© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
MEDICAL PRACTICE
High-fidelity simulation training programme for
final-year medical students: implications from the perceived learning
outcomes
YF Choi, FHKCEM, MSc(Clinical Education)(Edin)1,2,3;
TW Wong, FHKCEM, FHKAM (Emergency Medicine)1
1 Accident and Emergency Department,
Pamela Youde Nethersole Eastern Hospital, Chai Wan, Hong Kong
2 Programme Director, Nethersole
Clinical Simulation Training Centre, Hong Kong
3 Medical Director, Hong Kong Fire
Services Department, Hong Kong
Corresponding author: Dr YF Choi (choiyf@gmail.com)
Abstract
We designed a session of high-fidelity simulation
training course for final-year medical students in their emergency
medicine specialty clerkship. This was a new initiative with clearly
defined learning outcomes. We aimed to evaluate the learning outcomes.
Students completed an evaluation form at the end of the session focusing
on their perceived learning outcomes. Thematic analysis was conducted
for data processing. We collected responses from 149 students. In
addition to the intended outcomes of the course, students gained
unexpected learning outcomes from the training and some of them matched
a few identified learning gaps between undergraduate medical education
and their subsequent transition to early clinical practice that have
been described in the literature. High-fidelity simulation
training in medical school could be an effective tool to address some of
the identified gaps in the transition between undergraduate medical
education and postgraduate practice.
Introduction
Clinical simulation training has become more widely
practised in local hospitals and academic healthcare institutions in the
past decade, with a wide range of training modalities, from part-task
simulator to full-body manikin and from single skill training to
interprofessional team-based training.
The Nethersole Clinical Simulation Training Centre
is a hospital-based training centre which has advocated high-fidelity
multidisciplinary team training for hospital staff since its establishment
in 2012 in Pamela Youde Nethersole Eastern Hospital. From 2008, the
emergency department of the hospital was one of the centres for teaching
emergency medicine specialty clerkship medical students from one of the
medical schools in Hong Kong. In 2017, the emergency department
collaborated with the Nethersole Clinical Simulation Training Centre in an
initiative to design a high-fidelity simulation training session for
medical students.
In the past, medical students in local medical
school did not have much high-fidelity simulation training because medical
schools did not have high-fidelity training facilities. Furthermore, it
was conventionally believed that high-fidelity simulation training is more
beneficial for expert-level learners and that low-fidelity training was
more suitable for beginners, because the sophisticated context in the
high-fidelity environment might potentially jeopardise learning objectives
by creating excessive cognitive burden.1
2 3
Medical students, owing to their low clinical exposure, were regarded as
beginners.
However, a recent study suggested that once medical
students have learnt some basic skills, high-fidelity simulation training
might benefit learners through psychological immersion, despite the extra
cognitive burden.4 Therefore, we
decided to trial high-fidelity simulation training for final-year medical
students, who have already completed most of their academic studies and
have acquired some basic practical skills.
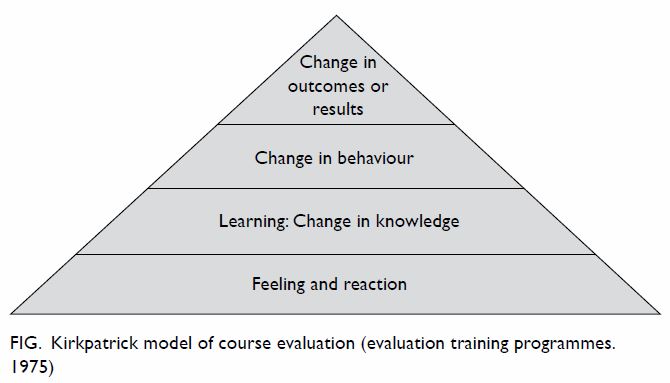
The prototype of the simulation training course was
started in 2017 and at that time we mainly evaluated the “reaction” phase
of the learners which is the basic level of outcome evaluation according
to Kirkpatrick’s model (Fig). The feedback from the students was very
positive and they welcomed the course very much.5
Encouraged by this, we revised the course material in 2018 with written
intended learning outcomes. In the present study, we evaluate “learning”,
which is a level higher in the Kirkpatrick’s model.
