Hong Kong Med J 2018 Apr;24(2):145–51 | Epub 14 Mar 2018
DOI: 10.12809/hkmj176804
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Intra-operative periarticular multimodal injection in
total knee arthroplasty: a local hospital experience in Hong Kong
Jason CH Fan, FHKAM (Orthopaedic Surgery)
Department of Orthopaedics and Traumatology, Alice
Ho Miu Ling Nethersole Hospital, Tai Po, Hong Kong
Corresponding author: Dr Jason CH Fan (fchjason@gmail.com)
Abstract
Introduction: Data from a local
report revealed the superior outcome of regional anaesthesia and
analgesia compared with general anaesthesia and intravenous
patient-controlled analgesia in total knee arthroplasty. This
retrospective study aimed to assess the efficacy of intra-operative
periarticular multimodal injection in improving postoperative pain and
reducing morphine consumption with patient-controlled analgesia after
total knee arthroplasty in patients with knee osteoarthritis.
Methods: From July 2005 to May
2009, 213 total knee arthroplasties without intra-operative
periarticular multimodal injection (control group) were performed at a
local hospital. From June 2009 to December 2012, 185 total knee
arthroplasties were performed with intra-operative periarticular
multimodal injection (cocktail group). The inclusion criteria were
osteoarthritis of the knee, single method of anaesthesia (general or
neuraxial), simple total knee arthroplasty without any metal
augmentation or constraint, and postoperative patient-controlled
analgesia. Postoperative patient-controlled morphine doses were
compared.
Results: A total of 152 total
knee arthroplasties were recruited to the cocktail group, and 89 to the
control group. Duration of tourniquet application and preoperative knee
score did not significantly correlate with morphine consumption by
patient-controlled analgesia. Multimodal injection significantly
decreased such consumption for 36 h. When injection was separately
analysed for general and neuraxial anaesthesia, the effect lasted for 42
h and 24 h, respectively.
Conclusion: Intra-operative
periarticular multimodal injection decreased morphine consumption for up
to 42 h postoperatively.
New knowledge added by this study
- Intra-operative periarticular multimodal injection in total knee arthroplasty could decrease parenteral morphine consumption for up to 42 hours.
- Intra-operative periarticular multimodal injection should be adopted as a standard local practice for postoperative pain control. This practice may be extended to operations other than total knee arthroplasty.
Introduction
Postoperative pain following total knee
arthroplasty (TKA) is reported to be severe in approximately 60% of
patients and moderate in approximately 30%.1
It is associated with arthrofibrosis and diminished range of motion.2 3 Good pain
relief is important for rehabilitation following TKA.4 Many modes of perioperative and postoperative analgesia
are available, and involve various combinations of systemic and regional
analgesia. Intra-operative periarticular multimodal drug injection has
been well documented as an excellent method to alleviate postoperative
pain following TKA.5 6 7 Nonetheless,
a previous retrospective study5 and
a randomised trial6 that analysed
two different groups of patients with multiple diagnoses and multiple
anaesthetic methods revealed that the effect of periarticular injection
might have been affected by different causes of end-stage arthritis
leading to TKA. Different anaesthetic methods could also have affected
patients’ perception of pain and parenteral morphine consumption.
In 2006, Chu et al8
reported the superior outcome of regional anaesthesia and regionally
delivered analgesia compared with general anaesthesia (GA) and intravenous
patient-controlled analgesia (PCA) in TKA at the Alice Ho Miu Ling
Nethersole Hospital (AHNH). Since June 2009, intra-operative periarticular
multimodal injection (IPMI) consisting of an opioid (morphine), a
long-acting local anaesthetic (levobupivacaine) and epinephrine, has been
administered by surgeons to control postoperative pain following TKA. This
retrospective cohort study analysed the efficacy of IPMI in TKA and also
its effect following different types of anaesthesia.
Methods
Perioperative pain management
Before June 2009, postoperative pain following
primary TKA was managed by a combination of parenteral and oral analgesia.
The anaesthetist determined the choice of parenteral analgesia that
included regular or as-required subcutaneous morphine injection, PCA with
intravenous morphine injection, or epidural analgesia (EpA). Oral
paracetamol 1 g every 6 h was prescribed to all patients from day 1 to 3.
