Hong Kong Med J 2020 Jun;26(3):208–15 | Epub 4 Jun 2020
Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Communication skills of providers at primary
healthcare facilities in rural China
Q Zhou, MSc1; Q An, MSc1; N Wang, MSc1; Jason Li, BS2; Y Gao, MD, PhD3; J Yang, PhD1; J Nie, PhD1; Q Gao, PhD1; H Xue, PhD1
1 Center for Experimental Economics in Education, Shaanxi Normal University, Xi’an, China
2 Harvard Medical School, Harvard University, United States
3 Cadre Training Centre, National Health and Family Planning Commission of People’s Republic of China, Beijing, China
Corresponding author: Ms J Yang (jyang0716@163.com)
Abstract
Introduction: Effective provider-patient communication has been confirmed to improve
diagnosis, treatment planning, health outcomes,
patient satisfaction, and treatment compliance.
Few studies have measured the effectiveness
of communication between patients and rural
providers in China. To fill this gap in the literature,
the present study describes the communication skills
of providers at primary healthcare facilities in rural
China and investigates the provider- and facility-level
factors underlying these communication skills.
Methods: The standardised patients successfully
completed 504 interactions across two tiers of China’s
rural health system and engaged with providers
at village clinics and township health centres. We
assessed providers’ communication skills based on
recorded interactions between the providers and the
standardised patients using the SEGUE Framework,
which contains the following five dimensions: ‘Set
the stage’, ‘Elicit information’, ‘Give information’,
‘Understand the patient’s perspective’, and ‘End the
encounter’.
Results: The providers’ overall average score was
50.6% on the SEGUE communication tasks. They did
well in ‘Set the stage’ (54.4%) and ‘Elicit information’
(56.2%) but performed poorly in ‘End the encounter’
(24.5%) and ‘Understand the patient’s perspective’
(44.0%). Female and younger providers scored 0.75 (P<0.05) and 0.04 (P<0.01) points higher than their
male and older counterparts on total SEGUE score,
respectively.
Conclusion: Providers in rural China had relatively
poor communication skills overall, especially in
terms of their demonstration of care for patients
and inviting them to participate in the interaction.
Gender and age were significantly associated with
providers’ level of communication skills in rural
China.
New knowledge added by this study
- Rural providers in China scored 50.6% on the SEGUE Framework, revealing relatively poor communication skills.
- No correlations were found between education level and communication skills in rural China.
- The ability of providers in townships to establish a relationship with patients was worse than that of providers in villages.
- Policy officials and medical educators must focus on systemically reforming medical school curricula and integrating evidence-based communication skills training rather than simply encouraging further education using an outdated curriculum.
- Appropriate incentives should be provided to encourage rural providers and improve their job satisfaction.
- It is necessary to enhance the ability of providers in townships to communicate with strangers.
Introduction
A wealth of literature has demonstrated the
importance of providers’ communication skills
to the delivery of high-quality healthcare.1 2
Although definitions of effective provider-patient
communication vary, some common attributes are as follows: establish a provider-patient relationship,
elicit and understand patient perspectives, convey
empathy and affirmation, and reach shared decisions
regarding treatment and goals.2 3 Effective provider-patient
communication has been shown to improve
diagnoses, treatment plans, health outcomes, patient satisfaction, and treatment compliance1 2 4;
in contrast, deficiencies in provider-patient
communication are associated with patient anger,
frustration,5 and malpractice litigation.6
Measuring and improving providers’
communication skills are especially critical in
rural China’s primary healthcare facilities. As rural
residents’ first points of contact, village clinics and
township healthcare centres provide services for
a large proportion of the population in those areas
(40.42%)7 8; however, their quality of service remains
low.9 10 For example, Shi et al9 found that rural
clinicians were incorrect in 41% of their diagnoses
and gave prescriptions that were unnecessary or
harmful 64% of the time.
Existing research has reached the consensus
that quality medical care is heavily dependent
on providers’ communication skills,1 2 4 but some
prominent limitations also exist. First, to our
knowledge, no studies have measured provider-patient
communication skills in rural primary
healthcare facilities in China. Instead, existing
research has focused on medical students and related
education11 12 or examined providers in upper-tier
hospitals.13 14 15 Second, studies have primarily
relied on recall-based assessments, such as patient
exit interviews or surveys, which may be biased or
inaccurate.12 14 Finally, students and clinicians in
those studies are notified in advance that they are
being evaluated, which may lead them to deviate
from their actual clinical behaviours because they know they are being observed (also known as the
‘Hawthorne Effect’).12 13 14
Given the above, it is critically important
to understand how rural providers communicate
with their patients. The primary goal of this study
was to systematically describe and analyse the
communication skills of primary care providers in
China’s rural healthcare system and to identify the
provider- and facility-level factors of providers’
interactions with standardised patients (SPs).