The aim of the present study was to evaluate the
learning outcomes of a high-fidelity simulation training course for
final-year medical students.
Methods
Design
This was a qualitative study by a survey in
English. The contents were checked against SRQR reporting guideline
(Standards for Reporting Qualitative Research 2016 version).
Setting
The training course was conducted in the Nethersole
Clinical Simulation Training Centre that has a simulation training suite
with isolated simulation rooms and a debriefing room. The simulation rooms
are equipped with ceiling-mounted cameras for video-assisted debriefing.
The simulation room used was prepared to resemble the environment of a
resuscitation room in the emergency department with a full-body
high-fidelity manikin.
Course design
The training course consisted of a brief
introduction followed by four short case scenarios in a 3-hour session. In
the introduction, students were briefed about course structure, learning
objectives, and clinical simulation rules and underwent a short simulation
laboratory familiarisation session. A group of seven to eight students
further divided into two subgroups played the four scenarios in turn.
While one subgroup was doing the scenario, the other subgroup observed
from the debriefing room via the audio-visual system. The instructor wore
a nurse uniform and acted as an experienced nurse in the scenarios, which
included no real-time coaching. In the four scenarios all the patients
presented with acute or even life-threatening conditions that need prompt
treatment. Such a design simulated the high psychological fidelity of real
life. Participants had to treat the patients on their own with no guidance
from the instructor. A debriefing session was carried out immediately
after each scenario.
Data collection
A cohort of student participants in 2018 were
selected by convenience sampling and they were asked to complete an
evaluation form immediately after the session. The evaluation form invited
the students to offer free text only with no rating scale. They could
write up to three perceived learning outcomes, up to three reflections
after the course and any extra comments or suggestions about the course.
There was no space to enter the name of the students, so the data
collection was completely anonymous.
Data analysis
The findings in the evaluation form were processed
through thematic analysis shortly after each course and compared with the
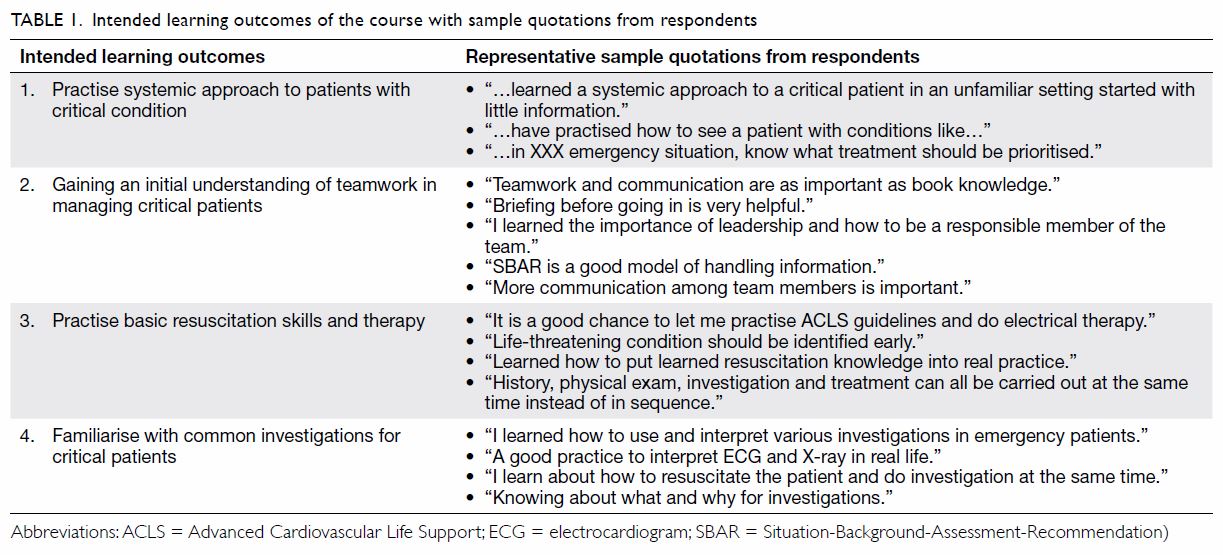
intended learning outcomes of the course (Table 1). The intended learning outcomes were
designed to include both clinical learning outcomes and teamwork learning
outcomes such as briefing, debriefing, communication, situation awareness,
and leadership. The clinical learning outcomes, owing to their diversity
were further divided into three separate categories (general approach to
critical patients, use of investigations and resuscitation skills) while
all the teamwork-related learning outcomes are grouped under one category.
