Hong
Kong Med J 2018 Dec;24(6):571–8 | Epub 14 Nov 2018
DOI: 10.12809/hkmj177149
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Cross-sectional study on emergency department
management of sepsis
Kevin KC Hung, FHKCEM, MPH1,2; Rex PK
Lam, FHKCEM, MPH3; Ronson SL Lo, MB, BCh, BAO1;
Justin W Tenney, PharmD, BCPS4; Marc LC Yang, FHKCEM1,5;
Marcus CK Tai, FHKCEM1,2; Colin A Graham, FHKCEM, MD1,2
1 Accident and Emergency Medicine
Academic Unit, The Chinese University of Hong Kong, Shatin, Hong Kong
2 Accident and Emergency Department,
Prince of Wales Hospital, Shatin, Hong Kong
3 Emergency Medicine Unit, The
University of Hong Kong, Pokfulam, Hong Kong
4 School of Pharmacy, The Chinese
University of Hong Kong, Shatin, Hong Kong
5 Accident and Emergency Department,
Queen Elizabeth Hospital, Jordan, Hong Kong
Corresponding author: Prof Colin A Graham (cagraham@cuhk.edu.hk)
Abstract
Introduction: Emergency
departments (EDs) play an important role in the early identification and
management of sepsis. Little is known about local EDs’ processes of care
for sepsis, adoption of international recommendations, and the impact of
the new Sepsis-3 definitions.
Methods: Structured telephone
interviews based on the United Kingdom Sepsis Trust ‘Exemplar Standards
for the Emergency Management of Sepsis’ were conducted from January to
August 2017 with nominated representatives of all responding public
hospital EDs in Hong Kong, followed by a review of hospital/departmental
sepsis guidelines by the investigators.
Results: Sixteen of the 18
public EDs in Hong Kong participated in the study. Among various
time-critical medical emergencies such as major trauma, sepsis was
perceived by the interviewees to be the leading cause of in-hospital
mortality and the second most important preventable cause of death.
However, only seven EDs reported having departmental guidelines on
sepsis care, with four adopting the Quick Sequential Organ Failure
Assessment score or its modified versions. All responding EDs reported
that antibiotics were stocked within their departments, and all EDs with
sepsis guidelines mandated early intravenous antibiotic administration
within 1 to 2 hours of detection. Reported major barriers to optimal
sepsis care included lack of knowledge and experience, nursing human
resources shortages, and difficulty identifying patients with sepsis in
the ED setting.
Conclusion: There are
considerable variations in sepsis care among EDs in Hong Kong. More
training, resources, and research efforts should be directed to early ED
sepsis care, to improve patient outcomes.
New knowledge added by this study
- Large variations were found in practice and adoption of international sepsis recommendations across emergency departments (EDs) in Hong Kong. Fewer than half of the EDs had sepsis management guidelines, and there were no regular audits or any registry to monitor the performance of sepsis care.
- Although sepsis was perceived as the leading cause of in-hospital mortality, and second only to trauma in terms of preventable mortality, sepsis has not received a high level of attention within EDs.
- Many EDs specified the requirements for early intravenous antibiotics administration and stocked antibiotics, but they differed in terms of the methods and screening criteria used for identification of patients with sepsis.
- Sepsis, an emergency condition with high mortality that requires timely intervention, continues to lack adequate attention and resource allocation within EDs in Hong Kong. Now is a critical time to review whether performance indicators for sepsis should be formalised.
- Previous sporadic quality improvement programmes were not adequate to address the high mortality of patients with sepsis who attend EDs. Sustained improvements in resources and training must be provided to improve care for patients with sepsis in Hong Kong.
- By overcoming barriers including the lack of knowledge among ED staff and the need for standard screening to be implemented, EDs in Hong Kong have the capacity to provide a higher standard of care for sepsis patients.