Methods
Setting and study design
Stratified random sampling was employed as the
sampling method. The study sample was drawn from
rural areas in three provinces: Anhui, Eastern China;
Sichuan, Central China; and Shaanxi, Western China.
Specifically, 21 counties were randomly selected
from a total of 24 counties in the sample provinces.
Within the selected counties, 209 township health
centres and 139 village clinics were randomly
selected as the study sample (441 providers in total).
Two separate waves of data collection were
conducted among the village- and township-level
providers: an initial provider survey conducted in June
2015 and visits by SPs in August 2015. The provider
survey included items about basic demographic
characteristics, educational attainment, medical
experience, medical instruments, and the facility in
which they worked. In August 2015, SPs visited all
sampled township health centres and village clinics
with concealed devices to record their encounters.
The recordings were then transcripted with the
consultation of the SPs.
Standardised patients
A total of 63 individuals (42 male and 21 female;
mean age 36 years; range, 25-50 years) were hired
and trained as SPs in three provinces (21 from each
province). To be qualified as SPs, they had to be of
average weight and height and in good overall health
with no obvious signs of illness or other conditions
that might influence the accuracy of diagnoses.
The SPs were divided into 21 groups of three. In
each group, each SP was taught to report a case
of either pulmonary tuberculosis, childhood viral
gastroenteritis, or unstable angina. In each location,
the group of three SPs visited the township health
centre in a randomly arranged order. Only one SP was
sent to village clinics to minimise the risk that SPs
were identified as fake patients. The case reported by
SPs visiting a village clinic was randomly determined
beforehand. Upon presenting to the provider, the SPs
made an opening statement describing the primary
symptom(s) of their disease case (fever and cough
for pulmonary tuberculosis, diarrhoea for viral
gastroenteritis, or chest pain for angina). For the viral gastroenteritis cases, the SPs presented the case
of a child who was not present. The SPs responded
to all questions asked by the providers following a
predetermined script, purchased all medications
prescribed (which are sold by providers in China),
and paid the providers their fees. After each visit, the
SPs were debriefed using a structured questionnaire,
and the SPs’ responses were confirmed against a
recording of the interaction taken using a concealed
recording device.
Measuring communication skills
Over the past 10 years, China has used various
methods and tools to measure the communication
level of Chinese providers; although progress has
been made, rigorously validated and widely accepted
measurement tools are still lacking. Meanwhile,
studies in other countries have used a variety
of verified scales owing to their large amount of
research on this topic over the last 30 years. The
SEGUE Framework is one of the most common
tools used to assess providers’ communication skills.
In previous studies, the scale has demonstrated
acceptable psychometric characteristics (inter-rater
reliability, validity, and sensitivity to differences in
performance) in varied contexts.11 14 15 16
First developed by Makoul,17 the SEGUE
Framework employs a nominal (Yes/No) scale to
allow coders to assess medical communication skills
using a task-based checklist. The SEGUE checklist
contains 25 items, which are classified into the five
aforementioned dimensions as follows: (1) ‘Set the
stage’ [5 items]; (2) ‘Elicit information’ [10 items];
(3) ‘Give information’ [4 items]; (4) ‘Understand
the patient’s perspective’ [4 items]; and (5) ‘End
the encounter’ [2 items]. Each of the 25 items
comprising the SEGUE Framework can also be
coded into one of two categories: communication
content (17 items) or communication process (8
items). Communication content tasks include topics
raised or behaviours enacted at least once during
the encounter (eg, Discuss antecedent treatments).
Conversely, communication process items focus
on the manner in which providers communicate,
assessing aspects such as behaviours that should be
maintained throughout the encounter (eg, Maintain
a respectful tone).17 We used a Chinese version
of the SEGUE, which was translated to test the
communication skills of Chinese medical students.11
Eight research assistants were recruited
from the local community and trained to code the
providers’ communication skills. Following a highly
structured protocol, we conducted a series of training
sessions to ensure that the coders could understand
and accurately use the SEGUE Framework to score
various possible behaviours and interactions. The
coders then followed the transcripts while listening
to the recordings and identified the targeted behaviours contained in the SEGUE Framework
whenever they occurred. Coders were blinded to the
provider-, facility-, and regional-level characteristics
of each encounter. The overall score for all of the
different communication dimensions was computed
by adding the total scores for each dimension per
encounter. The Cronbach’s α internal consistency
reliability estimate of SEGUE Framework is 0.63.
This moderate reliability result suggests that the
SEGUE Framework is an acceptable measurement
tool.
