Hong
Kong Med J 2018 Aug;24(4):426.e1-2
DOI: 10.12809/hkmj176876
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
Emphysematous epididymo-orchitis: an uncommon but
life-threatening cause of scrotal pain
HW Lau, MB, ChB, FRCR1; CH Yu, MB, ChB1;
SM Yu, FRCR, FHKCR2; LF Lee, MB, ChB3
1 Department of Radiology, Tuen Mun
Hospital, Tuen Mun, Hong Kong
2 Department of Radiology, United
Christian Hospital, Kwun Tong, Hong Kong
3 Division of Urology, Department of
Surgery, United Christian Hospital, Kwun Tong, Hong Kong
Corresponding author: Dr HW Lau (jackylauhw@gmail.com)
An 80-year-old man presented to the emergency
department in August 2016 with a 2-day history of painful scrotal swelling
and fever. There was no history of trauma. He had a history of
hypertension, diabetes mellitus and bullous pemphigoid, and was taking
long-term steroid therapy. Upon presentation, the patient had a fever of
38.8°C and fast atrial fibrillation with a heart rate of 170 beats per
minute. Blood pressure was 149/104 mm Hg. Physical examination of the
patient revealed scrotal skin erythema and a firm left scrotal swelling
that was tender on palpation. No cough impulse could be elicited. His
white cell count was 21.8 × 109 /L and blood glucose level was 21.6
mmol/L. Ultrasound of the left hemiscrotum showed a fluid collection with
hyperechoic interfaces and ring-down artefact suggestive of the presence
of gas, obscuring the underlying structures (Fig 1). Subsequent non-contrast computed tomographic
scan of the pelvis confirmed that the mottled gas and fluid density were
confined to the left hemiscrotum (Fig 2a). The left testis and epididymis were poorly
delineated. There was no gas density in the subcutaneous layer of the
scrotum or perineum or in the intraperitoneal cavity. There was also no
evidence of indirect inguinal hernia (Fig 2b). A diagnosis of emphysematous
epididymo-orchitis was made. Emergency surgery was arranged a few hours
after imaging. Intra-operatively, gas and pus were seen within the left
tunica vaginalis. The left epididymis was necrotic and almost destroyed
but the left testis was relatively spared with friable tissue and patches
of necrosis (Fig 3). Drainage of pus and left orchidectomy were
performed. Pus culture revealed Escherichia coli. The patient
subsequently developed septic shock and died 3 days after the operation.
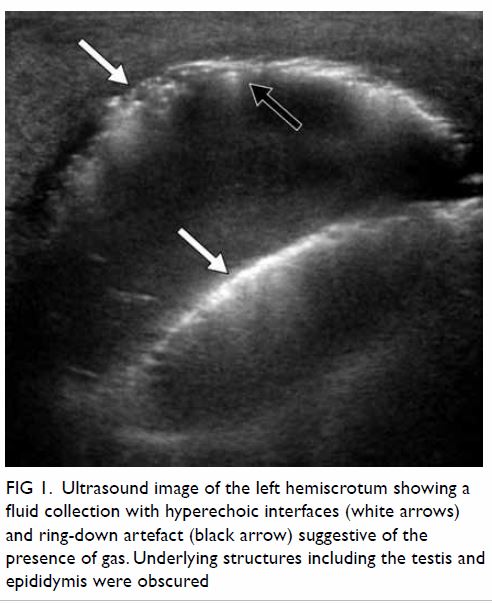
Figure 1. Ultrasound image of the left hemiscrotum showing a fluid collection with hyperechoic interfaces (white arrows) and ring-down artefact (black arrow) suggestive of the presence of gas. Underlying structures including the testis and epididymis were obscured
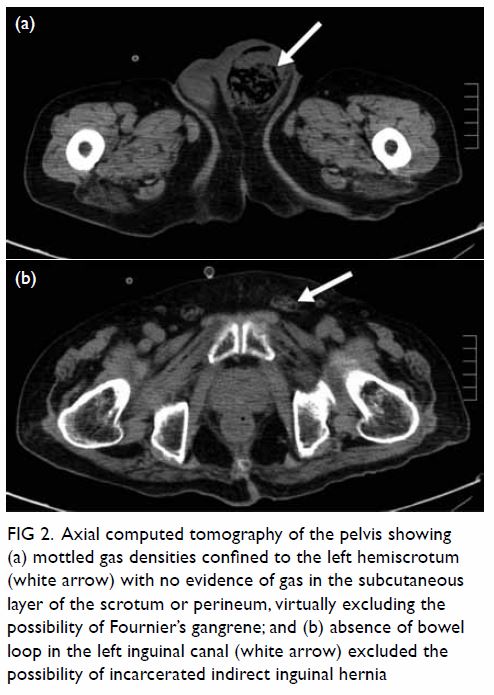
Figure 2. Axial computed tomography of the pelvis showing (a) mottled gas densities confined to the left hemiscrotum (white arrow) with no evidence of gas in the subcutaneous layer of the scrotum or perineum, virtually excluding the possibility of Fournier’s gangrene; and (b) absence of bowel loop in the left inguinal canal (white arrow) excluded the possibility of incarcerated indirect inguinal hernia
