Hong
Kong Med J 2019 Oct;25(5):356–62 | Epub 9 Oct 2019
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Prehospital electrocardiogram shortens ischaemic time
in patients with ST-segment elevation myocardial infarction
KS Cheung, FHKCEM1; LP Leung, FHKCEM2; YC
Siu, FHKCEM3; TC Tsang, FHKCEM1; Matthew SH Tsui, FRCP (Edin), FHKAM (Emergency Medicine)1; CC Tam, FHKCP, FHKAM (Medicine)4;
Raymond HW Chan, FHKAM (Medicine)5
1 Department of Accident and Emergency,
Queen Mary Hospital, Pokfulam, Hong Kong
2 Emergency Medicine Unit, Li Ka Shing
Faculty of Medicine, The University of Hong Kong, Pokfulam, Hong Kong
3 Fire and Ambulance Services Academy,
Hong Kong Fire Services Department, Tseung Kwan O, Hong Kong
4 Department of Medicine, Queen Mary
Hospital, Pokfulam, Hong Kong
5 Division of Cardiology, Hong Kong
Sanatorium & Hospital, Happy Valley, Hong Kong
Corresponding author: Dr KS Cheung (
cks373@ha.org.hk)
Abstract
Introduction: Total
ischaemic time should be shortened as much as possible in patients with
ST-segment elevation myocardial infarction (STEMI). This study evaluated
whether prehospital 12-lead electrocardiogram (ECG) could shorten system
delay in STEMI management.
Methods: From November 2015 to
November 2017, 15 ambulances equipped with X Series Monitor/
Defibrillator (Zoll Medical Corporation) were used in the catchment area
of Queen Mary Hospital, Hong Kong. Prehospital ECG was performed for
patients with chest pain; the data were tele-transmitted to attending
emergency physicians at the Accident and Emergency Department (AED) for
rapid assessment. Data from patients with STEMI who were transported by
these 15 ambulances were compared with data from patients with STEMI who
were transported by ambulances without prehospital ECG or who used
self-arranged transport.
Results: Data were analysed from
197 patients with STEMI. The median patient delay for activation of the
emergency response system was 90 minutes; 12% of patients experienced a
delay of >12 hours. There was a significant difference in delay
between patients transported by ambulance and those who used
self-arranged transport (P<0.001). For system delay, the use of
prehospital ECG shortened the median time from ambulance on scene to
first ECG (P<0.001). When performed upon ambulance on scene,
prehospital ECG was available 5 minutes earlier than if performed in
ambulance compartment before departure. Use of prehospital ECG
significantly shortened AED door-to-triage time, AED door-to-first AED
ECG time, AED door-to-physician consultation time, and length of stay in
the AED (P<0.001 for all comparisons).
Conclusion: Prehospital ECG
shortened ischaemic time prior to hospital admission.
New knowledge added by this study
- Patient delay is significantly longer for patients who use self-arranged transport compared with those transported by ambulance.
- System delay—in particular the time from ambulance on scene to first electrocardiogram (ECG)—is significantly shorter with prehospital ECG than without.
- To minimise ischaemic time, ECG should be performed on scene, rather than in the ambulance compartment whenever feasible.
- This evidence supports a recommendation for the Hong Kong Fire Services Department to purchase prehospital ECG machines for the whole territory in the future.
Introduction
Approximately 10.6 persons in Hong Kong die of
coronary heart diseases each day.1
Coronary heart diseases represent a spectrum of disorders, from common
atherosclerosis to life-threatening ST-segment elevation myocardial
infarction (STEMI). The European Society of Cardiology has divided the
total ischaemic time in patients with STEMI into patient and system
delays.2 System delays are further
subdivided into emergency medical system and non-emergency medical system
(hospital) delays. Minimising delays of all types would be most beneficial
for patient outcome. To the best of our knowledge, there have been no
studies of the components of ischaemic time in patients with STEMI in Hong
Kong.
The Hong Kong Fire Services Department (HKFSD)
serves as the primary emergency ambulance provider in Hong Kong. Ambulance
services are activated by the Fire Service Control Centre upon calls to
999; the ambulances are staffed in accordance with protocols approved by
the HKFSD Medical Director.3
Patients are transported to the nearest public hospital, based on their
geographical location. There is no opportunity for patients to choose the
destination hospital, and no primary diversions are used for chest
pain/STEMI.