The written learning outcomes were first coded under these intended
learning outcomes. Items not fitted under the intended learning outcomes
were considered new findings. These new findings were further processed
newly identified themes. The results of thematic analysis were checked
serially by the authors for quality assurance. Consensus on new themes
after further literature review was made between authors on items that
could not be categorised under the intended learning outcomes.
Results
Data saturation was attained after 20 sessions with
149 evaluation forms collected (data saturation is a point when no new
theme was found by thematic analysis after analysing the responses after
several courses). The response rate was 100% and more than 99% (148 out of
149) of the returned forms were complete, despite the voluntary nature of
data collection.
The intended learning outcomes are listed in Table
1. From the contents of the evaluation form, all of the intended
learning outcomes were well received by the respondents, as reflected by
the responses shown in Table 1.
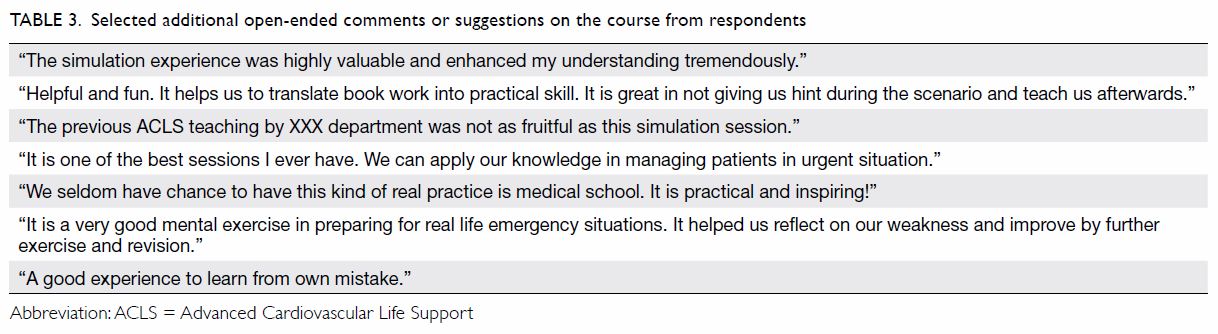
In addition to the intended learning outcomes, we
discovered a large number of learning points or reflections that cannot be
categorised under our pre-planned learning objectives. These additional
unexpected learning points were processed by thematic analysis under new
headings as listed in Table 2.
