Hong Kong Med J 2020 Feb;26(1):10–8 | Epub 22 Jan 2020
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Second tier non-invasive prenatal testing in a regional
prenatal diagnosis service unit: a retrospective analysis and literature
review
Vivian KS Ng, MB, ChB, FHKAM (Obstetrics and
Gynaecology)1; Avis L Chan, MB, BS, FHKAM (Obstetrics and
Gynaecology)1,2; WL Lau, MB, BS, FHKAM (Obstetrics and
Gynaecology)1; WC Leung, MD, FHKAM (Obstetrics and Gynaecology)1
1 Department of Obstetrics and
Gynaecology, Kwong Wah Hospital, Yaumatei, Hong Kong
2 Department of Pediatrics, Stanford
University School of Medicine, Palo Alto, California, United States
Corresponding author: Dr Vivian KS Ng (vivian_nks@hotmail.com)
Abstract
Introduction: The Hong Kong Hospital Authority has newly introduced a new Down's syndrome screening algorithm that offers free-of-charge non-invasive prenatal testing (NIPT) to women who screen as high risk. In preparation for this public-funded second tier NIPT service, the present study was conducted to retrospectively analyse women eligible for NIPT and to review the local literature.
Methods: Our retrospective study included women screened as high risk for Down's syndrome (adjusted term risk ≥1:250) during the period of 1 January 2015 to 31 December 2016. We performed descriptive statistics and multivariable logistic regression to examine the factors associated with women’s choice between NIPT and invasive testing. We also reviewed existing local literature about second tier NIPT.
Results: The study included 525 women who screened positive: 67% chose NIPT; 31% chose invasive diagnostic tests; and 2% declined further testing. Our literature review showed that in non-research (self-financed NIPT) settings, NIPT uptake rates have been increasing since 2011. Nulliparity, first trimester status, higher education, maternal employment, and conception by assisted reproductive technology are common factors associated with self-financed NIPT after positive screening. Among women choosing NIPT, the rates of abnormal results have typically been around 8% in studies performed in Hong Kong.
Conclusion: Implementation of second tier NIPT in the public setting is believed to be able to improve quality of care. We expect that the public in Hong Kong will welcome the new policy.
New knowledge added by this study
- A comprehensive review of all local studies in Hong Kong (including ours) that summarise the increasing trend of women choosing second tier non-invasive prenatal testing (NIPT) after high-risk Down's syndrome screening results; factors associated with choice of NIPT; and the percentages of abnormal NIPT results.
- The new Hospital Authority policy of offering publicly funded second tier NIPT for high-risk Down’s syndrome screening results will be feasible, beneficial, and welcomed by pregnant women and their partners.
Introduction
Prenatal diagnostic tests for Down’s syndrome have
been changing dramatically in recent decades. In the 1990s, women aged ≥35
years at confinement of pregnancy were regarded as the ‘high-risk’ group
in terms of carrying babies with Down’s syndrome. They were offered direct
invasive procedures that involved using a needle to puncture the amniotic
sac (amniocentesis) or placenta (chorionic villus sampling) to rule out
chromosomal abnormalities. Although these tests are diagnostic and
accurate, they have procedure-related miscarriage risks of 1/100 to 1/200.1 Indeed, the majority of these
cases undergoing such invasive procedures are normal pregnancies, and this
age-based approach imposed avoidable risks on otherwise normal babies.
Later, Down’s syndrome screening for nuchal translucency (NT) and maternal
serum markers was introduced to women of advanced maternal age (≥35
years). Since 1 July 2010, universal Down’s syndrome screening has been
offered in all public obstetrics units in Hong Kong.2 All pregnant women at appropriate gestation are offered
informed prenatal screening choices irrespective of their age. Those women
who are screened as high risk (adjusted term risk ≥1:250) were counselled
for either invasive diagnostic prenatal tests (chorionic villus sampling
versus amniocentesis) or expectant management without further tests.
Ultrasound examination for fetal abnormalities was performed regardless of
women’s choices. This measure has significantly reduced unnecessary
invasive procedures for women of advanced maternal age without introducing
any other risk factors.3 However,
the sensitivity and specificity of first or second trimester Down’s syndrome
screening tests are only about 90%,4
and false positive cases and accidental findings of chromosomal and
structural abnormalities may put women at risk of further unnecessary
procedures.