To shorten the total ischaemic time in patients
with STEMI, the HKFSD and the Department of Accident and Emergency (AED)
of Queen Mary Hospital (QMH) jointly launched a pilot project named
‘Prehospital Ambulance 12-lead Electrocardiogram for Chest Pain Patients
in Hong Kong West Cluster’. Our group previously published an article
using data from the first phase of this pilot project (12 November 2015 to
31 December 2016), demonstrating the impact of prehospital 12-lead
electrocardiogram (ECG) on door-to-balloon time (D2B) in patients with
STEMI who received primary percutaneous coronary intervention (PPCI).3 However, the majority of D2B time constituted the
post-admission period, whereas myocardial injury likely began with the
onset of symptoms before hospital admission. We hypothesised that
prehospital ECG would also shorten the ischaemic time before hospital
admission, including the first medical contact-to-first ECG time, AED
door-to-triage and AED door-to-consultation time, and length of stay in
the AED. In the present analysis, pre-admission data from our pilot
project were compared with those of patients with STEMI who received the
standard management. By assessing the patient flow from the onset of
symptoms until admission, patient and system delays could be identified,
and potential improvements could be implemented accordingly.
Methods
This was a retrospective observational study of
data from the first and second phases of the ‘Prehospital Ambulance
12-lead Electrocardiogram for Chest Pain Patients in Hong Kong West
Cluster’ pilot project (12 November 2015 to 5 November 2017). Data were
provided by the QMH AED, QMH Cardiac Care Unit (CCU), and HKFSD.
The QMH CCU provided the list of all patients
admitted through the AED with emergency coronary angiography, with or
without PPCI. This included patients who travelled to hospital by
self-arranged transport, as well as those who travelled by ambulance with
and without prehospital 12-lead ECG. Patients were excluded if they had
STEMI that developed during in-patient stay, if they had post-arrest
malignant arrhythmia, or if they had
extracorporeal-membrane-oxygenation-assisted cardiopulmonary resuscitation
(ECMO-CPR). Patients secondarily transported from St John Hospital on an
outlying island were also excluded. The HKFSD and QMH AED provided data
regarding the first and second phases of our pilot project, in which 15
HKFSD ambulances in Hong Kong West Cluster were equipped with X Series
Defibrillator/Monitor (Zoll Medical Corporation, Chelmsford [MA], US).
Prehospital 12-lead ECGs of chest pain patients were tele-transmitted to
the AED for immediate assessment by an emergency physician. Physicians
from CCU received alerts regarding patients with suspected STEMI in ECG.
This pilot project began on 12 November 2015; the first phase ended on 31
December 2016. In the first phase, all prehospital ECGs were obtained in
ambulance compartments before departure from the scene. In the second
phase (1 January 2017 to 5 November 2017), prehospital ECGs were performed
either upon ambulance on scene or in the ambulance compartment, as
determined by the ambulance crew based on the feasibility of carrying the
X Series Defibrillation/Monitor to the scene.
The primary objective of this study was to
investigate whether there were significant differences in patient and
system delays between the use of prehospital 12-lead ECG and standard
care. The primary outcomes were the patient and system delay times in
minutes. Patient delay was measured from the time of symptom onset to the
time of emergency response system activation. The times of emergency
response system activation were the time of the 999 call for ambulance
patients and the time of AED registration for patients with self-arranged
transport. System delay was measured from the time of emergency response
system activation to the time of admission through the AED. System delay
was further stratified as the time from ambulance on scene to AED
registration; ambulance on scene to first ECG (for patients travelling by
ambulance); AED door-to-triage time, AED door-to-first AED ECG time, AED
door-to-physician consultation time, and length of stay in the AED (for
all patients). The secondary objective of this study was to assess
accuracy of triage, benefit of performing prehospital ECG when ambulance
on scene compared with in the ambulance compartment, ability to call CCU
on/before patient arrival, and adherence to HKFSD performance pledge.
