Hong
Kong Med J 2019 Jun;25(3):222–7 | Epub 10 Jun 2019
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
MEDICAL PRACTICE
Hong Kong needs a territory-wide registry for
out-of-hospital cardiac arrest
CT Lui, FHKCEM, FHKAM (Emergency Medicine)1;
CL Lau, FHKCEM, FHKAM (Emergency Medicine)1; Axel YC Siu,
FHKCEM, FHKAM (Emergency Medicine)2; KL Fan, FHKCEM, FHKAM
(Emergency Medicine)3; LP Leung, FHKCEM, FHKAM (Emergency
Medicine)4
1 Accident and Emergency Department,
Tuen Mun Hospital, Tuen Mun, Hong Kong
2 Accident and Emergency Department,
Ruttonjee Hospital, Wanchai, Hong Kong
3 Accident and Emergency Department, The
University of Hong Kong–Shenzhen Hospital, Shenzhen, China
4 Emergency Medicine Unit, The
University of Hong Kong, Pokfulam, Hong Kong
Corresponding author: Dr CT Lui (luict@ha.org.hk)
Abstract
Out-of-hospital cardiac arrest (OHCA) is an
urgent disease entity, and the outcomes of OHCA are poor. This causes a
significant public health burden, with loss of life and productivity
throughout society. Internationally, successful programmes have adopted
various survival enhancement measures to improve outcomes of
OHCA. A territory-wide organised survival enhancement campaign is
required in Hong Kong to maintain OHCA survival rates that are
comparable to those of other large cities. One key component is to
establish an OHCA registry, such as those in Asia, the United States,
Europe, Australia, and New Zealand. An OHCA registry can provide
benchmarking, auditing, and surveillance for identification of weak
points within the chain of survival and evaluation of the effectiveness
of survival enhancement measures. In Hong Kong, digitisation of records
in prehospital and in-hospital care provides the infrastructure for an
OHCA registry. Resources and governance to maintain a sustainable OHCA
registry are necessary in Hong Kong as the first step to improve
survival and outcomes of OHCA.
Background
Out-of-hospital cardiac arrest (OHCA) and sudden
cardiac death (SCD) are significant healthcare challenges and public
health burdens worldwide.1 It has
been estimated that around half of cardiovascular mortalities present as
SCD.2 Premature death may be caused
by OHCA and SCD, particularly in cases involving children, adolescents,
and young adults. The burden of premature death due to OHCA is on the
magnitude of millions of years of potential life lost, and this is the
third leading cause of years of potential life lost following cancer and
heart disease.1
In Hong Kong, more than 5000 OHCA cases with
attempted resuscitation occur annually.3
The incidence rate of OHCA in 2012 was reported to be 72 per 100 000
population. Although the incidence is low, the prognosis of OHCA is
generally poor. Worldwide, the survival rate of OHCA is 2% to 11%.4 In Hong Kong, a 2017 territory-wide study reported a
survival rate of 2.3% and a neurologically favourable survival rate of
1.5%.3 Reported survival rates of
OHCA in other parts of the world are heterogeneous, with 0.5%-8.5%
reported in Asian countries,5 8.5%
in the US,6 and 10.3% in Europe.7 The survival rate of OHCA in Hong
Kong is low compared with other cities or countries.