The discovery of the presence of cell-free fetal
DNA in maternal plasma by Professor Dennis Lo in 1997 was a remarkable
breakthrough in prenatal screening.5
6 7
In 2011, non-invasive prenatal testing (NIPT) became commercially
available in Hong Kong as a self-financed examination. Following positive
Down’s syndrome screening, women are now given an additional choice, NIPT,
in addition to the traditional approach with either invasive diagnostic
procedures or expectant management. The introduction of this technology
has made a significant impact on choices and decisions by obstetricians,
healthcare policy makers, and pregnant women.8
Compared with conventional screening, which has a
90% detection rate of Down’s syndrome and a 5% false positive rate,1 NIPT achieves a higher detection rate (99%) and a lower
false positive rate (as low as 0.1%).9
Even though NIPT costs >HK$5000, it is generally accepted by clinicians
and pregnant women because of its accuracy and safety. In December 2019,
the Hong Kong Hospital Authority introduced a publicly funded
(free-of-charge) second tier of NIPT to pregnant women who are screened
positive/high risk by the Down’s syndrome screening tests. While
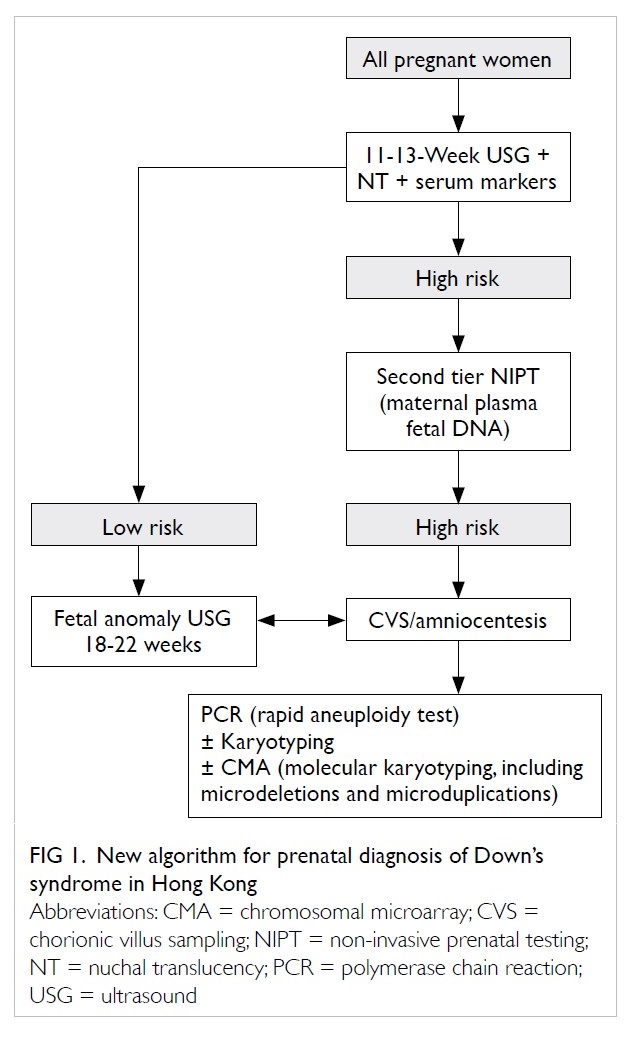
transitioning to the new healthcare policy (Fig 1), we performed this study to analyse data from
a large sample in our centre (which has approximately 5000 annual
deliveries) and summarise local NIPT study findings from Hong Kong. We
hypothesised that the general population and healthcare providers in Hong
Kong are ready for and supportive of the new policy and that the
prospective NIPT uptake rate will be very high.
Methods
This retrospective cohort study was conducted in a
government-funded regional obstetrics unit in Hong Kong that manages
approximately 5000 annual deliveries. All women who presented to our
obstetrics unit were eligible for Down’s syndrome screening, should their
gestation meet the screening criteria. The Down’s syndrome screening
programme is funded by the government and therefore free of charge to all
registered pregnant women. Pregnant women are offered either first
trimester combined Down’s syndrome screening at 11 to 13 weeks of gestation
or second trimester screening at 16 to 19 weeks of gestation. In all
Hospital Authority units, first trimester combined Down’s syndrome screening
measures and analyses the woman’s age, NT thickness, pregnancy-associated
plasma protein A, and free beta human chorionic gonadotropin, while second
trimester biochemical screening includes the woman’s age, total human
chorionic gonadotropin, alpha-fetoprotein, and unconjugated estriol (uE3)
[uE3 has been included in biochemical screening since late 2016 to improve
screening detection rates of trisomy 13, 18, and 21]. The result is
regarded as high risk if the adjusted term risk ratio for trisomy 21, 18,
and/or 13 is ≥1:250. Women who are screened as high risk are notified and
counselled for further management options by trained nurses or midwives
who are certified for ultrasound scanning by the Hospital Authority and
Fetal Medicine Foundation. These women are offered the following informed
choices: (1) publicly funded invasive tests; (2) self-financed NIPT; or
(3) decline further tests. The procedure-related risks of miscarriage are
quoted as 1% in chorionic villus sampling and 0.5% in amniocentesis.1 In the presence of thickened NT, especially those ≥3.5
mm, women were offered the option of direct invasive testing, as that
finding indicates an increased risk of microdeletions or
microduplications. Regardless of their choices, detailed ultrasound
examination is arranged at 19 to 22 weeks of gestation in women screened
as high risk to screen for any fetal structural abnormalities. If
ultrasound abnormalities are detected, women who have chosen NIPT or
declined further tests are counselled again for invasive diagnostic tests
to rule out chromosomal or genetic abnormalities.
Pregnant women screened with high-risk results for
trisomy 21, 18, and/or 13 by the universal Down’s syndrome screening
programme during the period of 1 January 2015 to 31 December 2016 (2
years) were included in this study. We retrieved their demographic
(maternal age, education level, race) and clinical (obstetric history,
history of abnormal pregnancy, family history, ultrasound findings, Down's
syndrome screening test results, woman’s choice of further tests after
positive screening) details from the Clinical Management System,
Electronic Patient Record, Antenatal Record System, and our written
records. Descriptive data (counts and percentages) were presented in
tables and flowcharts. Bivariate analysis of Chi squared or Fisher’s exact
tests was performed to identify factors associated with women’s choice
between NIPT and invasive tests. Two-tailed P values <0.05 were
considered statistically significant. We included all statistically
significant factors in a multivariable logistic regression model with
woman’s choice as the outcome. Variables that remained statistically
significant were regarded as factors that were independently associated
with the woman’s choice. The hypothesis was tested by comparing our
study’s results with the findings of other studies in Hong Kong about NIPT
uptake over time. Data were analysed using SPSS (Windows version 23.0; IBM
Corp, Armonk [NY], United States).