Since June 2009, IPMI has been routinely added, and comprises 20 mL of
0.5% levobupivacaine, 1 mL of 5 mg/mL morphine, 2 mL of 1:10000
adrenaline, and 17 mL of normal saline. In this study, half of this 40-mL
mixture was injected into the posterior capsule, collaterals, and
quadriceps incision before implantation of the prosthesis. The other half
was injected into the subcutaneous tissue after suturing of the
arthrotomy. All patients with PCA were assessed hourly for the first 24 h
to monitor vital signs, pain score, and patient-controlled analgesia
morphine consumption (PCAMC), and thereafter every 6 h for 2 more days.
Patient selection
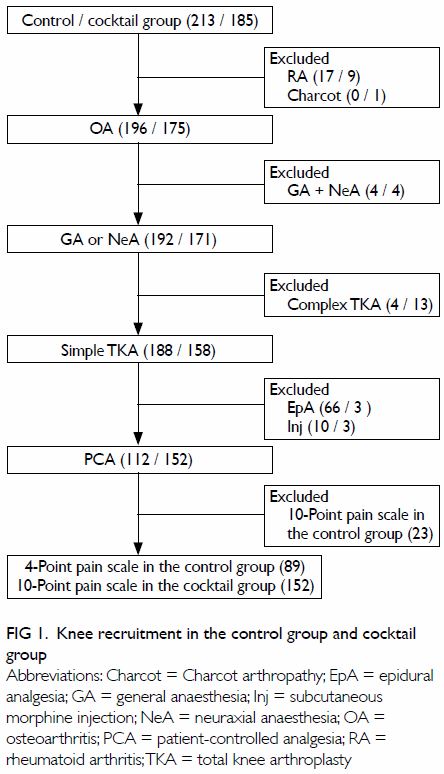
From July 2005 to May 2009, 213 TKAs without IPMI
(control group) were performed at AHNH. They included 196 knees with
osteoarthritis (OA) and 17 knees with rheumatoid arthritis. From June 2009
to December 2012, 185 TKAs were performed with IPMI (cocktail group).
There were 175 OA knees, nine rheumatoid arthritis knees, and one Charcot
knee.
All TKAs were performed through an anterior midline
incision and medial parapatellar arthrotomy with tourniquet pressure of
300 mm Hg. A cemented posterior stabilised model was used in all cases
except for two cases in the control group and nine cases in the cocktail
group where a semi-constrained TKA was performed. All operations were
performed under GA or neuraxial anaesthesia (NeA) that was either combined
spinal epidural or spinal anaesthesia. Four TKAs in the cocktail group and
four in the control group were performed with combined GA and NeA. A
closed-suction surgical drain was inserted and was routinely removed on
postoperative day 2.
For postoperative pain control in the control
group, PCA was used in 112 TKAs, EpA in 66 TKAs, and subcutaneous morphine
injections in 10 TKAs. A 4-point pain scale was completed by a pain nurse
to assess pain in 189 PCA patients before October 2008 and a 10-point pain
scale used in 23 PCA patients thereafter. In the cocktail group, 152 TKAs
were managed with PCA, three with EpA, and three with subcutaneous
morphine injections. Pain in all PCA patients was assessed by a 10-point
pain scale.
The inclusion criteria for this study were OA of
the knee, single method of anaesthesia of either GA or NeA, simple TKA
without any metal augmentation or constraint, and postoperative PCA. The
patients in the control group who were assessed by the 10-point pain scale
were excluded to ensure a common pain assessment tool for each group.
Method of data retrieval, analysis, and study
hypothesis
This was a retrospective cohort observational study
carried out in accordance with the principles outlined in the Declaration
of Helsinki. Informed patient consent was not required because it was a
record-based study that revealed no individual identities or sensitive
individual information. The medical records and electronic patient records
were traced and the necessary data—including demographic data, TKA model
and anaesthetic method, first 72-hour pain score and morphine consumption,
and postoperative complications—were entered into an electronic file by a
single member of staff blinded to the study hypothesis. The accuracy of
the data was selectively double-checked by the author. To enable
comparison, pain score was divided by 4 when the 4-point scale was used
and by 10 for the 10-point scale. Statistical Package for the Social
Sciences (Windows version 13.0; SPSS Inc, Chicago [IL], United States) was
used for analysis. The null hypothesis was that IPMI would not alleviate
postoperative pain and would not reduce PCAMC. The Chi squared test and
two-tailed independent t test were used to analyse categorical and
continuous data, respectively. The Pearson correlation test was used to
detect any relationship between cumulative PCAMC and tourniquet time, and
between PCAMC and preoperative knee score. Statistical significance was
set at P<0.05.