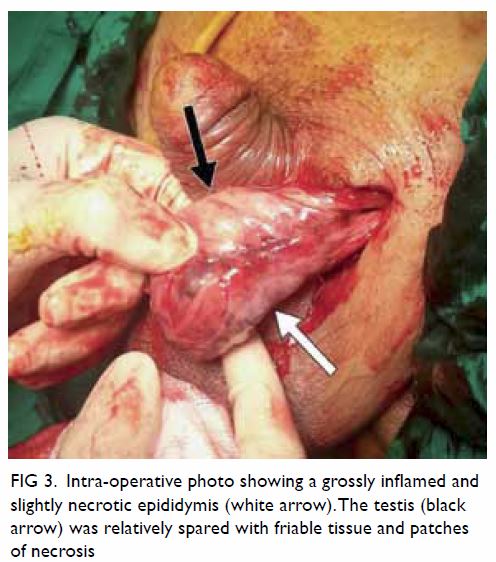
Figure 3. Intra-operative photo showing a grossly inflamed and slightly necrotic epididymis (white arrow). The testis (black arrow) was relatively spared with friable tissue and patches of necrosis
Emphysematous cholecystitis, pyelonephritis, and
cystitis are not uncommonly seen in patients with poorly controlled
diabetes mellitus. It is nonetheless rare to see gas-forming infection of
the epididymis and testis although this is also reported to be associated
with diabetes mellitus.1 2 3 Long-term use
of steroid in our patient may have been an additional risk factor due to
immunosuppression. Based on the clinical presentation and ultrasound
findings of our patient, the main differential diagnoses included
Fournier’s gangrene and incarcerated indirect inguinal hernia. Computed
tomographic scan was very helpful in delineating the definitive diagnosis.
Gas pockets confined to the scrotal sac without involvement of the
subcutaneous layer of the perineum virtually excluded the possibility of
Fournier’s gangrene. Incarcerated indirect inguinal hernia was excluded
due to the absence of bowel loops in the scrotal sac.
When a diabetic patient presents with acute scrotal
pain and features of infection, careful examination during the initial
ultrasound scan for the presence of gas within the scrotum is essential as
this will alter the subsequent management plan as it implies a much poorer
prognosis than non–gas-forming epididymo-orchitis.
In conclusion, emphysematous epididymo-orchitis is
an uncommon but life-threatening disease. Ultrasound and computed
tomographic scan are essential to identify this entity for early
treatment.
Author contributions
All authors have made substantial contributions to
the concept or design of this study; acquisition of data; analysis or
interpretation of data; drafting of the article; and critical revision for
important intellectual content.
Funding/support
This research received no specific grant from any
funding agency in the public, commercial, or not-for-profit sectors.
Declaration
All authors have disclosed no conflicts of
interest. All authors had full access to the data, contributed to the
study, approved the final version for publication, and take responsibility
for its accuracy and integrity.
References
1. Mathur A, Manish A, Maletha M, Luthra
NB. Emphysematous epididymo-orchitis: a rare entity. Indian J Urol
2011;27:399-400. Crossref
2. Mandava A, Rao RP, Kumar DA, Naga Prasad
IS. Imaging in emphysematous epididymo-orchitis: a rare cause of acute
scrotum. Indian J Radiol Imaging 2014;24:306-9. Crossref
3. Hegde RG, Balani A, Merchant SA, Joshi
AR. Synchronous infection of the aorta and the testis: emphysematous
epididymo-orchitis, abdominal aortic mycotic aneurysm, and testicular
artery pseudoaneurysm diagnosed by use of MDCT. Jpn J Radiol
2014;32:425-30. Crossref