Triage accuracy was measured by proportion of patients correctly triaged
as category 1. Benefit of performing prehospital ECG when ambulance on
scene compared with in the ambulance compartment was measured by shortened
time in minutes to undergo ECG when the former is performed. Ability to
call CCU on/before patient arrival was measured by the proportion of
patients with CCU calls on/before AED registration. Adherence to HKFSD
performance pledge was measured as the time from 999 call to the time of
ambulance arrival at the street address.
Data were analysed by Excel 2010 (Microsoft Corp,
Redmond [WA], US) and SPSS (Windows version 25.0; IBM Corp, Armonk [NY],
US). The non-parametric Mann-Whitney U test was used to analyse
statistical differences between groups.
Results
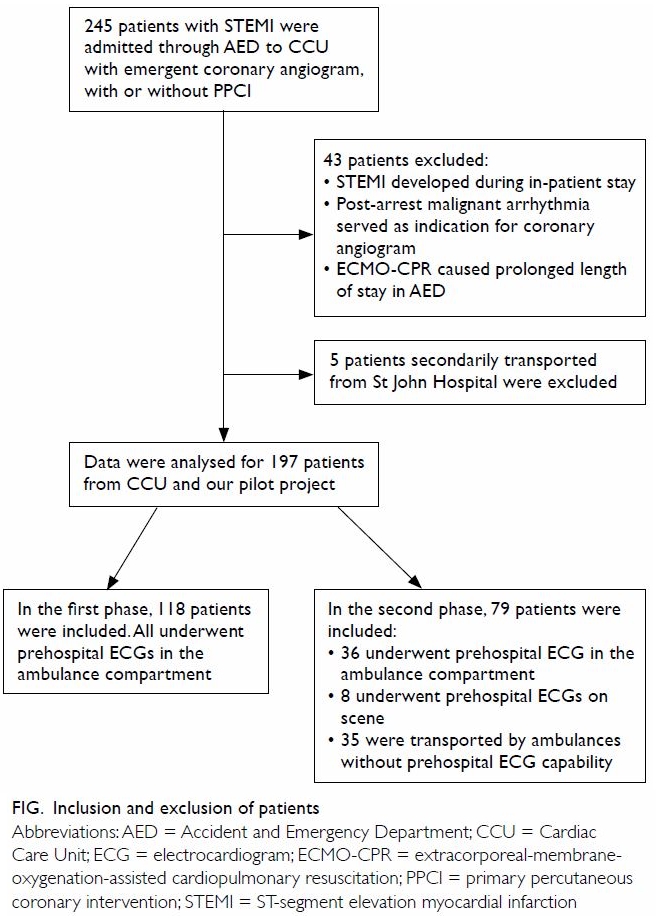
In all, 245 patients were admitted through the AED
to the CCU with emergent coronary angiogram, with or without PPCI. In
total, 43 patients were excluded because they developed STEMI during
in-patient stay, exhibited post-arrest malignant arrhythmia, or required
ECMO-CPR. In addition, five patients who were secondarily transported from
St John Hospital were excluded. Data were analysed for a total of 197
patients from CCU and our pilot project. In the first phase, 118 patients
were included; all underwent prehospital ECGs in the ambulance
compartment. In the second phase, 79 patients were included; 36 and eight
underwent prehospital ECGs in the ambulance compartment and on scene,
respectively. The remaining 35 patients were transported by ambulances
without prehospital ECG capabilities (Fig).
Patient delay
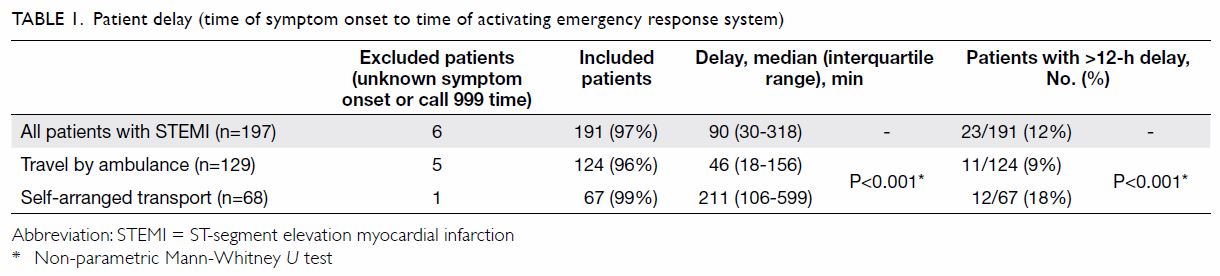
The median patient delay time was 90 minutes; 12%
of patients experienced delays of >12 hours. There was significant
difference in patient delay between patients travelling by ambulance and
those who used self-arranged transport (Table 1).