Strategies to enhance out-of-hospital cardiac arrest
survival
To maximise the effectiveness of any efforts to
improve OHCA outcomes, a well-organised territory-wide survival
enhancement campaign covering public, prehospital, and in-hospital
resuscitative care for OHCA would be optimal.8
9 In the public dimension,
fostering public awareness, enhancement of rate of good-quality bystander
cardiopulmonary resuscitation (CPR),10
and a territory-wide public access defibrillation programme11 have been the main pillars of enhancement of survival
of OHCA. In Hong Kong, there have been investigations on the availability
and accessibility of defibrillators in the community.12 13 However,
an organised public access programme is still lacking. In terms of
prehospital and in-hospital measures, shorter response times of emergency
medical systems, post-resuscitation targeted temperature management, and
comprehensive post-cardiac arrest care have proven to be effective
measures to improve survival.8 14 A previous systematic review
based mainly on observational data and small-scale trials suggested that
prehospital epinephrine produced no improvement in rate of survival to
hospital discharge.15 A recently
published large-scale trial demonstrated that epinephrine increased the
rate of survival to hospital discharge while increasing the rate of severe
neurological injury in survivors.16
Need for a cardiac arrest registry
Interpretation and comparison of survival rates of
OHCA between cities is complicated by various factors, including variation
in reporting mechanisms, reporting definitions, and prehospital care
models, particularly the practice of prehospital termination of
resuscitation at arrest scenes. The International Liaison Committee on
Resuscitation has defined a standardised style of resuscitation outcome
reports with definitions of parameters.17
The Utstein-style guidelines provide a standardised and harmonised
framework for comparison and benchmarking of emergency medical services
(EMS) systems.17 18 More importantly, epidemiological data on cardiac
arrest provide insight about local systems for management of cardiac
arrest and provide feedback to influence change in systems for enhancing
survival. In 2010, the American Heart Association (AHA) recognised and
reinforced the importance of data collection about OHCA and the
establishment of cardiac arrest registries. The AHA identified and defined
the essential core elements of a high-quality resuscitation system:
measurement, benchmarking, and providing feedback for change. Experts have
recommended that OHCA events become reportable events.19 In the last decade, there have been worldwide efforts
to establish regional cardiac arrest registries in various cities and
countries, including Japan, Singapore, South Korea, Sweden, and the United
Kingdom. There have been collaborative registries in Asia (The Pan-Asian
Resuscitation Outcomes Study), Europe (European Registry of Cardiac
Arrest), the US (Cardiac Arrest Registry to Enhance Survival), and
Australia, and New Zealand (Australian Resuscitation Outcomes Consortium
epidemiological registry). As OHCA is an important public health burden,
there is room for improvement in Hong Kong to enhance the survival rate of
OHCA, and there is scientific support for strategies and measures to
improve the outcomes of OHCA. What is missing in Hong Kong is a
well-organised survival enhancement campaign, together with a
territory-wide cardiac arrest registry. A cardiac arrest registry is a
non-replaceable element of continuous surveillance, identification of weak
points in the chain of survival, and evaluation of the effectiveness of
newly implemented survival enhancement measures.
Value of a cardiac arrest registry
As an indicator of the efficiency of emergency
healthcare systems and for benchmarking
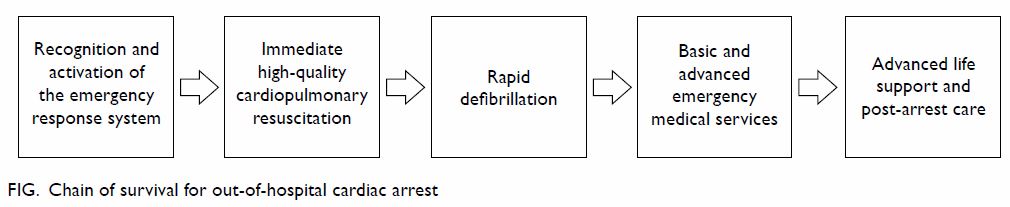
The outcomes and survival rate of OHCA depend on
the chain of survival (Fig). The survival rate and outcomes of OHCA are not
performance indicators of prehospital EMS or emergency departments.
Instead, it is a composite indicator of community resilience and
effectiveness of EMS, advanced life support, and resuscitation in
emergency departments and post-arrest cardiac and intensive care. The
concept of community resilience, which has been supported by many experts
in resuscitation science, had been raised in recent years in management of
conditions where every second counts, such as OHCA.20 Early recognition and appropriate response by
laypersons is the first and most critical step, including EMS activation,
initiation of bystander CPR, and public access defibrillation. If these
initial steps of recognition and resuscitation are not performed well,
profound hypoxic-ischaemic insult to the brain and other major organs is
likely. No matter how hard the subsequent steps in the chain of survival
are, and regardless of the sophistication of advanced and post-arrest
care, the chance of survival and neurological integrity would be limited.
Without a registry, the resilience of Hong Kong and the efficiency of its
emergency healthcare system remain unclear.