Results
From 1 January 2015 to 31 December 2016, 9276 women
underwent Down’s syndrome screening in our unit. A total of 525 (6%) women
were screened positive or at high risk of trisomy 21, 18, and/or 13. Table
1 shows the demographic and clinical characteristics of the screened
positive women in our study. Among them, 318 (61%) women were aged ≥35
years at their estimated date of confinement. Almost all women were
Chinese (512/525, 98%), and the remaining women were from a variety of
races. Regarding education level, almost half of these women (49%) had
achieved secondary school level, and one third had achieved tertiary
school level. The education level of 12% of them was unknown. The vast
majority of women (>95%) in this study had no significant family
history or personal history of abnormal pregnancy or genetic diseases.
Those with significant family history or personal history of abnormal
pregnancy were family history of mental retardation (n=2), trisomy 21
(n=1), Emmanuel syndrome (n=1), and not specified (n=1). Around one third
of women in this study had gravidity ≥3 (37%), and nearly half of them
were nulliparous (46%). Most of them were conceived naturally (94%).
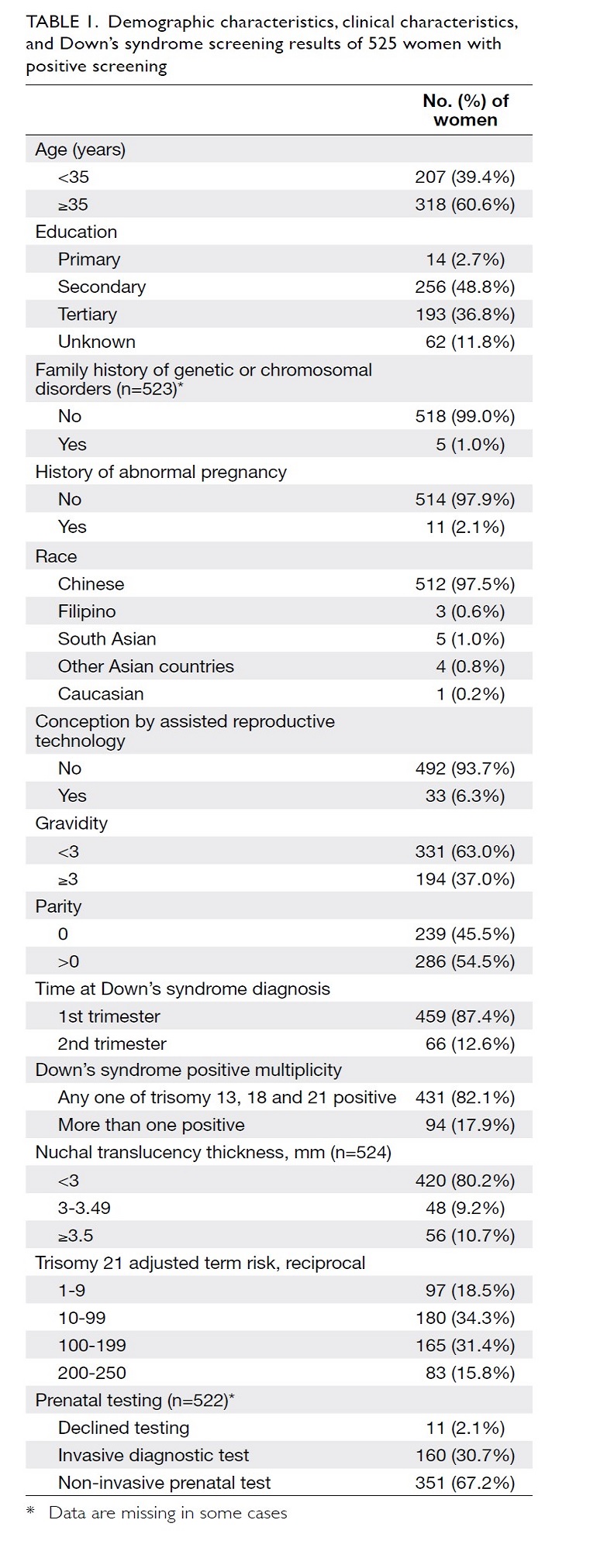
Table 1. Demographic characteristics, clinical characteristics, and Down’s syndrome screening results of 525 women with positive screening
For the index pregnancy, 459 (87%) women and 66
(13%) women had the Down’s syndrome screening performed during the first and
second trimester, respectively. Over 80% of screened positive women was
positive for any one of trisomy 21, 18, or 13. For those with NT measured
in the screening, 80% of women had NT <3 mm, and 10% had NT of ≥3.5 mm.
The distribution of the trisomy 21 risk ratio was uniform and even.