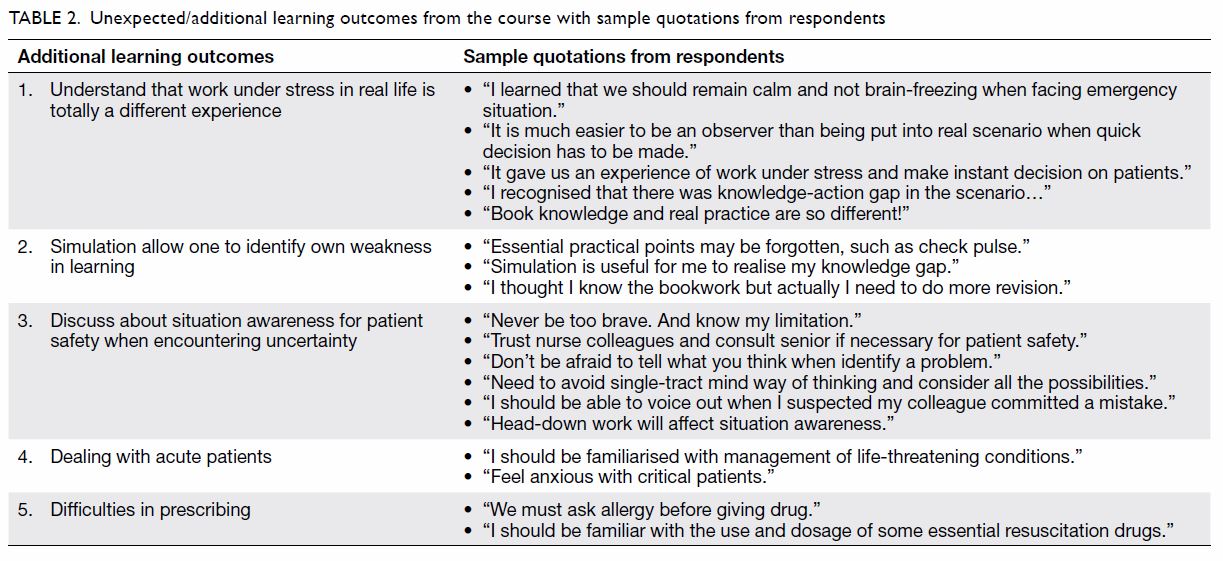
Table 2. Unexpected/additional learning outcomes from the course with sample quotations from respondents
Respondents were also given the opportunity to make
open comments or suggestions about the course. Some of the responses are
listed in Table 3.
Discussion
The original intention of course evaluation
questionnaire was to evaluate the learning objectives as perceived by
students. The results suggest that our intended learning outcomes were
well received by our students. A number of learning outcomes were revealed
that did not fall into our intended learning outcomes by thematic
analysis. Additional literature review revealed that these unexpected
outcomes match some gaps identified in the transition between
undergraduate medical education and postgraduate practice.
Fidelity
In our training course, high fidelity was thought
to be an important element to achieve the learning outcomes, including the
unexpected ones. Fidelity is commonly defined as “the level of realism
present to the learners during a simulation training”.3 4
Conventionally, it is believed that higher fidelity leads to more
efficient learning.6
However, fidelity is not a single-dimensional
concept and there are different components of fidelity described in the
literature using different terminology. For simplicity, we consider the
definition of fidelity described by Feinstein and Cannon, in which
fidelity of simulation has physical and functional aspects.3 Physical fidelity includes the environmental, visual,
and spatial components, such as the design of the simulation room, the
performance of manikin, and the settings of various instruments.
Functional fidelity is a dynamic interaction between the participants and
their task, including information, stimuli, and responses of learners.
Other simulation educators have used the terms “conceptual”,
“experiential”, “emotional” or more commonly “psychological” fidelity to
describe the same or similar concepts,2
7 but further discussion is beyond
the scope of the present study.
High-fidelity simulation training was not always
regarded as superior to lower-fidelity training. Besides the issue of
cost, early studies in the last century in various disciplines (such as
civil and military aviation) failed to show better learning outcomes after
high physical fidelity training.3 8 9
10 This might be because the high
physical fidelity training over-stimulated novice learners and resulted in
cognitive overload that jeopardised the intended learning objectives.11 Such findings supported the conventional belief that
low fidelity is better for beginners and high fidelity is for expert
learners. Medical students are regarded as novice learners and have little
or no working experience. These conventional beliefs lead to the
conclusion that it is unreasonable and not cost-effective to expose
medical students to high physical fidelity simulation training. However,
this overlooks the importance of functional or psychological fidelity. In
recent years, studies have suggested that functional or psychological
fidelity is important in enhancing learning.7
12 13
14 15
In addition to simulating real-world functioning, high psychological
fidelity also creates a stressful environment, increasing student arousal
level and facilitating learning and performance. Therefore, in our
training course, in addition to the relatively high physical fidelity
provided by the well-equipped simulation training room and sophisticated
manikin, we further enhanced functional or psychological fidelity by the
following interventions:
All of these measures enhanced functional fidelity
by providing a realistic working environment and imposed psychological
immersion for the participants.
