© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
REMINISCENCE: ARTEFACTS FROM THE HONG KONG MUSEUM OF
MEDICAL SCIENCES
Drainage apparatus for treating pneumothorax
Harry YJ Wu, MD, DPhil
Medical Ethics and Humanities Unit, Li Ka Shing
Faculty of Medicine, The University of Hong Kong, Pokfulam, Hong Kong
This drainage apparatus (Fig), collected by the Hong Kong Museum of Medical
Sciences and stored in a custom wooden case, is not an uncommon artefact.
It does, however, tell a distinctive story of Hong Kong people’s lungs.
The apparatus was donated by Dr Chiu Kwong Yu in 1999 and consists of two
1-L glass bottles containing sterile solutions, each measuring 21 cm tall
and 11.50 cm in diameter. The fluid in two bottles has deteriorated over
time and become darkened. Attached to the case door is a glass barometer
about 26 cm long. Under the glass bottles is a small drawer that used to
contain consumables, such as syringes, needles, scalpels, and blades. The
apparatus was used as a closed drainage system, mainly for the treatment
of pneumothorax and other conditions that require chest drainage, such as
pleural effusion and haemothorax. The portable design made it a practical
device that could be operated at the bedside.
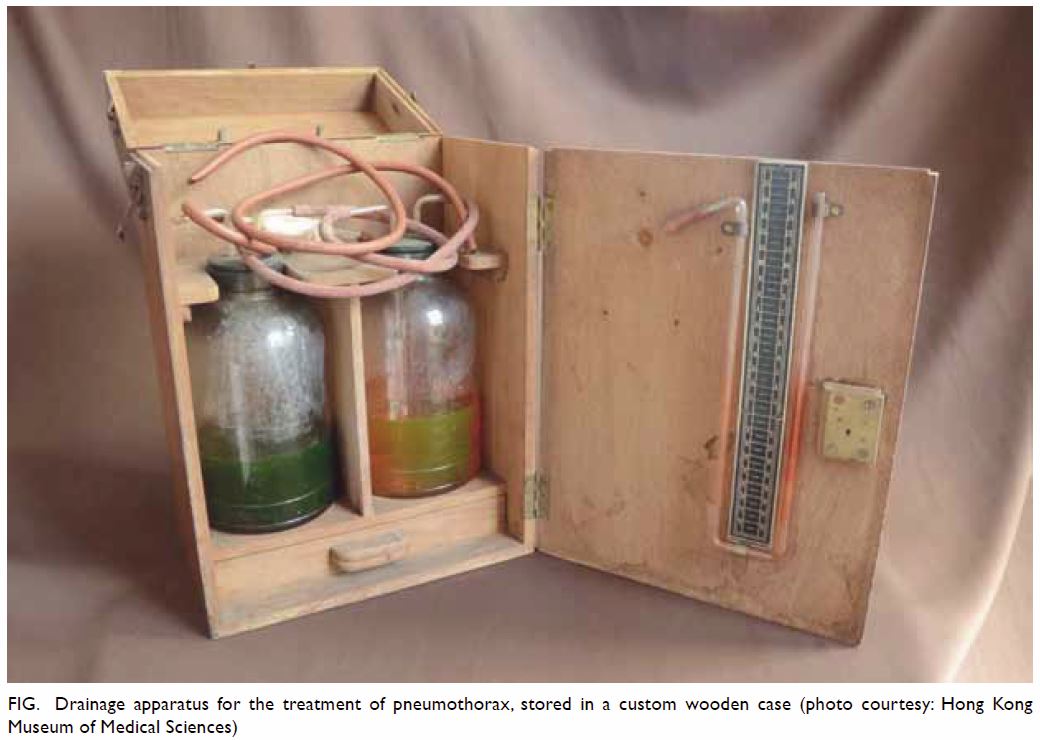
Figure. Drainage apparatus for the treatment of pneumothorax, stored in a custom wooden case (photo courtesy: Hong Kong Museum of Medical Sciences)
Pneumothorax is a common lung condition. When a
pneumothorax occurs, the negative pressure in the pleural cavity is
disrupted, resulting in respiratory distress. If the condition is mild, a
small amount of fluid or air may be absorbed by the body after sufficient
rest. However, in a more severe situation, a drainage system is required
to prevent the lung from collapsing. Such treatment, employing a siphon
effect, can be dated to the late 19th century. In one of the earliest
documented cases in 1875, the German internist Gotthard Bülau described
using drainage to treat an empyema as an alternative to the then-popular
rib resection. He first used a trocar to puncture the pleural space and
then introduced a rubber catheter with a distal clamp to create a closed
water-seal system. The end of the catheter was immersed in a bottle
one-third full of antiseptic solution and then unclamped, resulting in a
siphon drainage apparatus and allowing pus to flow from the chest cavity.1
In modern times, several basic components are
needed to drain the fluid or air out of a pleural cavity. This usually
comprises a closed sterile and disposable system containing one or
multiple chambers with a one-way valve that can prevent return of air or
fluid into the patient. The main part of the apparatus collected by the
museum was manufactured by Kelvin & Hughes, a British company still in
business that specialises in the design and manufacture of instruments
related to navigation. However, the spindle-shaped glass compartment
containing two Chinese characters shows clear signs that the entire
apparatus might be a convenient assemblage of various sources. It was
likely used most extensively in the 1960s; in 1963, closed thoracotomy
drainage with a Foley catheter and two-bottle suction system was advocated
as the preferred treatment for pneumothorax and significant haemothorax.2 While in use, the two bottles and