After high-risk results from Down’s syndrome
screening, 67% of women chose NIPT; 31% chose invasive diagnostic tests;
and 2% declined further testing. Figure 2 shows a detailed flowchart of women’s
decisions for further testing upon positive Down’s syndrome screening. Out
of 351 women who opted for NIPT after high-risk screening results, 328
(93%) had normal NIPT results, while 23 (7%) had abnormal results. The
abnormal results included trisomy 21, trisomy 18, trisomy 13, sex
chromosome-related, others (69XXX; dup (3q26.1-q29,31M) and del
(5q15.33-p14.1,22M); increased uptake chromosome 9), and non-reportable
(n=2). Of the 23 women with abnormal NIPT results, 21 proceeded to
invasive procedures; one miscarried prior to invasive procedures; and one
underwent termination of pregnancy directly. The diagnosis was confirmed
by diagnostic tests in 16 cases: 14 cases ended up with termination of
pregnancy; one continued pregnancy (47XYY); and one miscarried afterwards
(69XXX). The remaining five women who had invasive diagnostic tests
following high-risk NIPT (n=3) and non-reportable NIPT (n=2) were found
normal by karyotyping.
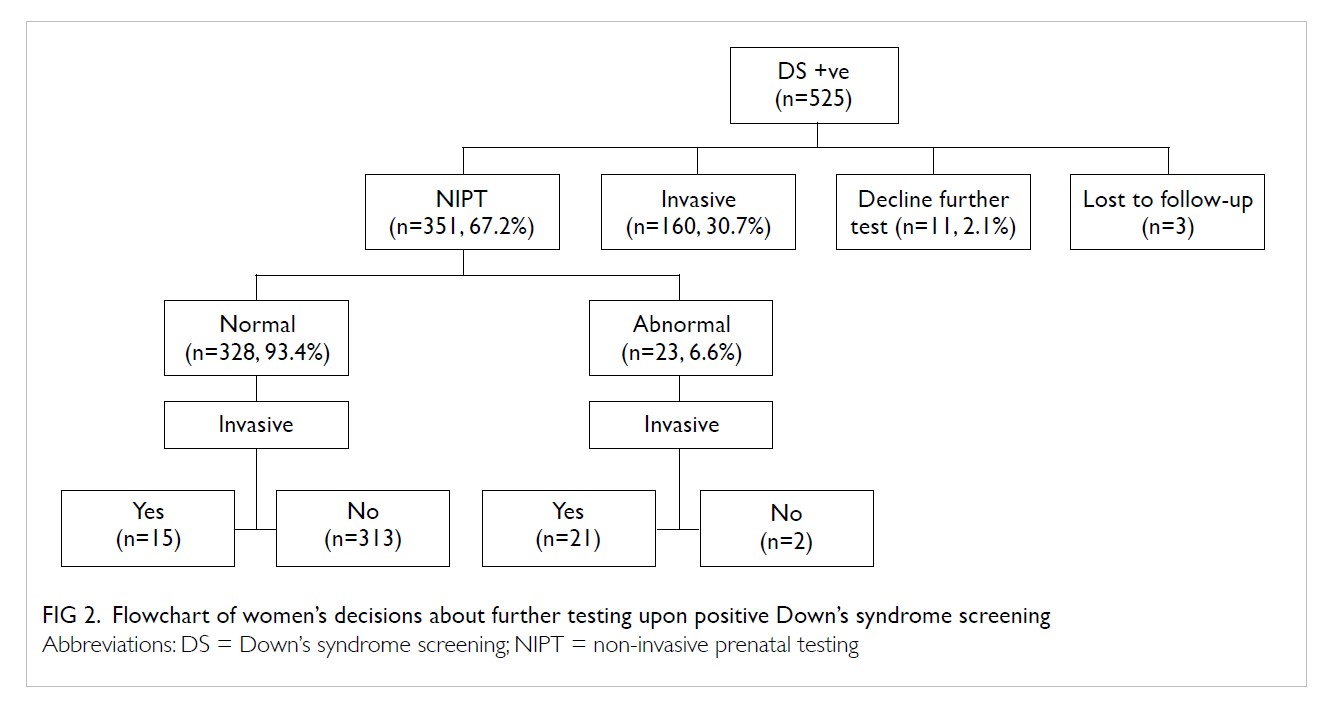
Figure 2. Flowchart of women’s decisions about further testing upon positive Down’s syndrome screening
There were 328 women with normal NIPT results.
However, 15 of them still required invasive procedures for reasons of
maternal anxiety (n=3), fetal gender confirmation (n=1), and sonographic
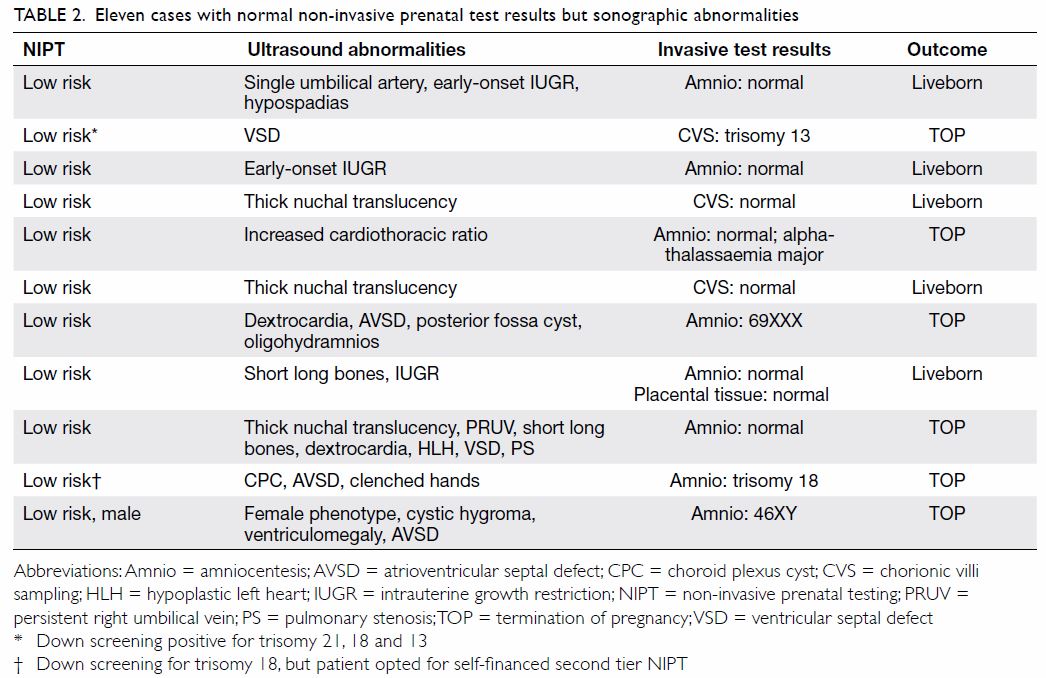
abnormalities detected during anomaly scans (n=11). The 11 women with
ultrasound abnormalities all proceeded to invasive procedures. The
ultrasound findings, karyotypes, and pregnancy outcomes of these women are
shown in Table 2.