Introduction
The global incidence rates of hospital-treated
sepsis and severe sepsis have been estimated as 437 and 270 cases per 100
000 person years, respectively,1
accounting for 17% and 26% of hospital mortality, respectively. The same
study estimated that 31.5 million cases of sepsis and 19.4 million cases
of severe sepsis account for 5.3 million deaths annually worldwide.1 The ageing of the population and the increasing number
of people living with co-morbid conditions are believed to be important
factors associated with the increasing incidence of sepsis.2
In early 2016, sepsis was re-defined as
‘life-threatening organ dysfunction caused by a dysregulated host response
to infection’ (Sepsis-3).3 The
criteria used for identifying patients with sepsis were also updated, with
the removal of the original systemic inflammatory response syndrome
criteria that had been used since the early 1990s. The Sequential Organ
Failure Assessment (SOFA) score is commonly used in intensive care units
(ICUs) for assessment of organ dysfunction. The quickSOFA (qSOFA) score
has been proposed as a bedside screening tool for patients at risk of
sepsis with adverse outcomes in emergency departments (EDs) and other
non-ICU settings. The evidence base for such a proposal is accumulating,4 and the optimal screening tool for
sepsis in EDs has not yet been identified.5
6 7
8
The recent ProCESS,9
ProMISE,10 and ARISE trials11 confirmed the importance of early recognition with
fluid resuscitation and appropriate antibiotic therapy in improving sepsis
outcomes. These trials refuted the need for strict adherence to the
haemodynamic goals proposed by Rivers et al in 2001 as early goal-directed
therapy.12 Although it is
generally agreed that early initiation of therapy is key to surviving
sepsis, controversies remain regarding the initial rate and choice of
fluids, the role and choice of inotropes, the identification of infection
sources with imaging and other techniques, the use of appropriate
antibiotics, and the optimal microbiological workup.13 14 15 16 17
The ED occupies a critical position in a patient’s
journey of sepsis care and plays an important role in the early
identification and treatment of sepsis.17
Despite frequent encounters with sepsis in EDs, few studies in Hong Kong
have investigated sepsis care. Yang et al18
studied patients with sepsis and septic shock in a tertiary university
teaching hospital and found no significant change in the in-hospital
mortality rate after the implementation of sepsis guidelines
(pre-implementation: 29.6% in 2009; post-implementation: 35.3% in 2010).
Although a significant proportion (25.5% in 2009 and 40.2% in 2010) of the
recruited patients had hypoperfusion (mean arterial pressure <65 mm Hg
or lactate >4 mmol/L), only 10.4% to 11.8% had blood cultures drawn,
13.0% to 23.5% had antibiotics administered, and 24.5% to 29.6% had fluid
resuscitation initiated in the ED. In that study, sepsis was recognised in
the ED in only two-thirds of the patients with sepsis who presented there.
Tse et al19 reported similar
findings in their study on the impact of departmental sepsis guidelines on
mortality (pre-implementation mortality: 25.8%; post-implementation
mortality: 33%), although there were improved rates of blood culture
collection and antibiotic administration in the ED after its
implementation. Overall, 17.2% of patients required direct ICU admission.
Those studies highlighted a few important issues
regarding sepsis care in Hong Kong EDs: a heavy burden of sepsis, low
compliance with treatment guidelines, and poor patient outcomes despite
efforts to standardise care. Evidently, implementing sepsis guidelines is
insufficient, and there is a need to evaluate the whole process of care
systematically. Moreover, those previous studies involved only individual
EDs and, thus, might not be representative of other EDs. Furthermore, the
adoption of international recommendations about sepsis care and the impact
of the new Sepsis-3 definitions on ED practice are not known. We therefore
conducted a survey to evaluate the process of sepsis care, the uptake of
international recommendations and the Sepsis-3 definitions to departmental
sepsis guidelines, and the barriers faced by health care providers in
public EDs in Hong Kong.
Methods
This was a cross-sectional survey across all EDs in
Hong Kong in 2017. All 18 public EDs under the Hospital Authority were
invited to participate. Private EDs and 24-hour out-patient departments
were excluded because 90% of in-patient care is provided by public
hospitals in Hong Kong. One representative was nominated by the Chief of
Service (medical director) of each ED to speak on behalf of the
department, but not individuals. The telephone survey was based on an
interview guide provided before the interview (online supplementary Appendix).
Interview guide development
The interview guide was developed by the study team
with the structure recommended by the UK Sepsis Trust “Exemplar Standards
for the Emergency Management of Sepsis”.20
It included nine domains: departmental guidelines on sepsis, screening
criteria for sepsis, physical location and resources, sepsis care and
microbiology, antibiotics availability and antimicrobial guidelines,
support from ICU and other departments, factors affecting the level of
care provided, priority of audits and research, and training and quality
assurance.
Telephone interview
One investigator (KH) performed all of the
telephone interviews from January to August 2017. Email invitations were
sent to the Chiefs of Services of all 18 departments 2 to 3 weeks before
the telephone interviews, and all participating departments were asked to
provide their prevailing sepsis guidelines (if available) before the
telephone interviews. Departments that had not responded were contacted
again up to a total of 4 times.
Data analysis
All telephone interviews were audio recorded after
obtaining consent. Interview data were recorded using a standardised data
collection sheet, and data were entered into an Excel spreadsheet.