System delay
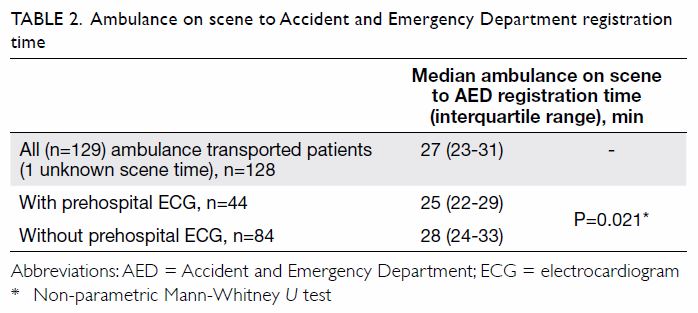
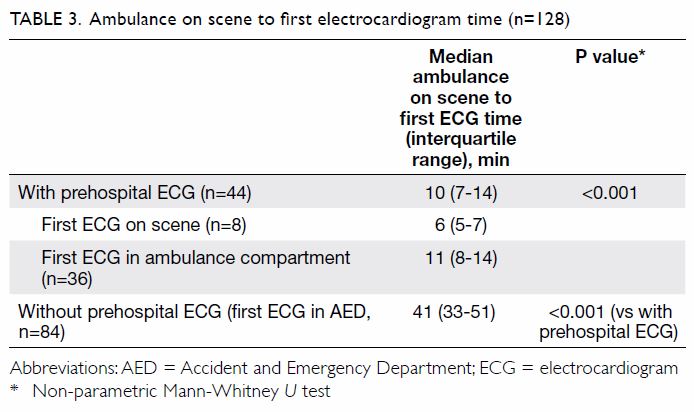
There were significant differences between patients
with and without prehospital ECG, in terms of median time from ambulance
on scene to AED registration (Table 2), and ambulance on scene to first ECG (Table
3). Prehospital ECG was available 5 minutes earlier if performed
upon ambulance on scene compared with that in ambulance compartment. This
5-minute difference also gave us an estimate of time required to transfer
the patient to the ambulance from the scene where the patient experienced
chest pain. Prehospital ECG performed at the time of ambulance on scene
was available 35 minutes earlier than the first ECG (in the AED) for
patients who used self-arranged transport.
After excluding six patients with unknown time of
999 call or unknown time of ambulance arrival on scene, the median time
from 999 call to ambulance on scene was 8 minutes (interquartile range,
6-10 minutes). Overall, 119 of 123 (96.7%) patients had times within 17
minutes (12 minutes to street address performance pledge by HKFSD, plus 5
minutes travel time between ambulance and scene). Forty-three patients
with STEMI underwent prehospital ECG and had known CCU call times; of
these, ambulance crews in 7 of 8 with ECG performed on scene (88%), and 25
of 35 with ECG performed in the ambulance compartment (71%), were able to
contact the CCU physician on or before patient arrival in AED. With
prehospital ECG, AED door-to-triage time, AED door-to-first AED ECG time,
AED door-to-physician consultation time, and length of stay in the AED
were all significantly shortened. In addition, more patients with STEMI
were correctly triaged as category 1 if they had undergone prehospital ECG
(Table 4).