Between women choosing NIPT and invasive diagnostic
procedures, the factors of maternal education, conception by assisted
reproductive technology, gravidity, parity, first trimester, trisomy
risks, and NT reached statistically significant difference (Table
3). After adjusting for all these variables in the logistic
regression model, only higher maternal education (P=0.04), gravidity <3
(P<0.001), nulliparity (P=0.03), and examination during the first
trimester (P<0.001) were associated with higher NIPT uptake.
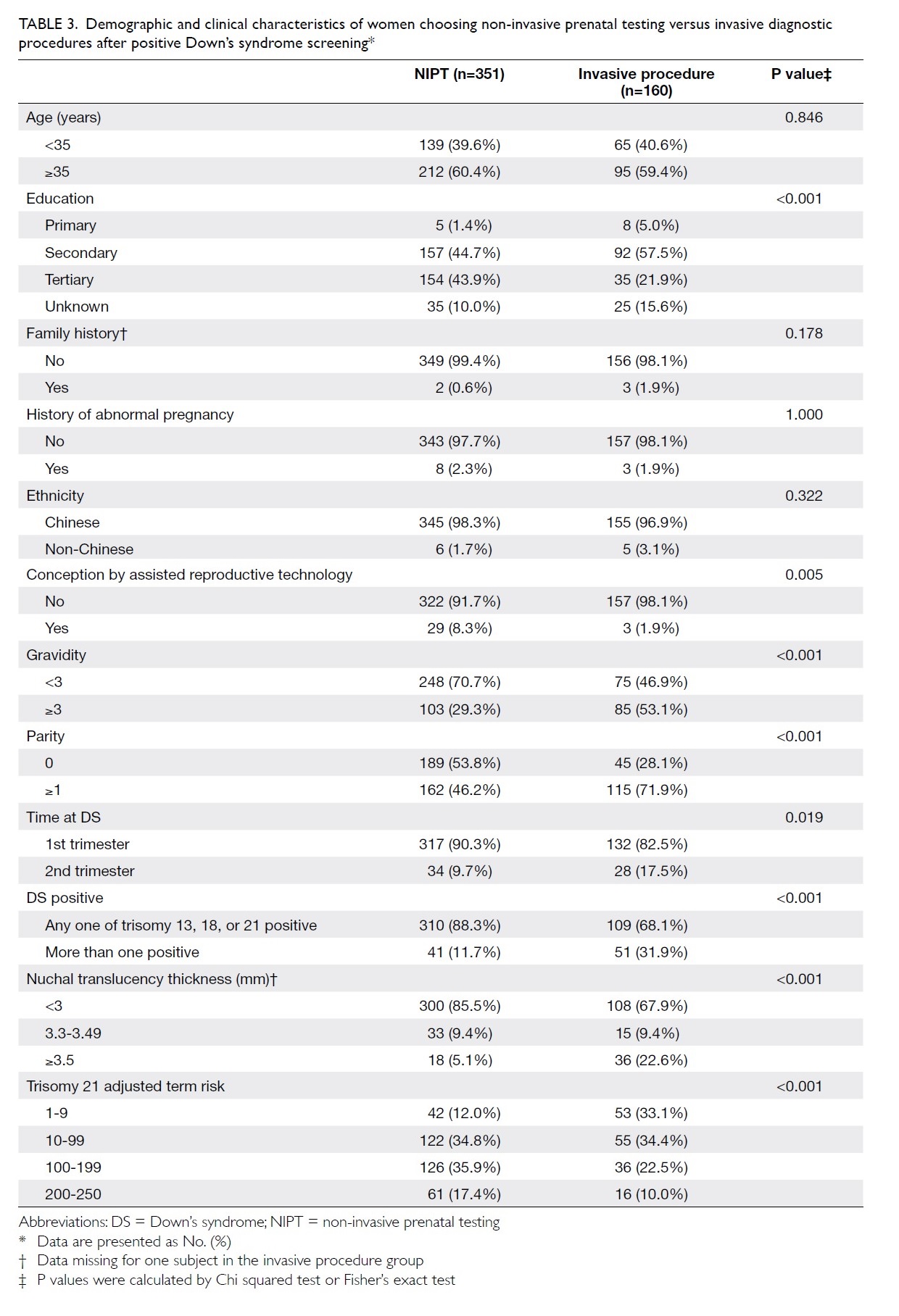
Table 3. Demographic and clinical characteristics of women choosing non-invasive prenatal testing versus invasive diagnostic procedures after positive Down’s syndrome screening
Discussion
Although NIPT was self-financed, increasing NIPT
uptake rates since 2011 reported by studies from Hong Kong support our
hypothesis that pregnant women are supportive of contingent NIPT after
positive Down’s syndrome screening tests. The uptake rate of self-financed NIPT has
increased from 20% (95% confidence interval [CI]=18%-24%; in Poon et al’s
study, 2011-201210) to 29% (95%
CI=26%-32%; in Chan et al’s study, 2012-201311)
to 67% (95% CI=63%-71%) in our study, 2015-2016. We observed a steep
increase in the NIPT uptake rate in our unit (from 23% in 2012 to 71% in
2016),12 and a corresponding rise
has been observed in other local public obstetrics units,13 despite the fact that women had to pay for the cost
of NIPT. A multi-centred survey-based study performed in Hong Kong showed
that >90% of women favouring NIPT after positive Down’s syndrome
screening were willing to pay for the test.14
This study also found that higher income was an independent predictor of
women’s choice for NIPT. Our study did not include household income
because the missing rate is very high (>50%). Low or non-response on
sensitive issues such as income and wealth has been well documented in the
literature.15 If cost is
eliminated as a factor, we would expect the majority of women to choose
NIPT as a contingent test, as projected by Lo et al13 in 2015-2016 and Cheng et al16
in 2015-2016. In those studies, NIPT was offered as a research expense,
and the uptake rates were 62% and 90%, respectively.13 16
Non-invasive prenatal testing is popular and widely
accepted in other parts of the world. The United Kingdom has the same
algorithm to manage women screened positive for Down’s syndrome, but outside
the research arena, NIPT is only available in the private sector at the
patient’s own expense. A study in the United Kingdom showed that the main
motivation for women choosing NIPT as a further test after positive Down's
syndrome screening was reassurance, as NIPT is safe, accurate, and able to
pick up those that may otherwise have been missed by combined Down's
syndrome screening.17 The
reassurance and reduction of anxiety made all women in the study believe
that NIPT should be adopted as part of the National Health System’s
obstetric practice. Another study in Australia also reported positive