Descriptive statistics were presented as medians for continuous variables
(unless specified otherwise) and percentage proportions for categorical
variables. Participants ranked each of the nine barriers to sepsis care
using a 5-point Likert scale (‘not important’ 1; ‘slightly important’ 2;
‘important’ 3; ‘fairy important’ 4; and ‘very important’ 5).
Results
Out of the 18 EDs, 16 agreed to participate. One
department declined to participate, and one did not respond after repeated
contacts.
Departmental guidelines on sepsis
Seven departments reported the presence of sepsis
guidelines in their EDs, with three of these departments using the same
regional guidelines. Therefore, five different sets of sepsis guidelines
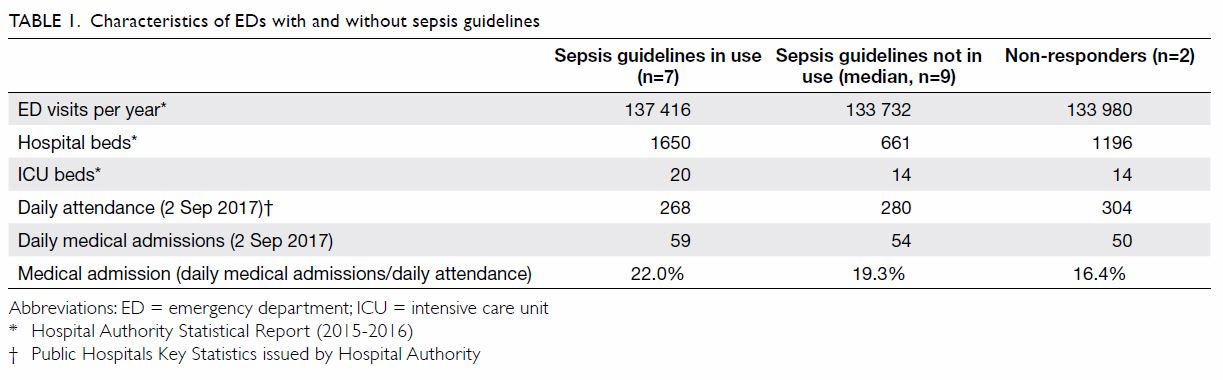
were reported to be in current use across all public EDs in Hong Kong. Table 1 shows the characteristics of the EDs with
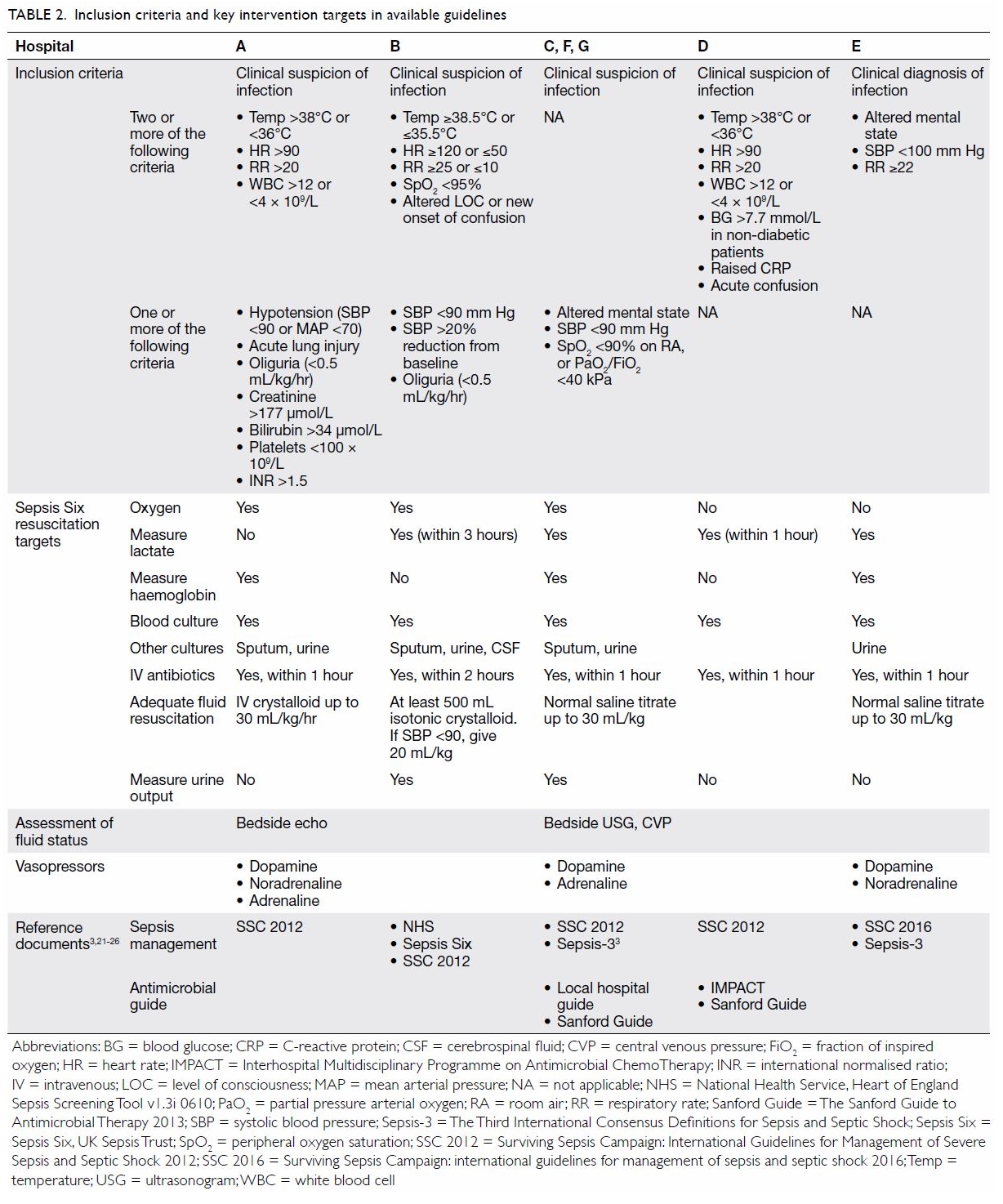
and without sepsis guidelines. Table 23 21 22
23 24
25 26
summarises the core components of the five sets of guidelines reported.
Most of the current versions of the guidelines were implemented between
2014 and 2017.
Screening criteria for sepsis
Four out of the seven departments with sepsis
guidelines used qSOFA, which is based on the Sepsis-3 recommendations.
Three departments (which used the same regional guidelines) used modified
qSOFA criteria. The reasons for this, as reported by respondents, included
the concern that replacing the definition of ‘severe sepsis’ with a qSOFA
score might increase the number of cases screened as positive. This would
result in an increased number of cases requiring management in
resuscitation rooms and put further strain on the already scarce ED human
resources.
The use of lactate as a biomarker for clinical
decision making in sepsis care was uncommon in the surveyed EDs. Fourteen
out of the 16 EDs had access to point-of-care testing of blood gases
inside the department, but only five had a lactate module. The ED