spindle-form glass device containing sterilised cotton wool were connected
by rubber tubes. One end of the apparatus connected the chest catheter
that was inserted into the patient’s pleura. The treatment could last from
1 day to 2 weeks, depending on how well the patient responded to the
procedure. X-ray plain films were sometimes useful for doctors to evaluate
the remaining air or fluid in the pleura.
In the early days of Hong Kong’s history, certain
populations were more prone to developing pneumothorax. Resulting from
poor sanitation and occupational hazards, these were mostly patients with
more fragile lung conditions, such as those living with tuberculosis or
pneumoconiosis. It is also worth noting that, from the 1930s to the 1950s,
pneumothorax was employed as a treatment for tuberculosis. Before the
advent of anti-tuberculosis drugs, there was no specific treatment for
this infection, although surgical treatment could be offered in some early
cases. In the 1930s, the three most commonly performed operations were
sectioning of the phrenic nerve, creation of an artificial pneumothorax,
and thoracoplasty by removal of some ribs.3
The Annual Medical Report of the government for 1934 reported that the
University Medical Unit at Government Civil Hospital had started a special
clinic for artificial pneumothorax of pulmonary tuberculosis cases.4 In 1938, artificial pneumothorax treatment was carried
out in all suitable male cases at Queen Mary Hospital with ‘gratifying
results’.5 Such treatment gradually
became less common in the 1950s, owing to the availability and
effectiveness of anti-tuberculosis medication. However, it is
understandable that pleural drainage might have continued to be used
extensively, because of the high incidence of pneumothorax and lung cavity
infection among the many tuberculosis patients at that time.
In modern times, treatment for pneumothorax is no
longer complex. Most spontaneous pneumothorax patients will recover with
sufficient bed rest and nutrition support. The most commonly used device
for drainage is a plastic three-chamber unit. These include a collection
chamber, a water-seal chamber, and a suction control chamber, which are
interconnected. Despite international guidelines now advocating the use of
simple aspiration and small-bore chest catheters, in Hong Kong,
intercostal chest tube insertion remains popular.6
Therefore, this drainage apparatus represents, not an outdated practice,
but conceivably only a change in materials.
References
1. Meyer JA. Gotthard Bülau and closed
water-seal drainage for empyema, 1875-1891. Ann Thorac Surg 1989;48:597-9.
https://doi.org/10.1016/S0003-4975(10)66876-2
2. Felton WL 2nd. Initial evaluation and
management of the patient with a chest injury. Am J Surg 1963;105:445-53.
Crossref
3. Li SF. Indications, contraindications
and end results in the surgical treatment of pulmonary TB. Caduceus
1931;10:167-77.
4. Wong TW. Plombage treatment for
pulmonary tuberculosis in Hong Kong. Hong Kong Med J 2014;20:268. Crossref
5. Wilkinson PB. Report of the University
Professorial Unit. Annual Medical Report for the Year Ending. 1938: 77.
6. Chan JW, Ko FW, Ng CK, et al. Management
of patients admitted with pneumothorax: a multi-centre study of the
practice and outcomes in Hong Kong. Hong Kong Med J 2009;15:427-33.