Statistical analysis
We calculated the mean, standard deviation, and
scoring rate (the rate at which providers achieved the
SEGUE checklist items) across all SP interactions for
each of our primary outcomes: the five dimensions,
Communication content, Communication process,
and the total score across all five SEGUE dimensions.
Ordinary least squares regressions were conducted
to assess the correlates of the different dimensions
of communication skills. For each of the primary
outcomes mentioned above, we assessed the
correlations with a fixed set of provider-level and
facility-level characteristics. These included the
provider’s gender, age, education, certification,
number of patients in catchment area, number of
full-time physicians employed at the facility, distance
between the county hospital and the facility, and the
monetary value of the facility’s medical instruments.
All regressions controlled for the fixed effects of
the disease cases, the SPs, and the coders. Analyses
were conducted using Stata 14.2 (Stata Corporation;
College Station, [TX], United States).
Results
Provider and facility characteristics
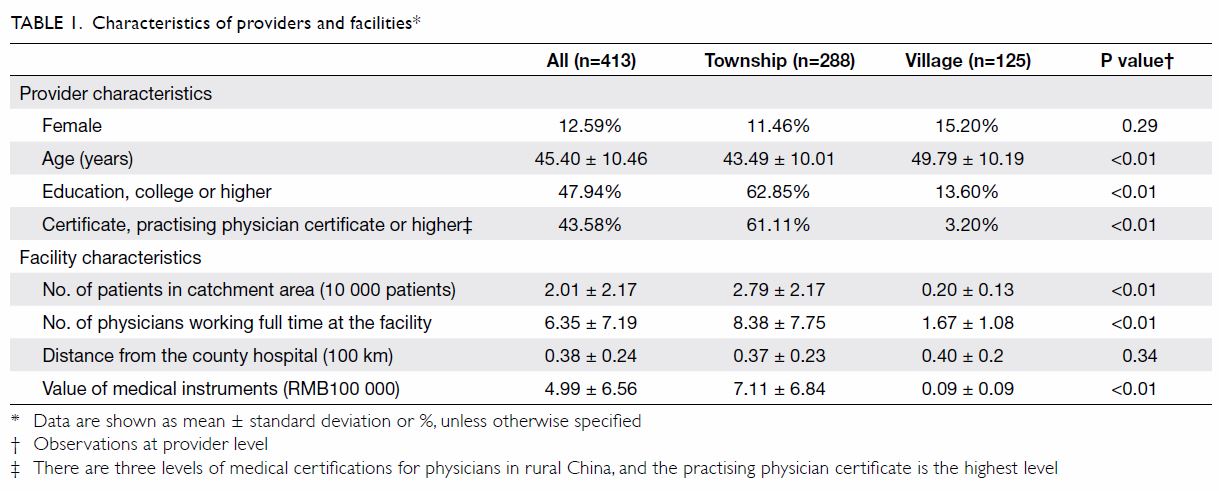
A total of 413 providers and 504 SP encounters were
included in our analysis (Table 1). The providers’
mean age was 45.40 years, and 87.4% of them were
male. A total of 47.9% of the providers had achieved
a minimum education level of college diploma, and
43.6% had a practising physician certificate, which
is the highest level of medical certification that can
be obtained by physicians in rural China. Township
health centres had a more developed and extensive
medical infrastructure than village clinics had
(P<0.01): the average value of the medical equipment
in township health centres was much higher than
that in village clinics (RMB 711 000 vs RMB 9000;
Table 1).
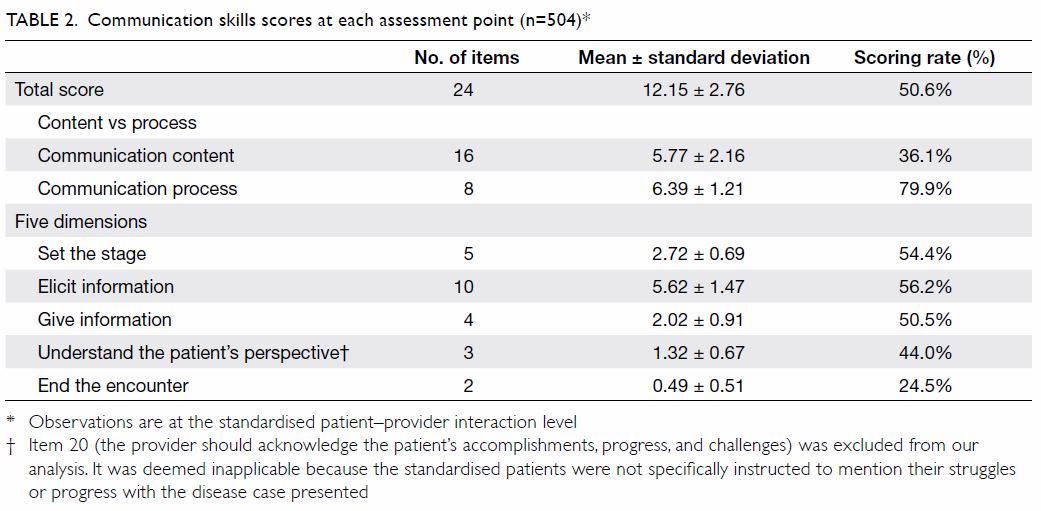
Communication skills scores
Table 2 shows the descriptive statistics for the total
SEGUE score and each of the five SEGUE dimensions.