physicians mainly rely on patients’ vital signs and clinical assessment to
facilitate recognition of sepsis.
Physical location and resources
Upon identification of sepsis, two of the EDs’
guidelines explicitly mentioned sending the patient to a resuscitation
room (or a bed with intensive monitoring, eg, a high-dependency unit).
Most of the surveyed EDs (13 of 16) routinely managed patients with sepsis
in their resuscitation rooms. None of the EDs had a designated team or a
code specifically for patients with sepsis, unlike the management of major
trauma, for which the EDs employed a trauma team approach. One of the EDs
had designed a sepsis kit consisting of antiseptic swab sticks and pre-set
blood collection tubes and had investigation shortcuts in the computer
system to facilitate implementation of the guidelines.
Sepsis care and microbiology
Regarding the resuscitation and stabilisation of
patients with sepsis, Table 2 highlights the key areas covered by the
existing guidelines. All sets of guidelines refer to the Surviving Sepsis
Campaign targets21 22 or the UK Sepsis Six targets.23 All sets of guidelines also mention time to
intravenous antibiotics and microbiological workup, including blood
cultures, with the majority specifying intravenous antibiotics within 1
hour of the patient’s arrival.
Most EDs (13 of 16) expressed a preference to use
normal saline or other isotonic crystalloids for fluid resuscitation. The
target volume is up to 20 to 30 mL/kg, with monitoring of the patient’s
blood pressure (especially mean arterial pressure) for fluid
responsiveness. The use of ultrasonograms was reported to be increasing,
especially bedside echocardiograms and inferior vena cava variability, to
assess patients’ fluid status. Central venous pressure was mentioned, but
its use by ED physicians was perceived to be decreasing in frequency. If
vasopressors or inotropes were needed, dopamine was the most common
choice, as it can be administered via peripheral veins.