experiences in women undergoing NIPT, with 93% of respondents indicating
support of public funding for NIPT as part of Down’s syndrome screening.18
In concordance with high acceptance of NIPT in Hong
Kong and worldwide, the number of invasive procedures has significantly
decreased recently. In our study, 328 (62%) women were able to avoid
unnecessary invasive diagnostic procedures that might have been performed
in historical clinical practice in public hospitals before NIPT and
current clinical practice if these pregnant women are not able to pay the
cost. Uptake may be much greater if NIPT is offered at no cost. Second
tier screening after positive combined first trimester screening
significantly reduced the number of invasive procedures performed and
increased specificity while maintaining close to 100% sensitivity.19 In addition, NIPT may provide a broader range of
information about microdeletions, microduplications, single-gene
disorders, etc. This provides additional options for women who prefer the
extended reports provided by NIPT if clinically indicated.20
Although NIPT is highly sensitive and specific in
detecting trisomies 21, 18, and 13, ultrasound still plays an important
complementary role in the contemplated algorithm for prenatal Down's
syndrome screening. Given normal NIPT results following positive Down's
syndrome screening, a number of women may also require invasive procedures
in the presence of sonographic abnormalities resulting from false negative
cases or non-aneuploidy diseases like thalassaemia (Table 2).
We reviewed the local data from studies in Hong
Kong regarding second tier NIPT after high-risk Down’s syndrome screening
results (Table 4 10
11 13
16 21).
Our study has the largest sample size in the last 5 years. The vast
majority of pregnant women presented to the obstetrics unit during the
first trimester and had first trimester combined Down’s syndrome screening
tests performed. In non-research (self-financed NIPT) settings, NIPT
uptake rates have been increasing since 2011. Nulliparity, first trimester
status, higher education, maternal employment, and conception by assisted
reproductive technology are common factors that have been independently
associated with self-financed NIPT after positive Down’s syndrome screening
tests. In our study, a multivariable logistic regression model indicated
that NT thickness and adjusted term risk ratio of trisomy 21 were no
longer statistically associated with NIPT uptake. We found that positive
Down’s syndrome screening results, adjusted term risk of trisomy 21, and NT were
correlated. By controlling for any one of these factors, the effects of
the other two factors could be held relatively constant. Moreover, NT
thickness is only reported in the first trimester, and therefore, the
effects of NT may be accounted for by the first trimester factor. Among
women choosing NIPT, the rate of abnormal results has typically been
around 8% in studies performed in Hong Kong.