On average, providers scored 50.6% (12.15 of 24)
on all SEGUE communication tasks (range, 16.7%-79.2%; 4-19 of 24), indicating that providers in rural
China had relatively poor communication skills.
Moreover, the providers scored means of 36.1%
(5.77 of 16) and 79.9% (6.39 of 8) on Communication
content and Communication process, respectively.
Among the five SEGUE dimensions, the providers
had difficulty with ‘End the encounter’ and
‘Understand the patient’s perspective’, scoring
means of 24.5% (0.49 of 2) and 44.0% (1.32 of 3), but
attained relatively high mean scores of 54.4% (2.72 of
5) and 56.2% (5.62 of 10) in ‘Set the stage’ and ‘Elicit
information’, respectively.
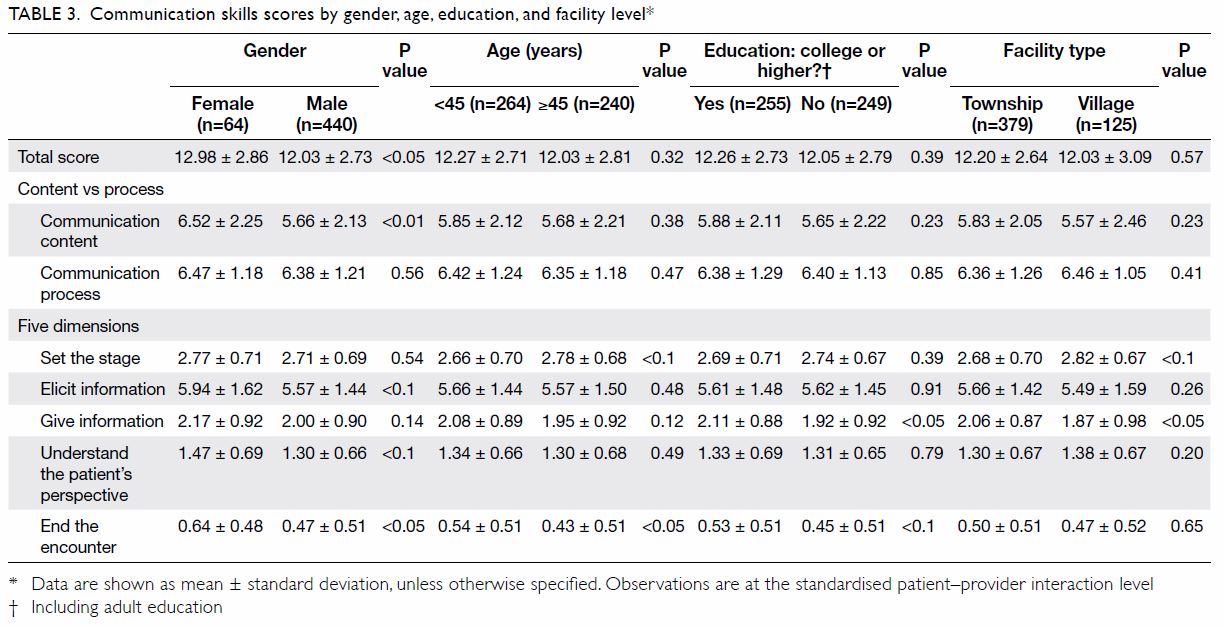
Further summary statistics of provider
communication skills are presented by gender, age,
education, and facility type in Table 3. The total
score achieved by female providers was slightly
but significantly higher than that of male providers (12.98 vs 12.03, P<0.05), which was also the case
for Communication content (6.52 vs 5.66, P<0.01),
‘Elicit information’ (5.94 vs 5.57, P<0.1), ‘Understand
the patient’s perspective’ (1.47 vs 1.30, P<0.1), and
‘End the encounter’ (0.64 vs 0.47, P<0.05). We
found statistically significant differences when
the individual SEGUE dimensions were examined
among subgroups. For instance, providers aged <45
years, who had a college education, and who were
based in township health centres performed better in
‘Give information’ and ‘End the encounter’. However,
their counterparts scored higher in ‘Set the stage’.