Concerning source identification for sepsis, most
sets of guidelines (4 of 5) mentioned chest X-rays and urinalysis. If
abdominal sepsis was suspected, some EDs would consult their surgical
colleagues and make a joint decision as to when a computed tomography (CT)
scan or further imaging may be necessary. Individual departments have
large variation in access to CT scans.
Antibiotic availability within the emergency department
and antimicrobial guidelines
All responding EDs reported that antibiotics were
stocked in their departments. The numbers of different antibiotics stocked
in the EDs ranged from 3 to 18, with a median of 8.5. The choice of
antibiotics stocked depended on the individual departments’ antimicrobial
guidelines or regional patterns of pathogen and antibiotic resistance.
Both the penicillin and cephalosporin groups were present in all EDs,
followed in frequency by fluoroquinolones (14 of 16), others (13 of 16),
aminoglycosides (12 of 16), carbapenems (9 of 16), and macrolides (2 of
16).
Support from the intensive care unit and other
departments
Organ failure and septic shock are frequent
indications for ICU admission. However, direct ICU admission of patients
with single organ failure from EDs is determined by individual ICU
admission policy and bed availability. Support from the ICU and in-patient
wards varies across different EDs. During the winter surge and flu
seasons, access to hospital beds is reduced, causing both ED congestion
and compromised sepsis care, especially for those with stable vital signs
or poor premorbid conditions. In some of the surveyed hospitals (4 of 16),
laboratory and pharmacy support for sepsis care after office hours is
limited. This means that those EDs need to dispense drugs or manage
patients without the results of certain laboratory investigations.
Training, audit, and research for sepsis
In terms of training, audits, and research, most of
the surveyed EDs (14 of 16) provided ad hoc training on sepsis management
to physicians and nurses, but none had a specific sepsis outcome audit or
registry. Even though two local studies18
19 provided some insight into
previous sepsis-related mortality, there has been no agreement regarding
standardisation of coding or key performance indicators across different
departments.
Factors affecting the level of care provided
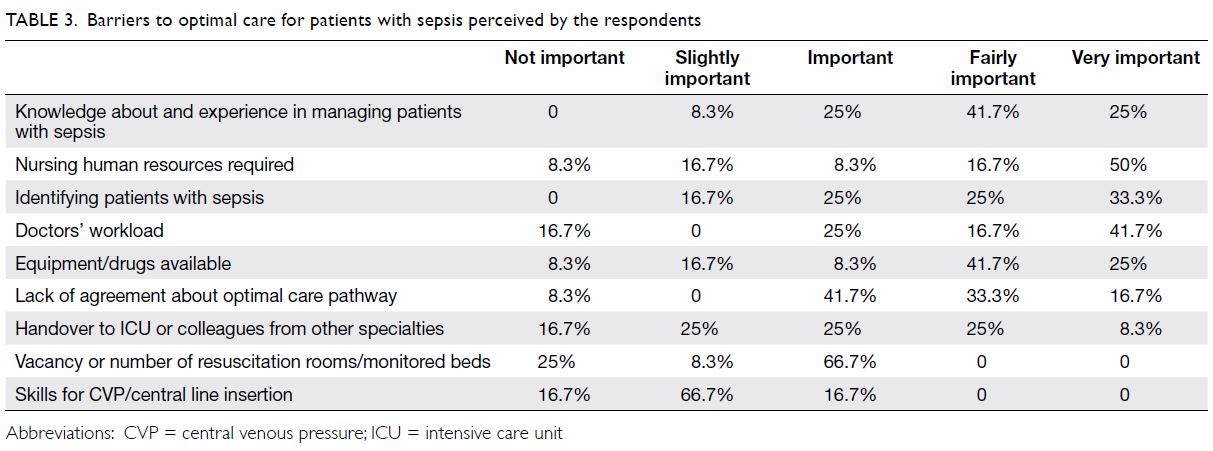
Compared with other time-critical medical
emergencies, the respondents perceived sepsis to be the leading cause of
in-hospital mortality (average: 4.17), followed by acute coronary syndrome
(4.09), stroke (3.00), trauma (2.58), and poisoning (1.08). When the
respondents were asked which time-critical emergencies had the highest
rates of preventable mortality that was not well managed in the ED, trauma
was rated the highest (4.00), followed closely by sepsis (3.42), poisoning
(2.92), stroke (2.42), and acute coronary syndrome (2.25). The top
barriers to optimal sepsis care in EDs identified by the respondents were
lack of knowledge and experience and inadequate nursing human resources,
followed by difficulty identifying patients with sepsis. Table
3 lists all of the barriers investigated by the survey and their
perceived importance.