Surveillance, audit, and feedback
The OHCA registry is a means of surveillance. The
US Cardiac Arrest Registry to Enhance Survival (CARES) generates reports
with trend analysis regularly. Any major changes in outcomes are
identified, with corresponding investigation and rectification of any
gaps. During audits, weak points of care in the chain of survival can be
identified, which would provide invaluable information for the planning of
a survival enhancement campaign. The AHA has recommended a complete audit
cycle of (1) measurement by a cardiac arrest registry; (2) benchmarking;
and (3) feedback and change. With the OHCA data, one could identify the
weakest link in the chain of survival. Targeted survival enhancement
measures can then be designed and implemented. For example, a local
cardiac arrest registry at the accident and emergency department of Tuen
Mun Hospital identified deficiencies in the availability and accessibility
of publicly accessible defibrillators.12
With the implementation of survival enhancement measures, longitudinal
data collected using the same collection methodology are required to
evaluate their effectiveness.
Evaluation of the effectiveness of survival enhancement
measures
Efficacy is the extent to which a treatment is
capable of bringing about its intended effect under ideal circumstances.
Most clinical trials nowadays have provided information on efficacy.
However, the translation of the effects into clinical practice is not
direct. Effectiveness is the extent to which a treatment achieves its
intended effect in usual clinical settings in daily practice, which is
addressed by studies with pragmatic design. Similar to numerous clinical
conditions, most studies of OHCA evaluate efficacy instead of
effectiveness. Effectiveness cannot be measured in controlled trials. The
observational data in cardiac arrest registries constitute an important
dimension to measure the effectiveness of survival enhancement measures.
In the past decade, there have been numerous improvements in community
engagement and prehospital and in-hospital care for OHCA in Hong Kong.
Community measures include the Heart-safe School Project by the Hong Kong
College of Cardiology,21 mass CPR
training organised by the Resuscitation Council of Hong Kong,22 and the CPR training programme for secondary school
students and domestic helpers by the Emergency Medicine Unit of the
University of Hong Kong. Prehospital improvement measures have included
universal application of external defibrillators, enhanced training of
ambulance crews, widespread prehospital use of laryngeal mask airways,
intravenous adrenaline, first dispatch firefighters, telephone CPR advice,
and enhanced diversion policy for cardiopulmonary arrest. In-hospital
innovations have included implementation of up-to-date advanced life
support care guidelines, use of end-tidal capnography for CPR feedback,
use of mechanical thumpers, extracorporeal CPR, and advancement in
post-arrest intensive and cardiac care. So far, all reports of
resuscitation outcomes of cardiac arrest in Hong Kong have been
cross-sectional. There are no longitudinal data reporting survival trends.
An OHCA registry provides insights into the effectiveness of these
measures in terms of changes in survival. The Japanese Nationwide public
access defibrillation programme, which employs the All-Japan Utstein
Registry of the Fire and Disaster Management Agency, recorded that the
rate of neurologically favourable survival rose from 1.6% to 4.3% in 5
years.11
Experience with cardiac arrest registries in other
cities and countries
The Pan-Asian Resuscitation Outcomes Study
The Pan-Asian Resuscitation Outcomes Study (PAROS)
collaborative network23 was
established in 2010 with a prospective multicentre registry of OHCA events
across the Asia-Pacific region. It was supported by the Singapore Clinical
Research Institute and followed the CARES method. With input from the US
Centers for Disease Control and Prevention (CDC), the PAROS database is
CARES-compatible. The Asian Emergency Medical Services Council adopted the
PAROS registry as one of its core activities. The PAROS network has now
grown into a consortium of nine participating regions and countries:
Australia, Japan, South Korea, Malaysia, Singapore, Taiwan, Thailand,
Turkey, and the United Arab Emirates. The registry includes a population
base of over 89 million. Each participating country is responsible for
administering its own data collection process, and all data are input via
a secure shared internet data capture system with a harmonised database
hosted by the Singapore Clinical Research Institute. The goals of the
network are to provide benchmarking against established registries, to
generate best practice protocols for EMS systems, and to impact community
awareness of emergency resuscitative care.