A further remark on the term “fidelity” is that
physical and psychological fidelity are not mutually exclusive nor
competitive, but are actually complementary to each other.17 18 19 20 For
example, a high-fidelity manikin who can talk or moan can enhance
psychological stimuli for the participants.
Some of the learning outcomes of the course are
closely related to psychological fidelity, namely teamwork, working under
stress, identifying one’s own weakness, acute patient management, and
situation awareness. In the written responses under these headings, we
could see interaction, flow of information, stress, and self-reflection.
Gaps in undergraduate medical education
Although not the original objective of this study,
we found that the unexpected learning outcomes of this study echoed some
of the identified gaps between transitions from undergraduate medical
education to early postgraduate medical practice in the literature. In the
medical education literature there have been calls worldwide for reform of
undergraduate medical curricula, to address gaps identified in
undergraduate medical education that adversely affect medical interns in
their early practice.21 22 23 24 25 These
gaps include working under stress, working on call, uncertainties,
helplessness, workload, difficulties prescribing medication, and managing
acutely ill patients, and similar gaps have been identified in medical
educations programmes across the world.
Newly graduated interns perceive their work to be
stressful and have feelings of being underprepared.23 24 25 Educators have suggested that undergraduate curricula
should prepare medical students to deal with expected stress, such as
facing uncertainty, knowing one’s limitations, and asserting one’s right
for support.21 26 27 These
wordings or identified gaps were found in the perceived learning outcomes
of our course. In the literature, interns have indicated that they could
not predict their shortcomings in their undergraduate study until they
were in clinical practice. Furthermore, it was also suggested that
undergraduate medical education should include more on communication
skills and emotional involvement.21
28 29
Again these aspects match the perceived learning outcomes of our course.
More work-related training should be put in the
final year of medical school, particularly for dealing with acutely ill
patients and prescribing medication.30
31 32
Studies have shown that despite curriculum reform, management of acute
problems has remained an unclosed gap.30
33 34
Work-related training with acutely ill patients is difficult to achieve
because such patients are not always readily available even if medical
students do a period of assistant internship. This is a likely reason that
curriculum reform and workplace placements during their final year closed
some gaps but not others.20 21 The opportunities for students to experience real
acute care are limited, making it difficult to build expertise through
repetitive practice.35 36 Furthermore, there is always an ethical consideration
of whether to allow students to treat acutely ill patients.37
The learning outcomes of our study suggest that
high-fidelity simulation training can be a solution to the gaps
identified. High-fidelity simulation training can create a lot of
scenarios with acutely ill patients in a short period of time, to create
an environment in which students can make mistakes and learn from these
mistakes without harming real patients. This idea is supported by the
literature, which demonstrates simulation training is better than other
forms of instruction method such as didactic or problem-based learning and
should serve as an adjunct to other instruction methods.2 38 39 This point is particularly important because interns
or junior doctors are the first medical responders called to attend
acutely deteriorating patient in a ward and their suboptimal management
might put patients at risk or delay appropriate treatment.21 29 The
General Medical Council of the United Kingdom also recommends the use of
simulation technology in medical school.22
The limitations of this study include that data
were collected from only one medical school, the current curriculum was
not discussed, the cohort included students at different times in their
final year, and most (but not all) students were recruited before formal
clinical placement.
Summary
There are gaps between undergraduate medical
education and transition to postgraduate clinical practice which could be
eliminated through reform of undergraduate medical school curricula. The
application of psychologically immersive high-fidelity simulation training
for medical students is likely to be a helpful strategy to enhance their
preparedness. Such training should emphasise management of acutely ill
patients.
Author contributions
All authors had full access to the data,
contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity. YF Choi wrote the
article. All authors contributed to the concept of study, acquisition and
analysis of data, and critical revision for important intellectual
content.
Conflicts of interest
As an editor of the journal, TW Wong was not
involved in the peer review process. The other author has disclosed no
conflicts of interest.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
No real patients were involved in this study and no
personal data was collected from the participants. Verbal consent was
obtained from all participants in the introduction session of the course;
participation was non-compulsory. The study was approved by the hospital
ethics committee (Ref HKECREC-2019-013).