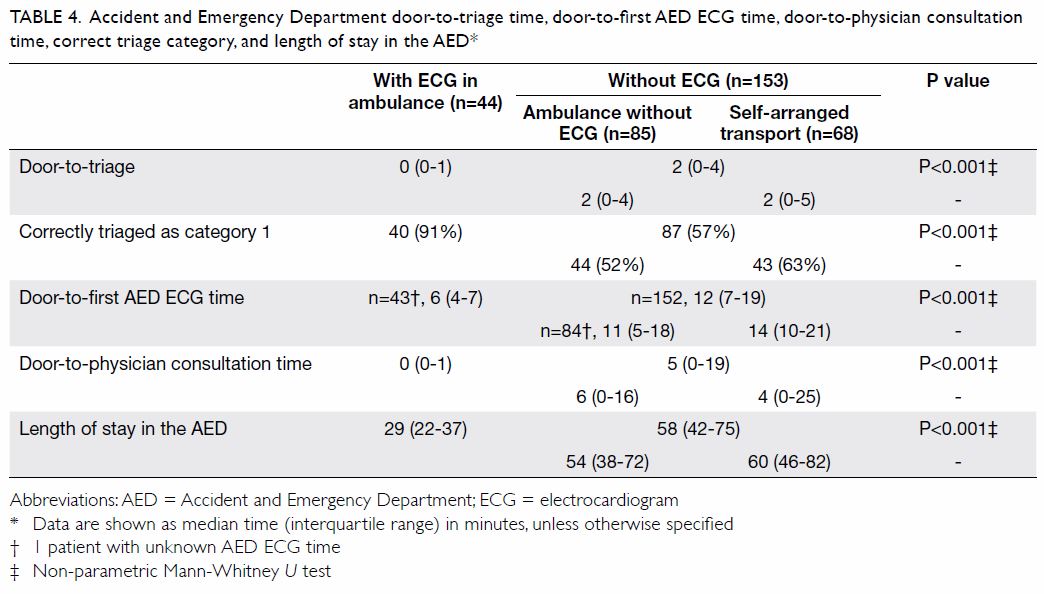
Table 4. Accident and Emergency Department door-to-triage time, door-to-first AED ECG time, door-to-physician consultation time, correct triage category, and length of stay in the AED
Discussion
Patient delay
The MEDEA study showed that female sex and age
>65 years were factors associated with delayed presentation in patients
with acute myocardial infarction.4
Perceived barriers in care-seeking and symptom congruence were also
associated with prehospital delays in Hong Kong Chinese patients with
acute myocardial infarction.5
Although current guidelines recommend PPCI by an experienced team within
12 hours of symptom onset as a reperfusion strategy in patients with
STEMI,2 12% of patients in our
study called 999 or arrived at the AED >12 hours after symptom onset (Table 1). These delays might have worsened their
outcomes. Moreover, 15 of 197 (7.6%) were evaluated by another physician
before they presented to the AED, and those other physicians might have
performed ECG in their clinics. Regardless of the availability of ECG in
the other clinics, there is no formal communication channel between the
AED and private physicians, with the exception of referral letters. These
factors may also have contributed to delays.
A key factor for reducing prehospital delay is
education of the public, especially high-risk patients, regarding the
prudent use of emergency medical services and the typical symptoms of
myocardial infarction. Online symptom checkers have been devised for
patient self-diagnosis. However, an audit study found only moderate
accuracy in these algorithms.6
Because patients with STEMI often have other medical co-morbidities that
require regular follow-up by family physicians or general out-patient
clinics, education regarding typical symptoms of myocardial infarction and
the availability of prehospital ECG assessments could be provided during
these regular consultations. Notably, prehospital ECG can be performed
only after a patient has activated the emergency response system;
therefore, it cannot shorten the patient delay unless it is coupled with
public education regarding STEMI symptoms and public awareness of
prehospital ECG availability.
Self-arranged travel versus ambulance transport
Approximately one-third of patients with STEMI in
our pilot project used self-arranged transport for travelling to the
hospital. This phenomenon is not unique to Hong Kong.7 8 9 Compared with patients travelling by ambulance, a
greater proportion of patients travelling by self-arranged transport had
patient delay time of >12 hours (Table 1). Self-arranged transport patients did not
undergo prehospital ECG. The delayed activation of the emergency response
system deprived such patients of early assessment by an ambulance crew, as
well as early notifications to the AED and CCU physicians of unstable
vitals and a potential need for life-saving treatment. It is important to
educate the public on appropriate use of ambulance services. Mass media
campaigns regarding use of ambulances for chest pain have been shown to
increase emergency medical system use by people with chest pain and
suspected acute coronary syndromes.10
In this study, there was a significant difference in the median times for
ambulance patients to make 999 calls and for self-arranged transport
patients to register in the AED (Table 1). This may be related to differences in
awareness of STEMI symptoms, different patient attitudes regarding
management of their own symptoms, and different treatment expectations
regarding ambulance services. Education should emphasise early 999 calls
for patients with STEMI symptoms, instead of the use of self-arranged
transport.