Predictors of providers’ communication
skills
Table 4 shows the results of multiple linear regressions
between the different dimensions of communication skills and provider and facility characteristics.
The provider’s gender was the factor that had the
strongest correlation with communication skills.
Female providers scored 0.75 points higher in their
total communication score (P<0.05) and 0.71 points
higher in the aspect of Communication content
(P<0.05) than their male counterparts. Among the five different dimensions of interaction that were
examined, female providers mainly excelled in their
ability to ‘Elicit information’, scoring about 0.42
points higher than male providers did (P<0.05). In
addition to provider gender, provider age was also
significantly correlated with communication skills.
Younger providers scored 0.04 points higher than their older counterparts on total SEGUE
score (P<0.01). Younger providers were more likely to score
higher in three of the five SEGUE dimensions:
‘Elicit information’, ‘Give information’, and ‘End the
encounter’. The results of the regressions without
correction for fixed effects are shown in the online
supplementary Appendix.
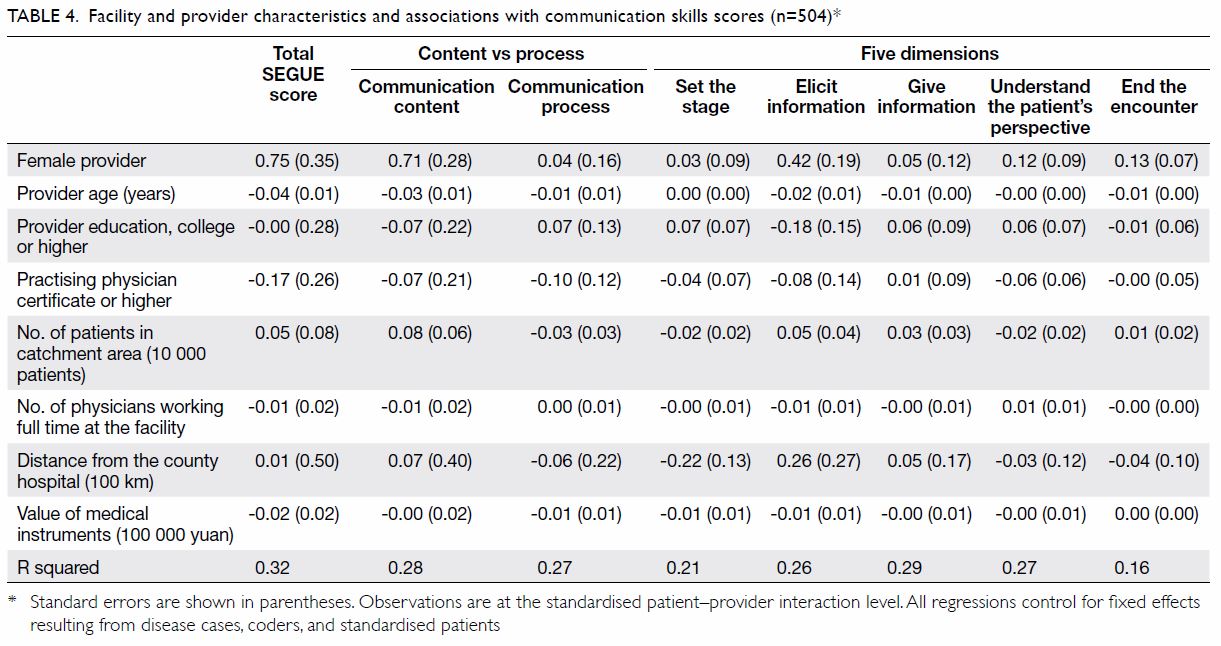
Table 4. Facility and provider characteristics and associations with communication skills scores (n=504)
Discussion
The results revealed that rural providers in China
had relatively poor communication skills overall,
especially in terms of understanding patients, caring
for them, and inviting patients to participate in
the interaction. Female and younger providers had
significantly higher overall communication scores,
even after controlling for fixed effects of SPs, disease
cases, and coders.
We found that rural providers in China had
relatively poor communication skills overall. They
performed poorly at most tasks involving patient
engagement during the encounter, such as inviting
them to discuss their questions and concerns.
In these cases, patients generally adopt a more
passive role, which could lead to inaccuracies
and inefficiencies when providers do not elicit
all information necessary to develop an effective
diagnosis and treatment plan.18 Moreover, while
rural providers generally maintained a respectful
tone throughout their patient encounters, they
seldom actively expressed understanding, care, or
concern.