Results
Perioperative variables
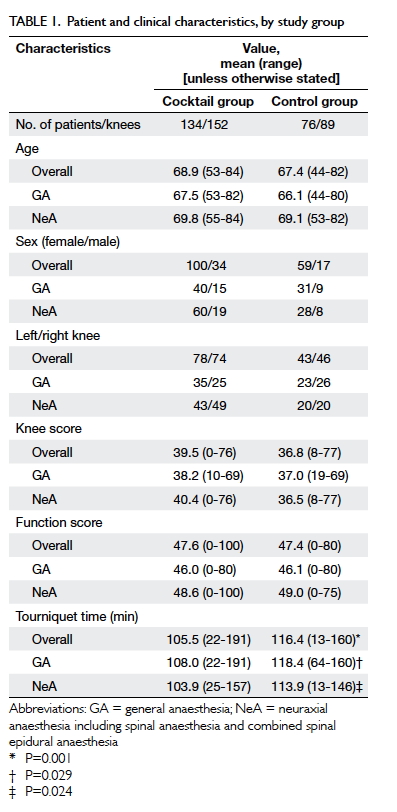
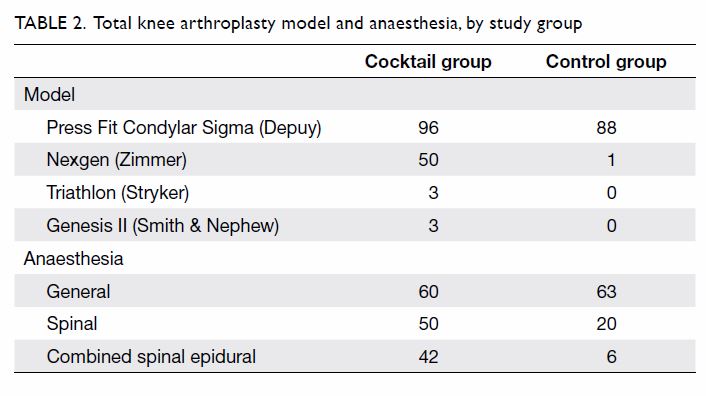
A total of 152 knees (134 patients) in the cocktail
group and 89 knees (76 patients) in the control group were recruited (Fig
1). Table 1 shows the demographic data and clinical
characteristics of patients, and Table 2 shows the models of primary TKAs and
anaesthetic methods. There was no statistically significant difference in
age, sex, the side operated on, and mean preoperative knee score or
function score between the cocktail and control groups. Tourniquet time
was significantly longer in the control group (P<0.05). There was no
correlation between tourniquet time and PCAMC for any postoperative period
(all correlation coefficients <0.1 and P>0.05). This indicated that
tourniquet time was not confounding. Preoperative knee score was not
correlated with PCAMC (all correlation coefficients <0.2 and
P>0.05). Comparison of the number of Press Fit Condylar Sigma and
non–Press Fit Condylar models between the two groups revealed a
statistical significance (P<0.001). However, all these models
substitute for the posterior cruciate ligament and have a similar design.
They were all used in primary simple TKA, and model type would not have
caused any difference in early postoperative pain perception.