European Registry of Cardiac Arrest
In 2007, the European Resuscitation Council
initiated a campaign for Europe-wide collaboration on a European registry
to record and analyse cases of cardiac arrest. The European Resuscitation
Council set up a steering committee in 2008 focusing on the development of
the European Registry of Cardiac Arrest (EuReCa), and its objective is to
create a central quality management tool.24
The EuReCa collects data about resuscitative events episodically. The
EuReCa ONE, which included 27 European countries, gathered all
resuscitative events in October 2014.7
For EuReCa TWO, which covers resuscitation events from 1 October 2017 to
31 December 2017, data collection was completed by April 2018 and
publication of results is pending.
Cardiac Arrest Registry to Enhance Survival
The CARES was funded by the US CDC, the Canadian
Ontario Pre-hospital Advanced Life Support network, and the Resuscitation
Outcomes Consortium of North America.25
Its governance is provided by the US CDC and the Emory University School
of Medicine. It provides various platforms for input of standardised
parameters about OHCA events by the participating states. The data sources
include EMS providers, dispatch centres, and hospitals. The data are then
merged into a single event representing a resuscitative episode. The
registry provides a validated measurement tool with benchmarking
capability for continuous quality improvement. It consolidates
observations and conclusions from the collected data and publishes them in
the form of a Morbidity and Mortality Report,6
and the scientific evidence is integrated into the AHA’s resuscitation
guidelines. The CARES was developed as a low-cost, high-impact public
health surveillance system to identify the weakest links in the chain of
survival in participating states.
The Australian Resuscitation Outcome Consortium
Australian and New Zealand out-of-hospital cardiac arrest Epistry
The Australian Resuscitation Outcome Consortium
(Aus-ROC) was established as a National Health and Medical Research
Council Centres of Research Excellence in 2011. Its objective is to
increase research capacity and improve OHCA survival and outcomes. Six
previously established cardiac arrest registries in Australia and two in
New Zealand contributed the data to form the Aus-ROC epidemiological
registry (Epistry) in 2014. The Epistry represents approximately 63% of
the Australian population (23.5 million) and 100% of the New Zealand
population (4.5 million). The Epistry is coordinated and located at the
Aus-ROC administrative base in the School of Public Health and Preventive
Medicine at Monash University in Australia. Participating ambulance
service networks are responsible for the data collection and upload
through a web-based engine. An Epistry Management Committee was
established to serve as the governing agent. Annual benchmarking reports
are generated from the Epistry’s data and provided to the ambulance
services network and relevant bodies for continuous quality improvement.
Technical and operational readiness for a cardiac
arrest registry in Hong Kong
Hong Kong is technically ready for the
establishment of a territory-wide cardiac arrest registry. Clinical
documentation in the prehospital and in-hospital settings would provide
the basic technical infrastructure of the registry. Prehospital care for
patients with cardiac arrest is provided almost exclusively by the
ambulance service of the Fire Services Department, while the Government
Flying Service and St John’s ambulance service play a supplementary role.
The prehospital documentation is digitalised in the electronic Ambulance
Journey Record, where the parameters about cardiac arrest patients are
standardised and Utstein-compatible. Together with electronic hospital
databases and the electronic Accident and Emergency System project of the
Hospital Authority, merging and integration of prehospital and in-hospital
databases would provide a feasible infrastructure and backbone of the
cardiac arrest registry in Hong Kong.
The establishment of cardiac arrest registries may
be quite different from other existing healthcare registries in Hong Kong,
such as the Hong Kong Cancer Registry26
and the Hong Kong Renal Registry.27
The cardiac arrest registries involve various stakeholders including
emergency medical dispatchers, EMS systems, and acute hospitals. The
specialties of acute hospitals include emergency departments, and
intensive care, paediatric, cardiology and medical units. Expert input
from academic units and professional bodies such as the Hong Kong Academy
of Medicine and its Colleges, the Resuscitation Council of Hong Kong, and
universities is desirable.
Governance and a well-defined operational framework
of the OHCA registry are mandatory for sustainability and assurance of
data quality. Referring to the experience with collaborative registries in
the US, Europe, Asia, Australia, and New Zealand, it is reasonable to set
up a registry governing and management committee whose role is to oversee
areas such as setup, maintenance, data quality control, data privacy and
security, and data use and access. The registry committee might be led by
government bodies such as the Food and Health Bureau or co-governed with
academic bodies such as the Hong Kong College of Emergency Medicine or
universities. All relevant stakeholders should be involved in the registry
committee. One key enabler of a sustainable registry is personnel to
maintain it. With the digitisation of documentation in prehospital and
in-hospital records, the gap requiring manual data entry and manipulation
has been dramatically narrowed in recent years.