Two possible explanations may account for the
rural providers’ poor communication skills. First, in
the past, medical students (ranging from those in-service
to those engaged in continuing education)
rarely received instruction in provider-patient
communication.19 20 21 According to a 2015 survey of
81 independent medical colleges, the proportion
of medical students who took provider-patient
communication courses was 61%, and the percentage
required to take compulsory communication
courses was only 27%.20 Thus, most currently
practising occupational health technicians have not
received systematic education in provider-patient
communication at an academic level.22 Training for
rural providers is more concerned with clinical skills
and medication knowledge and does not generally
involve provider-patient communication.23 This gap
has caused rural clinicians to have an insufficient
understanding of the importance of communication,
and their interpersonal abilities tend to be relatively
weak. Indeed, our data revealed no correlation
between education level and communication skills,
suggesting that further education does not improve
the providers’ methods of interacting with their
patients (Tables 3 and 4). Second, rural providers
have heavy workloads but low incomes compared with urban providers.24 25 Thus, they sometimes lack
enthusiasm for their work, are unwilling to give
patients humane care, and lack the motivation to
improve their communication skills.26 27 According
to survey data from providers in Chinese township
hospitals, income and provider-patient relationship
quality have positive impacts on rural providers’ job
satisfaction, and the provider-patient relationship
has strong endogeneity.28
Compared with the providers in townships,
the providers at village clinics were more likely to
make personal connections with their patients and
established a warmer and more accessible clinic
environment during the encounters. This result is
unsurprising, as township health centres serve a
patient population that is 13 times that of village
clinics (Table 1). Consequently, providers in villages
are more likely to develop longitudinal relationships
with their local patients and communities,
enabling greater knowledge of villagers’
socioeconomic backgrounds and more personable
communication.24 29
Our study also found that the providers’ gender
was associated with their level of communication
skills, especially in gathering information and
reviewing the next steps with patients. These results
are in line with a large body of literature that links
female gender with greater provider engagement
in patient concerns and asking more psychosocial
questions.30 31 These behaviours may stimulate
greater patient disclosure of aspects that are both
psychosocial and biomedical in nature. Thus,
although male and female providers did not differ
in the amount of information they provided to their
patients, the patients of female physicians collected
more biomedical information than those of male
providers.
Moreover, we found that younger providers
performed well in the two dimensions that are
directly related to diseases: eliciting or sharing
information, and reviewing the next steps with
patients. We conclude that greater experience may
not necessarily help providers to develop better
communication skills. One possible explanation is
that low income, heavy workload, lack of appreciation,
and restrictions on providers’ autonomy imposed
by hospital guidelines may contribute to fading
enthusiasm and burnout.32 33 Burnout may influence
the quality of care, resulting in more suboptimal
and less compassionate care.34 Older providers
who have been in their roles for longer periods are
more likely to experience emotional exhaustion.35
Therefore, although older providers have more
experience communicating with patients, they
do not necessarily communicate better. This is
consistent with previous findings indicating that
communication skill does not automatically develop
over time or with experience.36 37
Our study has three main limitations. First,
we evaluated providers’ communication skills
using audio recordings from concealed devices
rather than videos, which may have resulted in an
underestimation of providers’ communication skills
due to our sole reliance on verbal communication.
Second, although unannounced SPs may capture
actual provider behaviour more accurately, the
SPs themselves may not have accurately mimicked
actual patients, as they did not initially offer disease-related
information unless the providers asked for
it. However, any effects caused by the simulated
environment did not impact the comparisons
between different types of providers. We also
increased the accuracy of our observation of the
providers’ communication behaviour by excluding
any influence of the patient’s communication ability
on the provider. Finally, the physician-patient
relationship in the Asian context has historically been
described as more paternalistic than that in Western
countries.38 Thus, the SEGUE scale, which was based
on a Western model, may not be completely suitable
for measuring Chinese providers’ communication
skills. However, as increasing numbers of patients
and providers are recognising the importance of
‘patient-centred’ communication,21 39 the SEGUE
Framework is an effective tool for understanding the
characteristics of rural providers’ communication
skills in most regards.
Conclusion
The study revealed that providers in rural China have
poor communication skills overall. These deficits in
communication skills were especially pronounced
when providers were required to ‘Understand the
patient’s perspective’ and ‘End the encounter.’ They
asked about basic symptoms but rarely took the
initiative to invite patients to participate in the
encounter or discuss their questions and concerns,
and they also rarely showed care for the patients
themselves. Moreover, we found that the providers
from village clinics were more likely to make personal
connections with their patients. Female and younger
providers exhibited better communication skills,
asked more follow-up questions, and explained
future plans and steps more frequently than their
male and older counterparts.
Author contributions
Concept or design: Q Zhou, J Yang, J Nie, H Xue.
Acquisition of data: Q Zhou, Q An, N Wang, J Li, Q Gao, H Xue.
Analysis or interpretation of data: Q Zhou, J Li, Y Gao, J Yang, J Nie, H Xue.
