unremarkable despite changes on high-resolution computed tomography scans
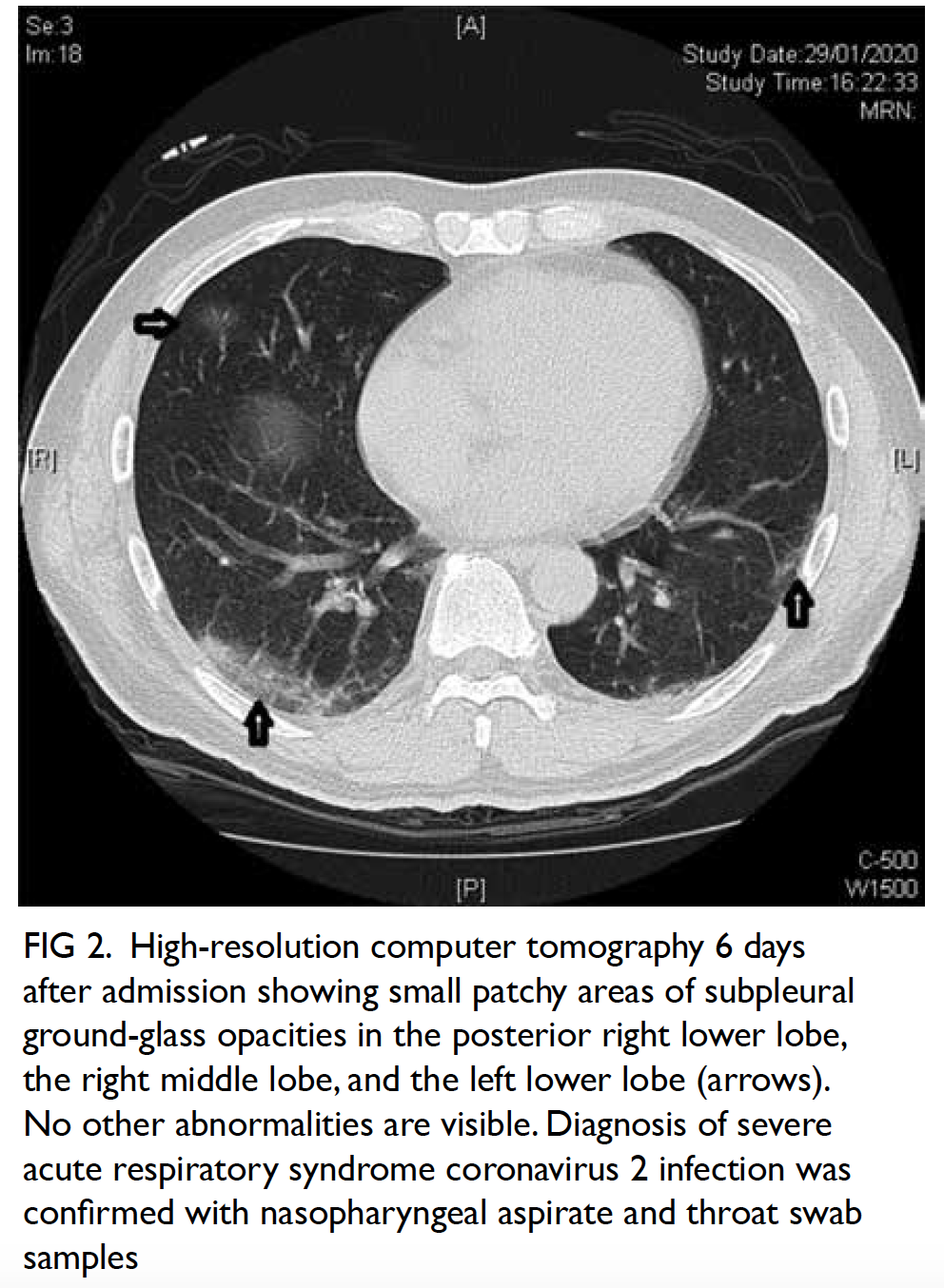
Figure 2. High-resolution computer tomography 6 days after admission showing small patchy areas of subpleural ground-glass opacities in the posterior right lower lobe, the right middle lobe, and the left lower lobe (arrows). No other abnormalities are visible. Diagnosis of severe acute respiratory syndrome coronavirus 2 infection was confirmed with nasopharyngeal aspirate and throat swab samples
The patient’s fever subsided 11 days after admission. No supplemental oxygen was required. Serial nasopharyngeal aspirate sample tests turned negative 22 days after admission. The patient was discharged from the hospital 27 days after admission.
Discussion
The SARS-CoV-2 infection is diagnosed with reverse transcription polymerase chain reaction results of respiratory specimens.
Prior to availability of confirmatory
microbiological test results, challenges exist in decision
making for patients with suspected COVID-19.
We advocate that early HRCT should be
considered in suspected cases to aid in clinico-radiological
diagnosis of SARS-CoV-2 infection by
demonstrating compatible radiological features,
before microbiological confirmation has been
established.
This can be especially beneficial if patients
have negative preliminary virology or radiographic
findings, as in the previously reported HRCT features
in severe acute respiratory syndrome (SARS) and
Middle East respiratory syndrome (MERS),1 2 as well
as recent reports on COVID-19 from China3 and Hong Kong.4
Findings on serial chest radiographs before and
after HRCT remain occult without demonstrable
airspace opacity, limiting its value in initial
assessment, monitoring or exclusion of pulmonary
involvement.
This is consistent with experience during the
SARS epidemic that HRCT was useful for early
radiological assessment for patients with negative
chest radiographs.5
Our patient subsequently demonstrated a
favourable outcome with recovery and did not require
supplemental oxygen throughout hospitalisation.
Mirroring experiences in previous coronavirus
outbreaks such as SARS and MERS, we believe that
HRCT will likely play a key role in aiding diagnosis,
assessing the extent of pulmonary involvement and
risk in the current COVID-19 pandemic. Early HRCT
can be beneficial in patients with obscure clinical
presentation or negative preliminary virological or
radiographic findings.
Author contributions
All authors contributed to the concept or design of the study,
acquisition of the data, drafting of the manuscript, and critical
revision of the manuscript for important intellectual content.
All authors had full access to the data, contributed to the
study, approved the final version for publication, and take
responsibility for its accuracy and integrity.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
We would like to express our gratitude to the Infectious
Disease Team and “dirty team” physicians of Princess Margaret
Hospital, Hong Kong, for their professional patient care and
invaluable contribution to the understanding of a novel disease.
Funding/support
This pictorial medicine paper received no specific grant from
any funding agency in the public, commercial, or not-for-profit
sectors.
Ethics approval
This study was approved by the Kowloon West Cluster
Research Ethics Committee (Ref KW/EX-20-049(145-08)).
References
1. Koo HJ, Lim S, Choe J, Choi SH, Sung H, Do KH. Radiographic and CT features of viral pneumonia.
Radiographics 2018;38:719-39. Crossref
2. Franquet T. Imaging of pulmonary viral pneumonia. Radiology 2011;260:18-39. Crossref
3. Lei J, Li J, Li X, Qi X. CT imaging of the 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology
2020;295:18. Crossref
4. World Health Organization. Clinical management of
severe acute respiratory infection when COVID-19 is
suspected. Interim guidance. Available from: https://
www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected. Accessed 6
Feb 2020.
5. Hui JY, Hon TY, Yang MK, et al. High-resolution computed tomography is useful for early diagnosis of severe acute
respiratory syndrome-associated coronavirus pneumonia
in patients with normal chest radiographs. J Comput
Assist Tomogr 2004;28:1-9. Crossref