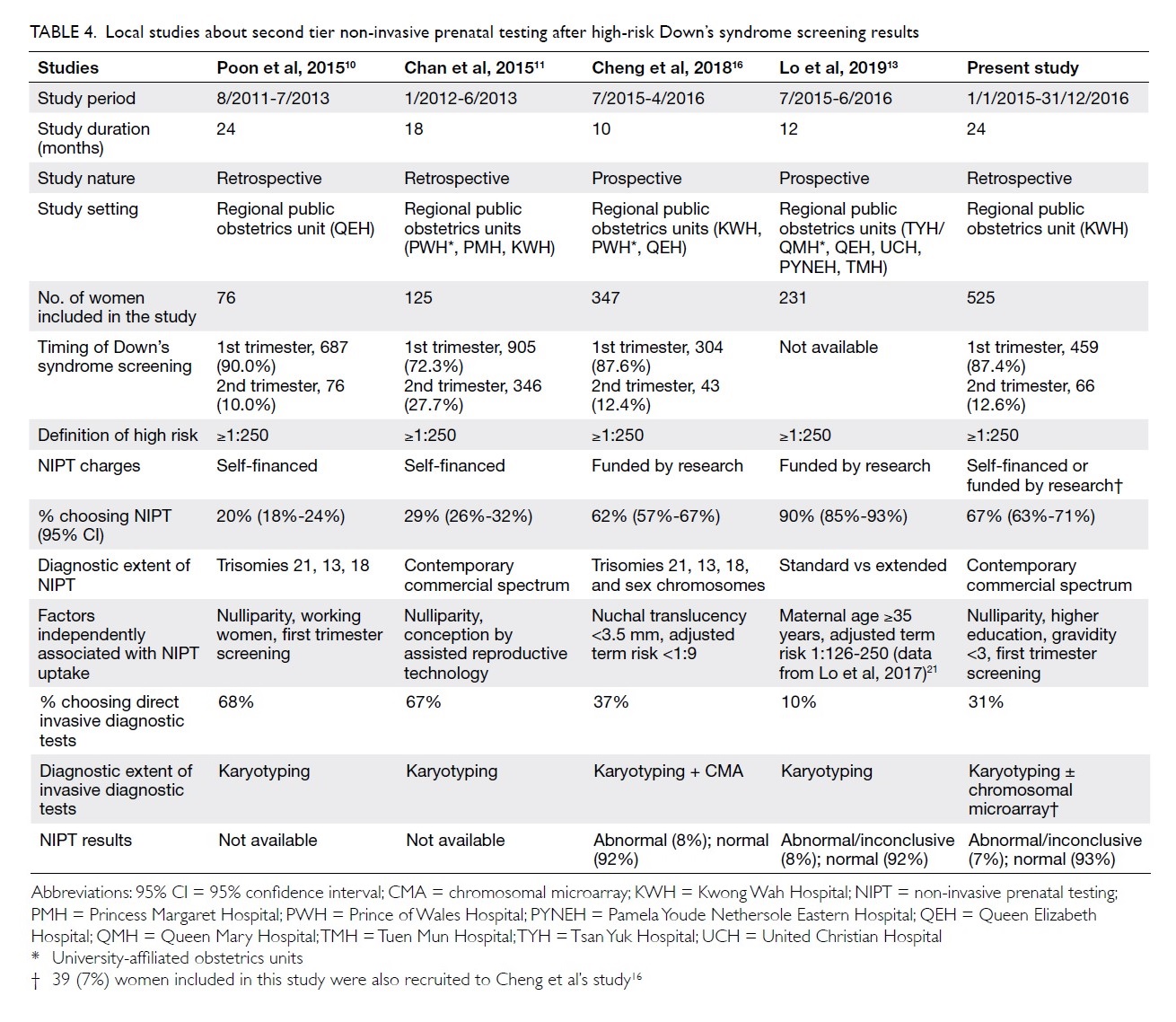
Table 4. Local studies about second tier non-invasive prenatal testing after high-risk Down’s syndrome screening results
Our study is limited by the retrospective nature of
the study and missing data on self-reported items like education level and
household income. Furthermore, obstetric professionals’ perceptions about
NIPT may vary among different healthcare providers, leading to potential
implicit bias.22 Studies have
found that obstetricians had more certain views about the usefulness of
NIPT than midwives had.23 To
consider this potential bias, a questionnaire to the healthcare providers
would be useful for understanding their perceptions, attitudes, and the
extent of any bias towards NIPT or invasive diagnostic procedures.
Standardised counselling materials (interview scripts, booklets, videos,
question and answer information sheets) distributed to women may also
minimise dynamic human factors during the counselling session.
Conclusion
Implementation of second tier NIPT in the public
setting is believed to improve quality of care, women’s choice, and
overall financial/budget performance.24
A significant number of unnecessary invasive procedures can be avoided. We
expect that the public in Hong Kong will welcome this new policy.
Author contributions
All authors had full access to the data,
contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Concept or design: VKS Ng.
Acquisition of data: VKS Ng.
Analysis or interpretation of data: VKS Ng.
Drafting of the article: VKS Ng.
Critical revision for important intellectual content: AL Chan, WL Lau, WC Leung.
Concept or design: VKS Ng.
Acquisition of data: VKS Ng.
Analysis or interpretation of data: VKS Ng.
Drafting of the article: VKS Ng.
Critical revision for important intellectual content: AL Chan, WL Lau, WC Leung.
Conflicts of interest
The authors have no conflicts of interest or
declarations to report regarding the present work.
Acknowledgement
The authors acknowledge the excellent work by staff
at the prenatal diagnostic clinic, Kwong Wah Hospital for their
outstanding service provision and patient care.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
This study protocol was reviewed and approved by
the Research Ethics Committee (Kowloon Central/Kowloon East) of the Hong
Kong Hospital Authority (Ref no. KC/KE-18-0123/ER-3). The requirement for
patient consent was waived by the Ethics Committee.
References
1. Benn P, Borrell A, Chiu RW, et al.
Position statement from the Chromosome Abnormality Screening Committee on
behalf of the Board of the International Society for Prenatal Diagnosis.