Drafting of the manuscript: Q Zhou, J Yang.
Critical revision of the manuscript for important intellectual content: All authors.
Acquisition of data: Q Zhou, Q An, N Wang, J Li, Q Gao, H Xue.
Analysis or interpretation of data: Q Zhou, J Li, Y Gao, J Yang, J Nie, H Xue.
Drafting of the manuscript: Q Zhou, J Yang.
Critical revision of the manuscript for important intellectual content: All authors.
Conflicts of interest
All authors have disclosed no conflicts of interest.
Acknowledgement
The authors thank the standardised patients and coders for their hard work.
Funding/support
The authors are supported by the 111 Project (Grant No.
B16031), Laboratory of Modern Teaching Technology of the
Ministry of Education, Shaanxi Normal University, National
Natural Science Foundation of China (Grant No. 71703083),
the National Social Science Fund Youth Project (Grant No.
15CJL005), the National Natural Science Foundation of
China (Grant No. 71703084), and the Knowledge for Change
Program at The World Bank (Grant No. 7172469).
Ethics approval
Approval was obtained from the Institutional Review Boards of Stanford University, United States (Protocol no. 25904) and
Sichuan University, China (Protocol no. K2015025).
References
1. Orth JE, Stiles WB, Scherwitz L, Hennrikus D, Vallbona
C. Patient exposition and provider explanation in routine
interviews and hypertensive patients’ blood pressure
control. Health Psychol 1987;6:29-42. Crossref
2. Ward MM, Sundaramurthy S, Lotstein D, Bush TM,
Neuwelt CM, Street RL Jr. Participatory patient-physician
communication and morbidity in patients with systemic
lupus erythematosus. Arthritis Rheum 2003;49:810-8. Crossref
3. Mafinejad MK, Rastegarpanah M, Moosavi F, Shirazi
M. Training and validation of standardized patients
for assessing communication and counseling skills of
pharmacy students: a pilot study. J Res Pharm Pract
2017;6:83-8. Crossref
4. Henman MJ, Butow PN, Brown RF, Boyle F, Tattersall
MH. Lay constructions of decision-making in cancer.
Psychooncology 2002;11:295-306. Crossref
5. van Osch M, van Dulmen S, van Vliet L, Bensing J.
Specifying the effects of physician’s communication on
patients’ outcomes: a randomised controlled trial. Patient
Educ Couns 2017;100:1482-9. Crossref
6. Levinson W, Roter DL, Mullooly JP, Dull VT, Frankel RM.
Physician-patient communication. The relationship with
malpractice claims among primary care physicians and
surgeons. JAMA 1997;277:553-9. Crossref
7. Babiarz KS, Miller G, Yi H, Zhang L, Rozelle S. China’s
new cooperative medical scheme improved finances of
township health centers but not the number of patients
served. Health Aff (Millwood) 2012;31:1065-74. Crossref
8. National Bureau of Statistics, PRC Government. National
Bureau of Statistics. 2018. Available from: http://www.
stats.gov.cn/. Accessed 7 Jun 2019.
9. Shi Y, Xue H, Wang H, Sylvia S, Medina A, Rozelle S.
Measuring the quality of doctors’ health care in rural
China: an empirical research using standardized patients
[in Chinese]. Studies in Labor Econ 2016;4:48-71.
10. Xue H, Shi Y, Huang L, et al. Diagnostic ability and
inappropriate antibiotic prescriptions: a quasi-experimental
study of primary care providers in rural China. J Antimicrob Chemother 2019;74:256-63. Crossref
11. Li J. Using the SEGUE Framework to assess Chinese
medical students’ communication skills in history-taking
[in Chinese]. Dissertation. China Medical University.
2008. Available from: https://kns.cnki.net/KCMS/detail/
detail.aspx?dbcode=CMFD&dbname=CMFD2008&filena
me=2008082494.nh. Accessed 7 Jun 2019.
12. Li H, Li D, Wang J, et al. Assessment on doctor-patient
communication skills of medical students with SEGUE
framework scale [in Chinese]. Hospital Manage Forum
2016;33:29-30.
13. Xu T, Dong E, Liu W, Liang Y, Bao Y. Reliability and validity
of the Chinese version of the Liverpool Communication
Skills Assessment Scale [in Chinese]. Chin Mental Health J
2013;27:829-33. Crossref
14. Shen L, Sun G. Assessment pf physician-patient
communication skills in practicing physicians by SEGUE
framework [in Chinese]. Chin Gen Pract 2017;20:1998-
2002.
15. Zhao T, Zou X, Zhou H, Ma H. General practitioner-patient
communications in outpatient clinic settings in
Beijing [in Chinese]. Chin Gen Pract 2019;22:413-6.