Discussion
In this study, we found varying levels of adoption
of international sepsis guidelines among the responding EDs. Sepsis was
perceived to be the top cause of in-hospital mortality and the second
leading cause of preventable mortality among all time-critical
emergencies. Few EDs had adopted the qSOFA score (which is based on the
Sepsis-3 recommendations) in patient screening at 1 year after its
publication. Early intravenous antibiotic administration within 1 to 2
hours was mandatory according to all of the surveyed EDs’ sepsis
guidelines, and all responding EDs reported that antibiotics were stocked
within their departments.
Emergency departments across the world have an
important responsibility to recognise patients with sepsis, as delays in
treatment and administration of antibiotics have been shown to increase
in-hospital mortality.27 All
responding public EDs had antibiotics available on-site, but few provided
clear guidance on which patients might benefit from timely intravenous
antibiotic administration except those with neutropenic or
post-chemotherapy fever. The widespread availability of intravenous
antibiotics across the EDs is likely a result of the recent Hospital
Authority review on acute management of neutropenic fever. All of the
participating EDs reported the use of either departmental or cluster-wide
guidelines for neutropenic fever, and the latest version of the Hospital
Authority triage guidelines emphasises the importance of its early
recognition and assigns a higher priority to patients with suspected
neutropenic fever.28 Despite
previous studies in Hong Kong that demonstrated high mortality rates among
patients with sepsis without neutropenia,18
19 sepsis generally does not
receive the same level of attention as neutropenia in Hong Kong EDs. To
improve patient outcomes, more emphasis should be placed on early
resuscitation and antibiotic therapy for sepsis in EDs.
Sustained improvement in sepsis care requires not
only guidelines but also more resources and staff training. Further, EDs
in Hong Kong face many challenges such as access blockages and
overcrowding.29 With the rising
level of service demand and competing priorities in EDs, it is important
to understand the barriers to better sepsis care from health care
providers’ perspectives. Our study highlights several challenges. The top
barriers reported included a lack of knowledge and experience, nursing
human resources shortages, and difficulty identifying patients with
sepsis. These findings are similar to those of Carlbom and Rubenfeld,30 who reported a lack of nursing staff, challenges in
the identification of patients with sepsis, and problems with central
venous pressure monitoring as barriers to optimal sepsis care. For
effective changes to take place, it is necessary to overcome these
barriers with more staff training, better nursing human resources
provision in EDs, elevation of staff awareness of sepsis, and provision of
useful bedside tools for sepsis recognition.
The UK Sepsis Six and quality improvement projects
in the UK shed light on how sustained reductions in sepsis mortality can
be achieved in a publicly funded health system similar to that of Hong
Kong.31 In the United States, New
York State has required hospitals to follow a sepsis protocol since 2013.
Results from 2014 to 2016 showed that 82.5% of patients across 149
hospitals had the 3-hour bundle of care (blood cultures, broad-spectrum
antibiotics, and lactate measurement) completed within 3 hours, with a
median time to completion of 1.3 hours.32
Steady improvements in survival of other
time-critical emergencies including ST elevation myocardial infarction,33 acute ischemic stroke,34 and major trauma35
have been achieved in Hong Kong through systemic changes, more staff
training and resources, multidisciplinary collaboration, and regular
interdepartmental audits. Regular and systematic data collection from EDs
in Hong Kong for monitoring, evaluation of performance and processes of
care, and benchmarking is important to assess the impact of various ED
sepsis initiatives.
Limitations
This study has a number of limitations. Not all
public EDs in Hong Kong participated in the study. However, we believe
that our findings are representative of the current ED processes of sepsis
care in Hong Kong. We did not include other private EDs, which might
affect the generalisability of our findings; however, ambulances in Hong
Kong bring patients to public EDs only, and 90% of all in-patient care is
provided by public hospitals. We have likely covered the majority of the
EDs in Hong Kong that provide emergency care to patients with sepsis,
especially those in critical condition.
Second, it is possible that some respondents might
have expressed personal bias when responding to the questions, especially
those regarding the barriers to optimal sepsis care. This could have
affected the results despite the fact that respondents were reminded that
their replies should provide the views of the department (not their
personal points of view), and even though the interview guide was shared
in advance to consolidate departmental opinions. Individual questionnaires
targeting various seniority levels of ED staff might be better to address
these questions in the future.
Finally, we relied heavily on the materials
provided by the respondents, and their views do not necessarily reflect
real clinical practice. However, this provides a beginning to facilitate a
better systematic understanding of sepsis care in Hong Kong EDs as a
whole. Future studies are warranted to evaluate actual clinical practice,
patient outcomes in cases of sepsis, and the impact of adopting new sepsis
definitions and international guidelines on a territory-wide basis.