Cumulative patient-controlled analgesia morphine
consumption
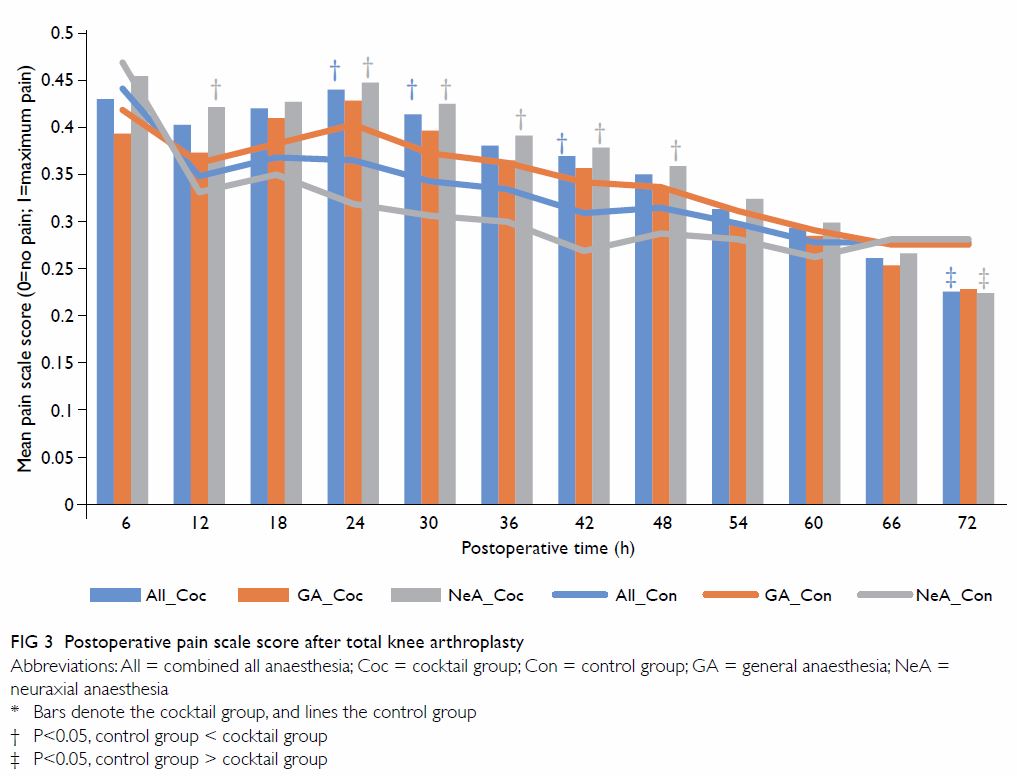
The mean cumulative PCAMC in both the cocktail and
control groups increased gradually until 72 h postoperatively (Fig
2). The difference between the two groups reached statistical
significance in the first 36 h. When effects of GA and NeA were reviewed
separately, significantly less PCA morphine was required in the cocktail
group than in the control group for the first 42 h (after GA) and 24 h
(after NeA).
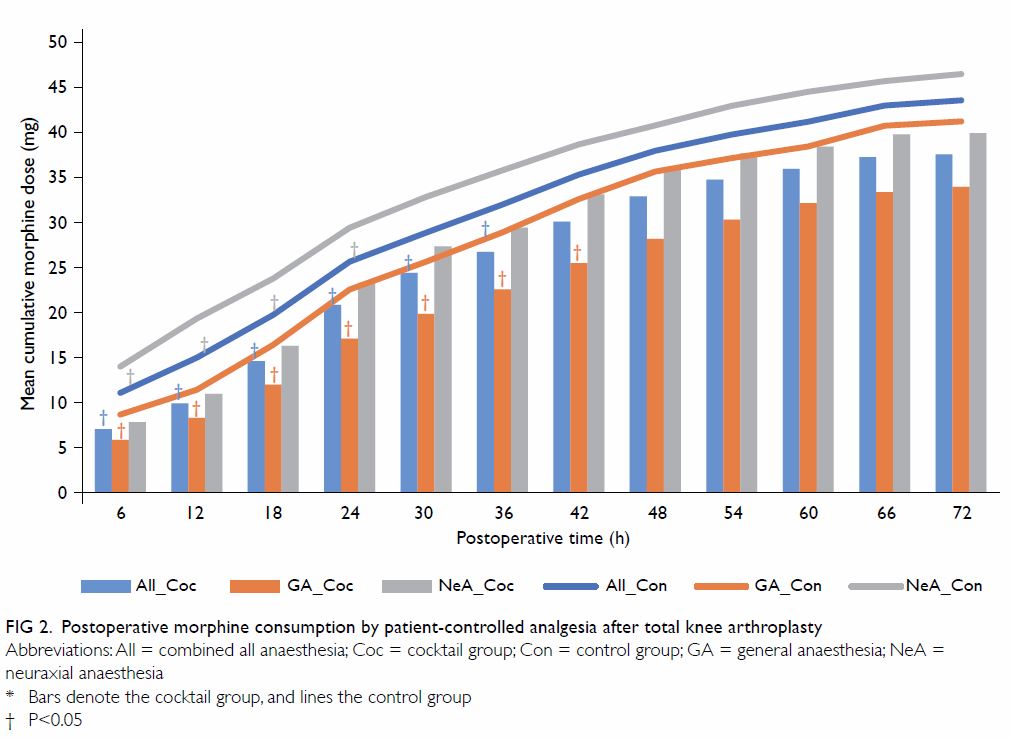
Figure 2. Postoperative morphine consumption by patient-controlled analgesia after total knee arthroplasty
Pain scale and complication
Figure 3 shows a decreasing severity of pain for
both groups in the initial 72 h after surgery. There was no statistically
significant difference between groups when TKA was performed under GA. In
patients who underwent TKA under NeA, patients in the control group had a
lower pain scale score by 0.1 at 12 h and from 24 to 48 h compared with
the cocktail group, although this was gradually reversed up to 72 h. There
were no adverse effects or complications as a result of IPMI.