Setting up an OHCA registry alone does not improve
outcomes of patients with SCD. Survival enhancement campaigns and
strategies, perhaps led by the government, are required. A cardiac arrest
registry should be considered a starting point that provides data to
evaluate the effectiveness of measures adopted in survival enhancement
campaigns and strategies and to provide uniform benchmarking for quality
measurement.
Conclusion
With the growing public health burden of OHCA, Hong
Kong has an imminent need to establish a territory-wide cardiac arrest
registry. It can provide guidance and insight about the effectiveness of
survival enhancement measures. It also provides uniform benchmarking for
continuous quality improvement by both prehospital and in-hospital service
providers. Concerted efforts by various stakeholders from the government,
the Hospital Authority, and academia are necessary to make the registry a
reality.
Author contributions
All authors contributed to the content of the
review article, drafting of the manuscript, and critical revision for
important intellectual content. All authors had full access to the data,
contributed to the study, approved the final version for publication, and
take responsibility for its accuracy and integrity.
Conflicts of interest
All authors declared no conflicts of interest.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
References
1. Stecker EC, Reinier K, Marijon E, et al.
Public health burden of sudden cardiac death in the United States. Circ
Arrhythm Electrophysiol 2014;7:212-7. Crossref
2. Mehra R. Global public health problem of
sudden cardiac death. J Electrocardiol 2007;40(6 Suppl):S118-22. Crossref
3. Fan KL, Leung LP, Siu YC.
Out-of-hospital cardiac arrest in Hong Kong: a territory-wide study. Hong
Kong Med J 2017;23:48-53. Crossref
4. Berdowski J, Berg RA, Tijssen JG, Koster
RW. Global incidences of out-of-hospital cardiac arrest and survival
rates: systematic review of 67 prospective studies. Resuscitation
2010;81:1479-87. Crossref
5. Ong ME, Shin SD, De Souza NN, et al.
Outcomes for out-of-hospital cardiac arrests across 7 countries in Asia:
The Pan Asian Resuscitation Outcomes Study (PAROS). Resuscitation
2015;96:100-8. Crossref
6. McNally B, Robb R, Mehta M, et al.
Out-of-hospital cardiac arrest surveillance—Cardiac Arrest Registry to
Enhance Survival (CARES), United States, October 1, 2005-December 31,
2010. MMWR Surveill Summ 2011;60:1-19.
7. Gräsner JT, Lefering R, Koster RW, et
al. EuReCa ONE-27 Nations, ONE Europe, ONE Registry: a prospective one
month analysis of out-of-hospital cardiac arrest outcomes in 27 countries
in Europe. Resuscitation 2016;105:188-95. Crossref
8. Perkins GD, Lockey AS, de Belder MA, et
al. National initiatives to improve outcomes from out-of-hospital cardiac
arrest in England. Emerg Med J 2016;33:448-51. Crossref
9. Scottish Government. Scottish
out-of-hospital cardiac arrest data linkage project: 2015/16-2016/17
results. Available from:
https://www.gov.scot/publications/scottish-out-hospital-cardiac-arrest-data-linkage-project-2015-16/pages/4/.
Accessed 30 Sep 2018.