Conclusion
Compared with other time-critical emergencies with
high mortality and impact on patients, sepsis has not received adequate
attention in Hong Kong EDs. The process of care varies considerably among
EDs, and few have departmental sepsis guidelines. With increasing
recognition of the burden of sepsis among Hong Kong EDs, more training and
resources for management of these patients and the establishment of formal
performance indicators should be considered. Systematic routine data
collection for prospective multicentre research is needed to improve
patient care.
Author contributions
Concept and design: KKC Hung, RPK Lam, RSL Lo, CA
Graham.
Acquisition of data: KKC Hung, RPK Lam, MLC Yang, MCK Tai.
Analysis and interpretation of data: KKC Hung, JW Tenney.
Drafting of the article: KKC Hung, RPK Lam.
Critical revision for important intellectual content: All authors.
Acquisition of data: KKC Hung, RPK Lam, MLC Yang, MCK Tai.
Analysis and interpretation of data: KKC Hung, JW Tenney.
Drafting of the article: KKC Hung, RPK Lam.
Critical revision for important intellectual content: All authors.
Acknowledgement
We thank all of the participants for their time and
support of this study.
Declaration
All authors have disclosed no conflicts of
interest. All authors had full access to the data, contributed to the
study, approved the final version for publication, and take responsibility
for its accuracy and integrity.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Ethical approval
Ethical approval was obtained from the Survey and
Behavioural Research Ethics Committee of the Chinese University of Hong
Kong (097-16). Verbal informed consent was obtained from the participants.
References
1. Fleischmann C, Scherag A, Adhikari NK,
et al. Assessment of global incidence and mortality of hospital-treated
sepsis. Current estimates and limitations. Am J Respir Crit Care Med
2016;193:259-72. Crossref
2. Kempker JA, Martin GS. The changing
epidemiology and definitions of sepsis. Clin Chest Med 2016;37:165-79. Crossref
3. Singer M, Deutschman CS, Seymour CW, et
al. The Third International Consensus Definitions for Sepsis and Septic
Shock (Sepsis-3). JAMA 2016;315:801-10. Crossref
4. Churpek MM, Snyder A, Han X, et al.
Quick sepsis-related organ failure assessment, systemic inflammatory
response syndrome, and early warning scores for detecting clinical
deterioration in infected patients outside the intensive care unit. Am J
Respir Crit Care Med 2017;195:906-11. Crossref
5. Lo RS, Brabrand M, Kurland L, Graham CA.
Sepsis—where are the emergency physicians? Eur J Emerg Med 2016;23:159. Crossref
6. Kaukonen KM, Bailey M, Pilcher D, Cooper
DJ, Bellomo R. Systemic inflammatory response syndrome criteria in
defining severe sepsis. N Engl J Med 2015;372:1629-38. Crossref
7. Vincent JL, Martin GS, Levy MM. qSOFA
does not replace SIRS in the definition of sepsis. Crit Care 2016;20:210.
Crossref
8. Macdonald SP, Arendts G, Fatovich DM,
Brown SG. Comparison of PIRO, SOFA, and MEDS scores for predicting
mortality in emergency department patients with severe sepsis and septic
shock. Acad Emerg Med 2014;21:1257-63. Crossref
9. ProCESS Investigators, Yealy DM, Kellum
JA, et al. A randomized trial of protocol-based care for early septic
shock. N Engl J Med 2014;370:1683-93. Crossref
10. Mouncey PR, Osborn TM, Power GS, et
al. Trial of early, goal-directed resuscitation for septic shock. N Engl J
Med 2015;372:1301-11. Crossref
11. ARISE Investigators, ANZICS Clinical
Trials Group, Peake SL, et al. Goal-directed resuscitation for patients
with early septic shock. N Engl J Med 2014;371:1496-506. Crossref
12. Rivers E, Nguyen B, Havstad S, et al.
Early goal-directed therapy in the treatment of severe sepsis and septic
shock. N Engl J Med 2001;345:1368-77. Crossref
13. Gotts JE, Matthay MA. Sepsis:
pathophysiology and clinical management. BMJ 2016;353:i1585. Crossref
14. Cohen J, Vincent JL, Adhikari NK, et
al. Sepsis: a roadmap for future research. Lancet infect Dis
2015;15:581-614. Crossref
15. Andrews B, Semler MW, Muchemwa L, et
al. Effect of an early resuscitation protocol on in-hospital mortality
among adults with sepsis and hypotension: a randomized clinical trial.