Discussion
Severe pain following TKA may be related to bone or
soft tissue trauma or hyperperfusion following tourniquet release.6 Surgical difficulty in TKA has also been found to be
related to postoperative pain9 and
related to bone loss, severe deformity, flexion contracture, and poor
range, all of which contribute to a low preoperative knee score.
Nonetheless, in this study, the duration of tourniquet application was not
significantly correlated with morphine consumption; and preoperative knee
score was not correlated with PCAMC.
Pain management for TKA should start preoperatively
and intra-operatively. The preemptive use of analgesia has been shown to
prevent central sensitisation and improve postoperative pain control.10 11 12 Busch et al6
conducted a randomised trial of periarticular multimodal drug injection of
ropivacaine, ketorolac, epimorphine, and epinephrine in 64 TKA patients.
They reported significantly lower pain scores, increased patient
satisfaction scores, and decreased requirement for PCA in the first 24
hours after surgery. In another randomised trial of periarticular
injection of bupivacaine, fentanyl, and methylprednisolone in either side
of bilateral TKAs in 40 patients, pain scores were significantly lower,
and active knee flexion ranges were greater until the fourth week after
surgery.13 Maheshwari et al7 emphasised the importance of periarticular injection in
multimodal pain management following TKA at the Ranawat Orthopaedic
Center, United States, and PCA was no longer used because of the high
rates of systemic opioid side-effects.
The AHNH includes morphine in multimodal injections
because opioid receptors are present in peripheral inflamed tissue.14 15 They are
expressed within hours of surgical trauma and are thought to be
responsible for afferent sensory input to the central nervous system.16 17 The
injection also includes levobupivacaine, which is pharmacokinetically
similar to bupivacaine. It is a pure left-isomer and has less cardiac and
central nervous system toxicity.18
Corticosteroid was not added to the injection, although studies19 20 have
shown that methylprednisolone in periarticular injections in total joint
surgeries caused no delayed wound healing or wound infection. Mullaji et
al13 advocated cautious use of
steroid for fear of increasing the risk of surgical site infection in
patients who (1) had prior open surgical procedures, (2) were undergoing
revision TKA, (3) had poor nutritional status, (4) were immunocompromised,
(5) were rheumatoid, or (6) were diabetic. In the current study,
periarticular injection of a specific mixture decreased PCAMC for up to 42
hours. In 2013, Andersen et al21
advocated the addition of ketorolac during local infiltration analgesia.
They prepared the medication by mixing 150 mL of ropivacaine 2 mg/mL with
1 mL of ketorolac 30 mg/mL; to 100 mL of this mixture was added 0.5 mL of
epinephrine 1 mg/mL. The mixture containing epinephrine was injected into
the posterior capsule and around the prosthesis, and the 50 mL without
epinephrine was injected into the fascia and subcutis. An intra-articular
catheter was left in place to enable eight postoperative bolus injections
of analgesic without epinephrine. It was found that ketorolac successfully
reduced morphine consumption, pain intensity, and length of hospital stay.21 At the AHNH, 1 mL of ketorolac
30 mg/mL has been added to IPMI since July 2014 to provide local
anti-inflammatory action and enhance the analgesic effect.