The Hong Kong Fire Services Department performance
pledge
For emergency ambulance calls, the HKFSD has a
performance pledge of within 12 minutes for 92.5% of patients, from the
time of the call to the arrival of an ambulance at the designated street
address.11 For chest pain patients with suspected myocardial infarction,
even when 5 additional minutes are added to include travel time from the
ambulance to the scene (as estimated in Table 3), this pledge remains more stringent than
those of ambulance services in other countries. For example, the average
response time by the London Ambulance Service for corresponding category 2
calls is 18 minutes.12 In our 123
patients with STEMI who were transported by ambulances, the median
response time was 8 minutes; 96.7% of patients received a response within
the target of within 17 minutes during the pilot project. By enhancing the
mobilising system and commissioning new fire stations/ambulance depots at
various locations, the response time for chest pain patients is expected
to decrease further.
Prehospital electrocardiogram and the potential for
delayed transport to the hospital
Before this pilot project was implemented, there
were concerns regarding delayed transport to the hospital due to the
performance of prehospital ECG. In contrast to our expectations, the
median scene-to-AED registration time was 3 minutes shorter in patients
who underwent prehospital ECG, compared with patients who did not undergo
prehospital ECG (Table 2). However, every ambulance journey was
unique and involved a different travel distance. Because the actual
distances travelled and the proportions of time used for performing
prehospital ECG in each ambulance journey were not available, a larger
data analysis is needed to clarify these findings.
On scene or in ambulance compartment
Among the 44 patients with STEMI who underwent
prehospital ECG, the CCU physician was called before patient arrival in 7
of 8 (88%) patients for whom ECG was performed on scene and in 25 of 35
(71%) patients for whom ECG was performed in the ambulance compartment.
The CCU call time was unknown for the remaining one patient. Therefore,
performing prehospital ECG on scene allowed earlier CCU consultations. It
has been recommended that 12-lead ECG recording and interpretation should
be performed as soon as possible upon initial medical contact, with a
target maximum delay of 10 minutes.13
This target was achieved in our pilot project in patients for whom
prehospital ECG was performed on scene (median time: 6 minutes) [Table
3]. We were near this target in patients for whom ECG was performed
in the ambulance compartment (median time: 11 minutes). Therefore, ECG
performance on scene, rather than in the ambulance compartment, is
recommended whenever feasible.
More efficient Accident and Emergency Department
management in multiple steps
Preliminary history and vital signs collected
during ambulance transport were immediately given to the triage nurse upon
patient arrival. This shortened the triage time to 0 minutes
(door-to-triage time) in patients for whom prehospital ECG was performed.
Moreover, triage accuracy was improved: more patients with STEMI (40/44)
who underwent prehospital ECGs were correctly triaged as category 1
(critical) and therefore received immediate treatment. Shortened times for
door-to-first AED ECG and door-to-consultation were evident. Patients with
STEMI who were transported by ambulance could provide notification to the
AED before their arrival, thereby enabling pre-arrival preparation of an
acute care room. In addition, an immediate AED physician assessment with
repeat ECG could be performed upon patient arrival. These changes resulted
in an overall reduction in the length of AED stay (nearly by half),
compared with the length of AED stay for patients who did not undergo
prehospital ECG. Shortened length of AED stay is beneficial for
percutaneous coronary intervention centres where patients with STEMI
cannot yet bypass the AED with direct catheterisation laboratory
admission.
Conclusion
Delayed activation of the emergency response system
and choice of transportation contributed to patient delay. Prehospital
12-lead ECG, preferably performed on scene, can shorten system delay and
total ischaemic time in STEMI management.
Author contributions
All authors had full access to the data,
contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Concept or design: All authors.
Acquisition of data: KS Cheung, YC Siu, RHW Chan.
Analysis or interpretation of data: KS Cheung, LP Leung.
Drafting of the article: KS Cheung.
Critical revision for important intellectual content: All authors.
Acquisition of data: KS Cheung, YC Siu, RHW Chan.
Analysis or interpretation of data: KS Cheung, LP Leung.
Drafting of the article: KS Cheung.
Critical revision for important intellectual content: All authors.