References
1. Alessi SM. Fidelity in the design of
instructional simulations. J Comput Based Instr 1988;14:40-7.
2. Maran NJ, Glavin RJ. Low- to high-
fidelity simulation—a continuum of medical education? Med Educ
2003;37(Suppl 1):22-8. Crossref
3. Feinstein AH, Cannon HM. Fidelity,
verifiability, and validity of simulation: constructs for evaluation.
Developments in Business Simulation and Experiential Learning. 2001; 28:
57-65.
4. Mills BW, Carter OB, Rudd CJ, Claxton
LA, Ross NP, Strobel NA. Effects of low- versus high-fidelity simulations
on the cognitive burden and performance of entry-level paramedicine
students: a mixed-methods comparison trial using eye-tracking, continuous
heart rate, difficulty rating scales, video observation and interviews.
Simul Healthc 2016;11:10-8. Crossref
5. Choi YF, Wong TW. High fidelity
simulation training for medical students in emergency medicine specialty
clerkship. Proceedings of the 9th Asia Medical Education Symposium cum
Frontiers in Medical and Healthcare Science Education 2017. OP2.
6. Hays RT, Singer MJ. Simulation Fidelity
in Training System Design: Bridging the Gap between Reality and Training.
New York: Springer-Verlag; 1989. Crossref
7. Diederich E, Mahnken JD, Rigler SK,
Williamson TL, Tarver S, Sharpe MR. The effect of model fidelity on
learning outcomes of a simulation-based education program for central
venous catheter insertion. Simul Healthc 2015;10:360-7. Crossref
8. Matsumoto ED, Hamstra SJ, Radomski SC,
Cusimano MD. The effect of bench model fidelity on endourological skill: a
randomized controlled trial. J Urol 2002;167:1243-7. Crossref
9. Chandra DB, Savoldelli GL, Joo HS, Weiss
ID, Nail VN. Fiberoptic oral intubation: the effect of model fidelity on
training for transfer to patient care. Anesthesiology 2008;109:1007-13. Crossref
10. Grober ED, Hamstra SJ, Wanzel KR, et
al. The educational impact of bench model fidelity on the acquisition of
technical skill: the use of clinically relevant outcome measures. Ann Surg
2004;240:374-81. Crossref
11. Martin EL, Waag WL. Contributions of
platform motion to simulator training effectiveness: Study I—basic
contact. 39. Brooks Air Force Base, Texas Air Force Human Resources
Laboratory; 1978. Crossref
12. Bland AJ, Topping A, Tobbell J. Time
to unravel the conceptual confusion of authenticity and fidelity and their
contribution to learning within simulation-based nursing education. A
discussion paper. Nurse Educ Today 2014;24:1112-8. Crossref
13. Chetwood JD, Grag P, Burton K.
High-fidelity realistic acute medical simulation and SBAR training at a
tertiary hospital in Blantyre, Malawi. Simul Healthc 2018;13:139-45. Crossref
14. Rudolph JW, Simon R, Reamer DB. Which
reality matters? Questions on the path to high engagement in healthcare
simulation. Simul Healthc 2007;2:161-3. Crossref
15. Hamstra SJ, Brydges R, Hatala R,
Zendejas B, Cook DA. Reconsidering fidelity in simulation-based training.
Acad Med 2014;89:387-92. Crossref
16. Rudolph JW, Raemer DB, Simon R.
Establishing a safe container for learning in simulation: the role of the
presimulation briefing. Simul Healthc 2014;9:339-49. Crossref
17. Kozlowski SW, DeShon RP. A
psychological fidelity approach to simulation-based training: theory,
research and principles. In: Elliott LR, Coovert MD, Schiflett SG,
editors. Scaled Worlds: Development, Validation and Applications. New
York: Ashgate Publishing; 2017.
18. Oser RL, Cannon-Bowers J, Sala E,
Dwyer DJ. Enhancing human performance in technology-rich environments:
Guidelines for scenario-based training. Hum Tach Interact Complex Sys
1999;9:175-202.
19. Beaubien JM, Baker DP. The use of
simulation for training teamwork skill in health care: how low can we go?