Regional anaesthesia is the preferred method.7 8 The previous
randomised trials of multimodal drug injection in TKA involved a mixed
group of GA and regional anaesthesia,6
or excluded the samples of GA.13
Randomisation of anaesthesia in clinical trials is unethical because of
the obvious benefit of regional anaesthesia that avoids central nervous
system depression and prevents deep vein thrombosis following TKA.22 A retrospective study stratifying different types of
anaesthesia is therefore the preferred method, as in the current study.
The present study revealed that IPMI in TKA under NeA could significantly
decrease PCAMC for 24 hours.
A concordant finding could not be obtained between
the effect of IPMI on PCAMC and subjective pain scale. It is possible that
the greater use of PCA morphine in the control group in earlier years
explained the lower postoperative pain scores. Nonetheless, this could not
explain the absence of this phenomenon in the GA subgroup. Rather, it may
be explained by the secular change in patient expectations. To many
patients early on, TKA was well-known to be associated with a high level
of pain. They may have therefore used more PCA morphine. The level of
perceived pain was then less than expected with a consequent lower pain
score. With increasing popularity of TKA and knowledge of IPMI, patients
may have been overly optimistic about the outcome. The 4-point pain scale
used in the control group may have exaggerated this discrepancy when one
lower grade of pain severity was equal to a 0.25-drop in pain score
compared with a 0.1-drop in the 10-point pain scale.
Lamplot et al23
reported that the use of periarticular injection and multimodal analgesics
could lower pain scores, with fewer adverse effects, lower narcotic usage,
higher patient satisfaction, and faster recovery. At the AHNH, TKA
protocols for perioperative pain management, blood management, and
rehabilitation were altered following the establishment of the Joint
Replacement Centre in October 2015. For the pain management protocol, the
hospital now uses preemptive oral pregabalin, paracetamol, and etoricoxib
if not contra-indicated. The anaesthetist performs a single-injection
femoral nerve block or adductor canal block before anaesthesia. Surgeons
deliver IPMI. The postoperative cocktail consists of pregabalin,
paracetamol, etoricoxib, and tramadol. The new protocols have made a
significant contribution to the improvement in postoperative patient
recovery.24 25 Further studies will be conducted on the new
perioperative analgesic protocol to confirm its efficacy.
There were limitations to this retrospective study,
which compared two groups of patients with TKA performed during different
periods of time. First, possible secular changes to patient expectations
and pain assessment tools might have led to discordant outcomes when IPMI
was evaluated. Second, the pain scale did not focus separately on rest
pain and motion pain. Third, although the data were selectively verified
by the author, there might have been errors in data extraction and coding
of other data. Last but not least, because TKAs were performed by more
than one surgeon, it was difficult to standardise the intra-operative
soft-tissue tension and balancing and the injection technique of IPMI. If
the knee was made too tight or IPMI missed the quadriceps tendon, the
patient would experience greater postoperative pain.
In conclusion, IPMI effectively decreases
parenteral morphine consumption for up to 42 hours following TKA in
patients with OA of the knee.
Declaration
The author has disclosed no conflicts of interest.
No funding was received for this study.
References
1. Bonica JJ. Postoperative pain. In:
Bonica JJ, editor. The management of pain. 2nd ed. Philadelphia: Lea and
Febiger; 1990: 461-80.
2. Ranawat CS, Ranawat AS, Mehta A. Total
knee arthroplasty rehabilitation protocol: what makes the difference? J
Arthroplasty 2003;18(3 Suppl 1):27-30. Crossref
3. Singelyn FJ, Deyaert M, Joris D,
Pendeville E, Gouverneur JM. Effects of intravenous patient-controlled
analgesia with morphine, continuous epidural analgesia, and continuous
three-in-one block on postoperative pain and knee rehabilitation after
unilateral total knee arthroplasty. Anesth Analg 1998;87:88-92. Crossref
4. Shoji H, Solomonow M, Yoshino S,
D’Ambrosia R, Dabezies E. Factors affecting postoperative flexion in total
knee arthroplasty. Orthopedics 1990;13:643-9.