JAMA 2017;318:1233-40. Crossref
16. McIntyre L, Rowe BH, Walsh TS, et al.
Multicountry survey of emergency and critical care medicine physicians’
fluid resuscitation practices for adult patients with early septic shock.
BMJ Open 2016;6:e010041. Crossref
17. Lam SM, Lau AC, Lam RP, Yan WW.
Clinical management of sepsis. Hong Kong Med J 2017;23:296. Crossref
18. Yang ML, Graham CA, Rainer TH. Outcome
after implementation of sepsis guideline in the emergency department of a
university hospital in Hong Kong. Hong Kong J Emerg Med 2015;22:163-71. Crossref
19. Tse CL, Lui CT, Wong CY, Ong KL, Fung
HT, Tang SY. Impact of a sepsis guideline in emergency department on
outcome of patients with severe sepsis. Hong Kong J Emerg Med
2017;24:123-31. Crossref
20. Nutbeam T, Daniels R, Keep J; for the
UK Sepsis Trust. Toolkit: emergency department management of sepsis in
adults and young people over 12 years—2016. Available from:
https://sepsistrust.org/wp-content/uploads/2018/06/ED-toolkit-2016-Final-1.pdf.
Accessed 4 May 2018. Crossref
21. Dellinger RP, Levy MM, Rhodes A, et
al. Surviving Sepsis Campaign: International Guidelines for Management of
Severe Sepsis and Septic Shock, 2012. Intensive Care Med 2013;39:165-228.
Crossref
22. National Health Service UK. Sepsis
guidance implementation advice for adults. Available from:
https://www.england.nhs.uk/wp-content/uploads/2017/09/sepsis-guidance-implementation-advice-for-adults.pdf.
Accessed
3 Nov 2018.
23. Daniels R, Nutbeam T, McNamara G,
Galvin C. The sepsis six and the severe sepsis resuscitation bundle: a
prospective observational cohort study. Emerg Med J 2011;28:507-12. Crossref
24. Gilbert DN, Moellering RC, Eliopoulos
GM, Chambers HF, Saag MS. The Sanford Guide to Antimicrobial Therapy. 42nd
ed. Antimicrobial Therapy Inc; 2012.
25. Ho PL, Wong SS. Reducing bacterial
resistance with IMPACT—Interhospital Multi-disciplinary Programme on
Antimicrobial ChemoTherapy. Hong Kong: Centre for Health Protection; 2012.
26. Rhodes A, Evans LE, Alhazzani W, et
al. Surviving Sepsis Campaign: International Guidelines for Management of
Sepsis and Septic Shock: 2016. Intensive Care Med 2017;43:304-77. Crossref
27. Seymour CW, Kahn JM, Martin-Gill C, et
al. Delays from first medical contact to antibiotic administration for
sepsis. Crit Care Med 2017;45:759-65. Crossref
28. A&E Triage Guidelines version 5.
Hong Kong: Hospital Authority; 2016.
29. Chan SS, Cheung NK, Graham CA, Rainer
TH. Strategies and solutions to alleviate access block and overcrowding in
emergency departments. Hong Kong Med J 2015;21:345-52. Crossref
30. Carlbom DJ, Rubenfeld GD. Barriers to
implementing protocol-based sepsis resuscitation in the emergency
department—results of a national survey. Crit Care Med 2007;35:2525-32. Crossref
31. Bentley J, Henderson S, Thakore S,
Donald M, Wang W. Seeking sepsis in the emergency department-identifying
barriers to delivery of the Sepsis 6. BMJ Qual Improv Rep
2016;5:u206760.w3983.
32. Seymour CW, Gesten F, Prescott HC, et
al. Time to treatment and mortality during mandated emergency care for
sepsis. N Engl J Med 2017;376:2235-44. Crossref
33. Cheung GS, Tsui KL, Lau CC, et al.
Primary percutaneous coronary intervention for ST elevation myocardial
infarction: performance with focus on timeliness of treatment. Hong Kong
Med J 2010;16:347-53.
34. Wong EH, Yu SC, Lau AY, et al.
Intra-arterial revascularisation therapy for acute ischaemic stroke:
initial experience in a Hong Kong hospital. Hong Kong Med J
2013;19:135-41.
35. Cheung NK, Yeung JH, Chan JT, Cameron
PA, Graham CA, Rainer TH. Primary trauma diversion: initial experience in
Hong Kong. J Trauma 2006;61:954-60. Crossref