Conflicts of interest
All authors have disclosed no conflicts of
interest.
Acknowledgement
We would like to thank the staff of the following
institutions: (1) Hong Kong Fire Services Department, for performing
prehospital electrocardiograms and providing prehospital data; (2)
Division of Cardiology, Department of Medicine, Queen Mary Hospital, for
providing data on door-to-balloon and door-to-catheter time; (3)
Department of Accident and Emergency, Queen Mary Hospital, for collecting
patient clinical data; (4) Mr Fan Min of Emergency Medicine Unit, Li Ka
Shing Faculty of Medicine, The University of Hong Kong, for statistical
analyses; and (5) Zoll Medical Corporation (Chelmsford [MA], US), for
providing the machines, training, and technical support free of charge.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Ethics approval
Analysis of data from this pilot project was
approved by the Institutional Review Board of The University of Hong Kong/
Hospital Authority Hong Kong West Cluster (UW19-184). The requirement for
patient consent was waived.
References
1. HealthyHK, Department of Health, Hong
Kong SAR Government. Coronary heart diseases. Available from:
https://www.healthyhk.gov.hk/phisweb/en/healthy_facts/disease_burden/major_causes_death/coronary_heart_disease/.
Accessed 21 Apr 2019.
2. Ibanez B, James S, Agewall S, et al.
2017 ESC Guidelines for the management of acute myocardial infarction in
patients presenting with ST-segment elevation: The Task Force for the
management of acute myocardial infarction in patients presenting with
ST-segment elevation of the European Society of Cardiology (ESC). Eur
Heart J 2018;39:119-77. Crossref
3. Cheung KS, Leung LP, Siu YC, et al.
Prehospital 12-lead electrocardiogram for patients with chest pain: a
pilot study. Hong Kong Med J 2018;24:484-91. Crossref
4. Ladwig KH, Fang X, Wolf K, et al.
Comparison of delay times between symptom onset of an acute ST-elevation
myocardial infarction and hospital arrival in men and women <65 years
versus ≥65 years of age: findings from the Multicenter Munich Examination
of Delay in Patients Experiencing Acute Myocardial Infarction (MEDEA)
Study. Am J Cardiol 2017;120:2128-34. Crossref
5. Li PW, Yu DS. Predictors of pre-hospital
delay in Hong Kong Chinese patients with acute myocardial infarction. Eur
J Cardiovasc Nurs 2018;17:75-84. Crossref
6. Semigran HL, Linder JA, Gidengil C,
Mehrotra A. Evaluation of symptom checkers for self diagnosis and triage:
audit study. BMJ 2015;351:h3480. Crossref
7. Hong CC, Sultana P, Wong AS, Chan KP,
Pek PP, Ong ME. Prehospital delay in patients presenting with acute
ST-elevation myocardial infarction. Eur J Emerg Med 2011;18:268-71. Crossref
8. Mathews R, Peterson ED, Li S, et al. Use
of emergency medical service transport among patients with ST-segment-
elevation myocardial infarction: findings from the National Cardiovascular
Data Registry Acute Coronary Treatment Intervention Outcomes Network
Registry-Get with the Guidelines. Circulation 2011;124:154-63. Crossref
9. Lavery T, Greenslade JH, Parsonage WA,
et al. Factors influencing choice of pre-hospital transportation of
patients with potential acute coronary syndrome: an observational study.
Emerg Med Australas 2017;29:210-6. Crossref
10. Nehme Z, Cameron PA, Akram M, et al.
Effect of a mass media campaign on ambulance use for chest pain. Med J
Aust 2017;206:30-5. Crossref
11. Fire Services Department, Hong Kong
SAR Government. Performance pledge. Available from:
https://www.hkfsd.gov.hk/eng/aboutus/performance.html. Accessed 21 Apr
2019.
12. NHS London Ambulance Service. New
ambulance response categories. Available from:
https://www.londonambulance.nhs.uk/calling-us/17086-2/. Accessed 21 Apr
2019.
13. Diercks DB, Peacock WF, Hiestand BC,
et al. Frequency and consequences of recording an electrocardiogram >10
minutes after arrival in an emergency room in non-ST-segment elevation
acute coronary syndromes (from the CRUSADE Initiative). Am J Cardiol
2006;97:437-42. Crossref