Prenat Diagn 2015;35:725-34. Crossref
2. Sahota DS, Leung WC, Chan WP, To WW, Lau
ET, Leung TY. Prospective assessment of the Hong Kong Hospital Authority
universal Down syndrome screening programme. Hong Kong Med J
2013;19:101-8.
3. Lo TK, Lai FK, Leung WC, et al.
Screening options for Down syndrome: how women choose in real clinical
setting. Prenat Diagn 2009;29:852-6. Crossref
4. Tu S, Rosenthal M, Wang D, Huang J, Chen
Y. Performance of prenatal screening using maternal serum and ultrasound
markers for Down syndrome in Chinese women: a systematic review and
meta-analysis. BJOG 2016;123 Suppl 3:12-22. Crossref
5. Lo YM, Corbetta N, Chamberlain PF, et
al. Presence of fetal DNA in maternal plasma and serum. Lancet
1997;350:485- 7. Crossref
6. Chiu RW, Chan KC, Gao Y, et al.
Noninvasive prenatal diagnosis of fetal chromosomal aneuploidy by
massively parallel genomic sequencing of DNA in maternal plasma. Proc Natl
Acad Sci U S A 2008;105:20458-63. Crossref
7. Chiu RW, Akolekar R, Zheng YW, et al.
Non-invasive prenatal assessment of trisomy 21 by multiplexed maternal
plasma DNA sequencing: large scale validity study. BMJ 2011;342:c7401. Crossref
8. Dondorp W, de Wert G, Bombard Y, et al.
Non-invasive prenatal testing for aneuploidy and beyond: Challenges of
responsible innovation in prenatal screening. Eur J Hum Genet
2015;23:1438-50. Crossref
9. Gil MM, Accurti V, Santacruz B, Plana
MN, Nicolaides KH. Analysis of cell-free DNA in maternal blood in
screening for aneuploidies: updated meta-analysis. Ultrasound Obstet
Gynecol 2017;50:302-14. Crossref
10. Poon CF, Tse WC, Kou KO, Leung KY.
Uptake of noninvasive prenatal testing in Chinese women following positive
down syndrome screening. Fetal Diagn Ther 2015;37:141-7. Crossref
11. Chan YM, Leung WC, Chan WP, Leung TY,
Cheng YK, Sahota DS. Women’s uptake of non-invasive DNA testing following
a high-risk screening test for trisomy 21 within a publicly funded
healthcare system: findings from a retrospective review. Prenat Diagn
2015;35:342-7. Crossref
12. Kwong Wah Hospital, Hospital
Authority, Hong Kong SAR Government. Annual Report 2012-2016, Department
of Obstetrics and Gynaecology, Kwong Wah Hospital.
13. Lo TK, Chan KY, Kan AS, et al.
Decision outcomes in women offered noninvasive prenatal test (NIPT) for
positive Down screening results. J Matern Neonatal Med 2019;32:348-50. Crossref
14. Lo TK, Chan KY, Kan AS, et al. Effect
of knowledge on women’s likely uptake of and willingness to pay for
non-invasive test (NIPT). Eur J Obstet Gynecol Reprod Biol 2018;222:183-4.
Crossref
15. Riphahn RT, Serfling O. Item
non-response on income and wealth questions. Empir Econ 2005;30:521-38. Crossref
16. Cheng Y, Leung WC, Leung TY, et al.
Women’s preference for non-invasive prenatal DNA testing versus
chromosomal microarray after screening for Down syndrome: a prospective
study. BJOG 2018;125:451-9. Crossref
17. Lewis C, Hill M, Chitty LS. Women’s
experiences and preferences for service delivery of non-invasive prenatal
testing for aneuploidy in a public health setting: a mixed methods study.
PLoS One 2016;11:e0153147. Crossref
18. Bowman-Smart H, Savulescu J, Mand C,
et al. ‘Small cost to pay for peace of mind’: women’s experiences with
non-invasive prenatal testing. Aust N Z J Obstet Gynaecol 2019;59:649-55.Crossref
19. Miltoft CB, Rode L, Ekelund CK, et al.
Contingent first-trimester screening for aneuploidies with cell-free DNA
in a Danish clinical setting. Ultrasound Obstet Gynecol 2018;54:470-9. Crossref
20. Lo TK, Chan KY, Kan AS, et al. Study
of the extent of information desired by women undergoing non-invasive
prenatal testing following positive prenatal Down-syndrome screening test
results. Int J Gynecol Obstet 2017;137:338-9. Crossref
21. Lo TK, Chan KY, Kan AS, et al.
Informed choice and decision making in women offered cell-free DNA
prenatal genetic screening. Prenat Diagn 2017;37:299-302. Crossref
22. FitzGerald C, Hurst S. Implicit bias
in healthcare professionals: a systematic review. BMC Med Ethics
2017;18:19. Crossref
23. Ngan OM, Yi H, Wong SY, Sahota D,
Ahmed S. Obstetric professionals’ perceptions of non-invasive prenatal
testing for Down syndrome: clinical usefulness compared with existing
tests and ethical implications. BMC Pregnancy Childbirth 2017;17:285. Crossref
24. Chitty LS, Wright D, Hill M, et al.
Uptake, outcomes, and costs of implementing non-invasive prenatal testing
for down syndrome into NHS maternity care: Prospective cohort study in
eight diverse maternity units. BMJ 2016;354:i3426. Crossref