10. Wissenberg M, Lippert FK, Folke F, et
al. Association of national initiatives to improve cardiac arrest
management with rates of bystander intervention and patient survival after
out-of-hospital cardiac arrest. JAMA 2013;310:1377-84. Crossref
11. Kitamura T, Iwami T, Kawamura T, et
al. Nationwide public-access defibrillation in Japan. N Engl J Med
2010;362:994-1004. Crossref
12. Ho CL, Lui CT, Tsui KL, Kam CW.
Investigation of availability and accessibility of community automated
external defibrillators in a territory in Hong Kong. Hong Kong Med J
2014;20:371-8. Crossref
13. Fan KL, Lui CT, Leung LP. Public
access defibrillation in Hong Kong in 2017. Hong Kong Med J
2017;23:635-40. Crossref
14. Lai H, Choong CV, Fook-Chong S, et al.
Interventional strategies associated with improvements in survival for
out-of-hospital cardiac arrests in Singapore over 10 years. Resuscitation
2015;89:155-61. Crossref
15. Atiksawedparit P, Rattanasiri S,
McEvoy M, Graham CA, Sittichanbuncha Y, Thakkinstian A. Effects of
prehospital adrenaline administration on out-of-hospital cardiac arrest
outcomes: a systematic review and meta-analysis. Crit Care 2014;18:463. Crossref
16. Perkins GD, Ji C, Deakin CD, et al. A
randomized trial of epinephrine in out-of-hospital cardiac arrest. N Engl
J Med 2018;379:711-21. Crossref
17. Perkins GD, Jacobs IG, Nadkarni VM, et
al. Cardiac arrest and cardiopulmonary resuscitation outcome reports:
update of the Utstein resuscitation registry templates for out-of-hospital
cardiac arrest: a statement for healthcare professionals from a task force
of the International Liaison Committee on Resuscitation (American Heart
Association, European Resuscitation Council, Australian and New Zealand
Council on Resuscitation, Heart and Stroke Foundation of Canada,
InterAmerican Heart Foundation, Resuscitation Council of Southern Africa,
Resuscitation Council of Asia); and the American Heart Association
Emergency Cardiovascular Care Committee and the Council on
Cardiopulmonary, Critical Care, Perioperative and Resuscitation.
Resuscitation 2015;96:328-40. Crossref
18. Jacobs I, Nadkarni V, Bahr J, et al.
Cardiac arrest and cardiopulmonary resuscitation outcome reports: update
and simplification of the Utstein templates for resuscitation registries.
A statement for healthcare professionals from a task force of the
International Liaison Committee on Resuscitation (American Heart
Association, European Resuscitation Council, Australian Resuscitation
Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of
Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern
Africa). Resuscitation 2004;63:233-49. Crossref
19. Nichol G, Rumsfeld J, Eigel B, et al.
Essential features of designating out-of-hospital cardiac arrest as a
reportable event: a scientific statement from the American Heart
Association Emergency Cardiovascular Care Committee; Council on
Cardiopulmonary, Perioperative, and Critical Care; Council on
Cardiovascular Nursing; Council on Clinical Cardiology; and Quality of
Care and Outcomes Research Interdisciplinary Working Group. Circulation
2008;117:2299-308. Crossref
20. Rea TD, Page RL. Community approaches
to improve resuscitation after out-of-hospital sudden cardiac arrest.
Circulation 2010;121:1134-40. Crossref
21. The Hong Kong Jockey Club Charities
Trust. Hong Kong College of Cardiology. The Jockey Club ‘Heart-safe
School’ Project. Available from:
http://www.heartsafeschool.org.hk/aboutus.aspx. Accessed 30 Sep 2018.
22. Resuscitation Council of Hong Kong.
Useful information. The Jockey Club ‘Heart-safe School’ Project. Available
from: http://www.rchk.org.hk/Useful_information.aspx. Accessed 30 Sep 2018.
23. Singapore Clinical Research Institute.
About PAROS. Available from:
https://www.scri.edu.sg/crn/pan-asian-resuscitation-outcomes-study-paros-clinical-research-network-crn/about-paros/.
Accessed 30 Sep 2018.
24. Gräsner JT, Herlitz J, Koster RW,
Rosell-Ortiz F, Stamatakis L, Bossaert L. Quality management in
resuscitation—towards a European Cardiac Arrest Registry (EuReCa).
Resuscitation 2011;82:989-94. Crossref
25. Cardiac Arrest Registry to Enhance
Survival. myCARES. net. Available from: https://mycares.net. Accessed 30
Sep 2018.
26. Xie WC, Chan MH, Mak KC, Chan WT, He
M. Trends in the incidence of 15 common cancers in Hong Kong, 1983-2008.
Asian Pac J Cancer Prev 2012;13:3911-6. Crossref
27. Leung CB, Cheung WL, Li PK. Renal
registry in Hong Kong—the first 20 years. Kidney Int Suppl (2011)
2015;5:33-8. Crossref