5. Lavernia C, Cardona D, Rossi MD, Lee D.
Multimodal pain management and arthrofibrosis. J Arthroplasty 2008;23(6
Suppl 1):74-9. Crossref
6. Busch CA, Shore BJ, Bhandari R, et al.
Efficacy of periarticular multimodal drug injection in total knee
arthroplasty. A randomized trial. J Bone Joint Surg Am 2006;88:959-63. Crossref
7. Maheshwari AV, Blum YC, Shekhar L,
Ranawat AS, Ranawat CS. Multimodal pain management after total hip and
knee arthroplasty at the Ranawat Orthopaedic Center. Clin Orthop Relat Res
2009;467:1418-23. Crossref
8. Chu CP, Yap JC, Chen PP, Hung HH.
Postoperative outcome in Chinese patients having primary total knee
arthroplasty under general anaesthesia/intravenous patient-controlled
analgesia compared to spinal-epidural anaesthesia/analgesia. Hong Kong Med
J 2006;12:442-7.
9. Lozano LM, Núñez M, Sastre S, Popescu D.
Total knee arthroplasty in the context of severe and morbid obesity in
adults. Open Obes J 2012;4:1-10. Crossref
10. Ringrose NH, Cross MJ. Femoral nerve
block in knee joint surgery. Am J Sports Med 1984;12:398-402. Crossref
11. Heard SO, Edwards WT, Ferrari D, et
al. Analgesic effect of intraarticular bupivacaine or morphine after
arthroscopic knee surgery: a randomized, prospective, double-blind study.
Anesth Analg 1992;74:822-6. Crossref
12. Woolf CJ, Chong MS. Preemptive
analgesia—treating postoperative pain by preventing the establishment of
central sensitization. Anesth Analg 1993;77:362-79. Crossref
13. Mullaji A, Kanna R, Shetty GM, Chavda
V, Singh DP. Efficacy of periarticular injection of bupivacaine, fentanyl,
and methylprednisolone in total knee arthroplasty: a prospective,
randomized trial. J Arthroplasty 2010;25:851-7. Crossref
14. Mauerhan DR, Campbell M, Miller JS,
Mokris JG, Gregory A, Kiebzak GM. Intra-articular morphine and/or
bupivacaine in the management of pain after total knee arthroplasty. J
Arthroplasty 1997;12:546-52. Crossref
15. Stein C. The control of pain in
peripheral tissue by opioids. N Engl J Med 1995;332:1685-90. Crossref
16. Stein C. Peripheral analgesic actions
of opioids. J Pain Symptom Manage 1991;6:119-24. Crossref
17. Stein C. Peripheral mechanisms of
opioid analgesia. Anesth Analg 1993;76:182-91. Crossref
18. Leone S, Di Cianni S, Casati A,
Fanelli G. Pharmacology, toxicology, and clinical use of new long acting
local anesthetics, ropivacaine and levobupivacaine. Acta Biomed
2008;79:92-105.
19. Parvataneni HK, Ranawat AS, Ranawat
CS. The use of local periarticular injections in the management of
postoperative pain after total hip and knee replacement: a multimodal
approach. Instr Course Lect 2007;56:125-31.
20. Parvataneni HK, Shah VP, Howard H,
Cole N, Ranawat AS, Ranawat CS. Controlling pain after total hip and knee
arthroplasty using a multimodal protocol with local periarticular
injections: a prospective randomized study. J Arthoplasty 2007;22(6 Suppl
2):33-8. Crossref
21. Andersen KV, Nikolajsen L, Haraldsted
V, Odgaard A, Soballe K. Local infiltration analgesia for total knee
arthroplasty: should ketorolac be added? Br J Anaesth 2013;111:242-8. Crossref
22. Sharrock NE, Haas SB, Hargett MJ,
Urquhart B, Insall JN, Scuderi G. Effects of epidural anesthesia on the
incidence of deep-vein thrombosis after total knee arthroplasty. J Bone
Joint Surg Am 1991;73:502-6. Crossref
23. Lamplot JD, Wagner ER, Manning DW.
Multimodal pain management in total knee arthroplasty: a prospective
randomized controlled trial. J Arthroplasty 2014;29:329-34. Crossref
24. Ng FY, Ng JK, Chiu KY, Yan CH, Chan
CW. Multimodal periarticular injection vs continuous femoral nerve block
after total knee arthroplasty: a prospective, crossover, randomized
clinical trial. J Arthroplasty 2012;27:1234-8. Crossref
25. Wu JW, Wong YC. Elective unilateral
total knee replacement using continuous femoral nerve blockade versus
conventional patient-controlled analgesia: perioperative patient
management based on a multidisciplinary pathway. Hong Kong Med J
2014;20:45-51.