16. Makoul G. The SEGUE Framework for teaching and
assessing communication skills. Patient Educ Couns
2001;45:23-34. Crossref
17. Makoul G. Essential elements of communication in
medical encounters: the Kalamazoo consensus statement.
Acad Med 2001;76:390-3. Crossref
18. Beckman HB, Frankel RM. The effect of physician behavior
on the collection of data. Ann Intern Med 1984;101:692-6. Crossref
19. Li S, Liu Y. The achievements, problems and experiences
of the health services development in China’s 30-year
reform and opening-up [in Chinese]. Chin J Health Policy
2008;1:3-8.
20. Liu H, Shen C. Investigation report on educational
organization status of humanistic medicine in independent
medical universities [in Chinese]. Med Philos (A)
2015;36:13-8, 50.
21. Liu X, Rohrer W, Luo A, Fang Z, He T, Xie W. Doctorpatient
communication skills training in mainland China:
a systematic review of the literature. Patient Educ Couns
2015;98:3-14. Crossref
22. Guo L, Wang H, Zeng Q, et al. Exploration and practice of
the ways of cultivating communication and communication
ability of rural doctors [in Chinese]. Chin Rural Health
Serv Adm 2011;31:1017-8.
23. Song J, Yin W, Feng Z, et al. A study on-job-training status
and demand of rural doctors in Shandong Province [in
Chinese]. Chin Health Serv Manage 2017;34:378-80.
24. Hung LM, Shi L, Wang H, Nie X, Meng Q. Chinese primary
care providers and motivating factors on performance.
Fam Pract 2013;30:576-86. Crossref
25. Xue H, Shi Y, Medina A. Who are rural China’s village clinicians? Chin Agric Econ Rev 2016;8:662-76. Crossref
26. Campbell N, McAllister L, Eley D. The influence of
motivation in recruitment and retention of rural and
remote allied health professionals: a literature review.
Rural Remote Health 2012;12:1900.
27. Sun K, Yin W, Huang D, Yu Q, Zhao Y, Li Y. The effect of
income on occupation mentality of rural doctors under the
situation of new medical reform. Chin Health Serv Manage
2016;33:371-3.
28. Dong X, Ariana P. Why are rural doctors not satisfied with
their work? An empirical study on job income, doctorpatient
relationship and job satisfaction. Manage World
2012;(11):77-88.
29. Haddad S, Fournier P, Machouf N, Yatara F. What does
quality mean to lay people? Community perceptions
of primary health care services in Guinea. Soc Sci Med
1998;47:381-94. Crossref
30. Roter DL, Hall JA. Physician gender and patient-centered
communication: a critical review of empirical research.
Annu Rev Public Health 2004;25:497-519. Crossref
31. Swygert KA, Cuddy MM, van Zanten M, Haist SA, Jobe
AC. Gender differences in examinee performance on the
Step 2 Clinical Skills data gathering (DG) and patient note
(PN) components. Adv Health Sci Educ Theory Pract
2012;17:557-71. Crossref
32. Hojat M, Vergare MJ, Maxwell K, et al. The devil is in the
third year: a longitudinal study of erosion of empathy in
medical school. Acad Med 2009;84:1182-91. Crossref
33. Shanafelt TD, Gradishar WJ, Kosty M, et al. Burnout and
career satisfaction among US oncologists. J Clin Oncol
2014;32:678-86. Crossref
34. Dyrbye LN, Massie FS Jr, Eacker A, et al. Relationship
between burnout and professional conduct and attitudes
among US medical students. JAMA 2010;304:1173-80. Crossref
35. Yin S, Zhao J, Chen R. Empathy fatigue of clinical doctors
and its influencing factors. Chin Gen Pract 2016;19:206-9.
36. Kosunen E. Teaching a patient-centred approach and
communication skills needs to be extended to clinical
and postgraduate training: a challenge to general practice.
Scandi J Prim Health Care 2008;26:1-2. Crossref
37. Skoglund K, Holmström IK, Sundler AJ, Hammar LM.
Previous work experience and age do not affect final
semester nursing student self-efficacy in communication
skills. Nurse Educ Today 2018;68:182-7. Crossref
38. Ishikawa H, Takayama T, Yamazaki Y, Seki Y, Katsumata
N, Aoki Y. The interaction between physician and patient
communication behaviors in Japanese cancer consultations
and the influence of personal and consultation
characteristics. Patient Educ Couns 2002;46:277-85. Crossref
39. Ting X, Yong B, Yin L, Mi T. Patient perception and the
barriers to practicing patient-centered communication:
a survey and in-depth interview of Chinese patients and
physicians. Patient Educ Couns 2016;99:364-9. Crossref