Qual Saf Health Care 2004;13 Suppl 1:i51-6. Crossref
20. Tun JK, Alinier G, Tang J, Kneebone
RL. Redefining simulation fidelity in healthcare education. Simul Gaming
2015;46:159-74. Crossref
21. Bernnan N, Corrigan O, Allard J, et
al. The transition from medical student to junior doctor: today’s
experiences of tomorrow’s doctors. Med Educ 2010;44:449-58. Crossref
22. General Medical Council. Tomorrow’s
Doctors. London: GMC; 2009.
23. Teo A. The current state of medical
education in Japan: a system under reform. Med Educ 2007;41:302-8. Crossref
24. Segouin C, Jouquan J, Hodges B, et al.
Country report: medical education in France. Med Educ 2007;41:295-301. Crossref
25. Ochsmann EB, Zier U, Drexler H, Schmid
K. Well prepared for work? Junior doctors’ self-assessment after medical
education. BMC Med Educ 2011;11:99. Crossref
26. Miles S, Kellett J, Leinster SJ.
Medical graduates’ preparedness to practice: a comparison of undergraduate
medical school training. BMC Med Educ 2017;17:33. Crossref
27. Lempp H, Cochrane M, Seabrook M, Rees
J. Impact of educational preparation on medical students in transition
from final year to PRHO year: a qualitative evaluation of final-year
training following the introduction of new year 5 curriculum in a London
medical school. Med Teach 2004;26:276-8. Crossref
28. Watmough S, Garden A, Taylor D.
Pre-registration house officers’ views on studying under a reformed
medical curriculum in the UK. Med Educ 2006;40:893-9. Crossref
29. O’Neill PA, Jones A, Willis SC,
McArdle PJ. Does a new undergraduate curriculum based on Tomorrow’s
Doctors prepare house officers better for their first post? A qualitative
study of the views of pre-registration house officers using critical
incidents. Med Educ 2003;37:1100-8. Crossref
30. Illing JC, Peile E, Morrison J, et al.
How prepared are medical graduate to begin practice? A comparison of three
diverse UK medical school. London: General Medical Council; 2008.
31. Smith CM, Perkins GD, Bullock I, Bion
JF. Undergraduate training in the care of the acutely ill patient: a
literature review. Intensive Care Med 2007;33:901-7. Crossref
32. Jensen ML, Hesselfeldt R, Rasmussen
MB, et al. Newly graduated doctors’ competence in managing cardiopulmonary
arrests assessed using a standardized Advanced Life Support (ALS)
assessment. Resuscitation 2008;77:63-8. Crossref
33. Bosch J, Maaz A, Hitzblech T,
Holzhausen Y, Peters H. Medical students’ preparedness for professional
activities in early clerkship. BMC Med Educ 2017;17:140. Crossref
34. Illing JC, Morrow GM, Rothwell nee
Kergon CR, et al. Perception of UK medical graduates’ preparedness for
practice: a multi-centre qualitative study reflecting the importance of
learning on the job. BMC Med Educ 2013;13:34. Crossref
35. Phillips PS, Nolan JP. Training in
basic and advanced life support in UK medical schools: questionnaire
survey. BMJ 2001;323:22-3. Crossref
36. Vozenilek J, Huff JS, Reznek M, Gordon
JA. See one, do one, teach one: advanced technology in medical education.
Acad Emerg Med 2004;11:1149-54. Crossref
37. Ziv A, Wolpe PR, Small SD, Glick S.
Simulation-based medical education: an ethical imperative. Acad Med
2003;78:783-8. Crossref
38. Beal MD, Kinnear J, Anderson CR,
Martin TD, Wamboldt R, Hooper L. The effectiveness of medical simulation
in teaching medical students critical care medicine: A systemic review and
meta-analysis. Simul Healthc 2017;12:104-16. Crossref
39. McCoy CE, Menchine M, Anderson C,
Kollen R, Langdorf MI, Lotfipour S. Prospective randomized crossover study
of simulation vs didactics for teaching medical students the assessment
and management of critically ill patients. J Emerg Med 2011;40:448-55. Crossref