Hong
Kong Med J 2018 Feb;24(1):48–55 | Epub 5 Jan 2018
DOI: 10.12809/hkmj176984
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Injuries and envenomation by exotic pets in Hong Kong
Vember CH Ng, FHKCEM, FHKAM (Emergency Medicine)1;
Albert CH Lit, FRCSEd, FHKAM (Emergency Medicine)2; OF Wong,
FHKAM (Anaesthesiology), FHKAM (Emergency Medicine)2; ML Tse,
FHKCEM, FHKAM (Emergency Medicine)1; HT Fung, FRCSEd, FHKAM
(Emergency Medicine)3
1 Hong Kong Poison Information Centre,
United Christian Hospital, Kwun Tong, Hong Kong
2 Accident and Emergency Department,
North Lantau Hospital, Tung Chung, Lantau, Hong Kong
3 Accident and Emergency Department,
Tuen Mun Hospital, Tuen Mun, Hong Kong
Corresponding author: Dr OF Wong (oifungwong@yahoo.com.hk)
Abstract
Introduction: Exotic pets are
increasingly popular in Hong Kong and include fish, amphibians,
reptiles, and arthropods. Some of these exotic animals are venomous and
may cause injuries to and envenomation of their owners. The clinical
experience of emergency physicians in the management of injuries and
envenomation by these exotic animals is limited. We reviewed the
clinical features and outcomes of injuries and envenomation by exotic
pets recorded by the Hong Kong Poison Information Centre.
Methods: We retrospectively
retrieved and reviewed cases of injuries and envenomation by exotic pets
recorded by the Hong Kong Poison Information Centre from 1 July 2008 to
31 March 2017.
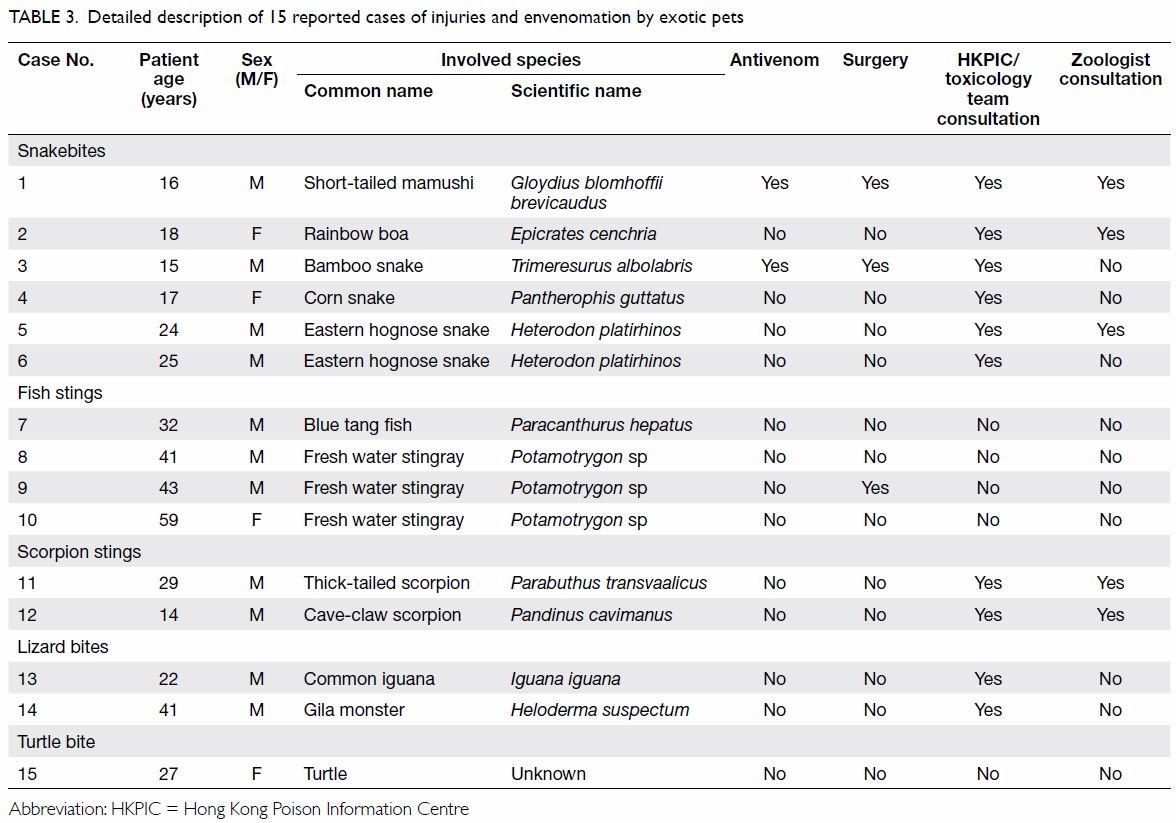
Results: There were 15 reported
cases of injuries and envenomation by exotic pets during the study
period, including snakebite (n=6), fish sting (n=4), scorpion sting
(n=2), lizard bite (n=2), and turtle bite (n=1). There were two cases of
major effects from the envenomation, seven cases with moderate effects,
and six cases with mild effects. All major effects were related to
venomous snakebites. There were no mortalities.
Conclusion: All human injuries
from exotic pets arose from reptiles, scorpions, and fish. All cases of
major envenomation were inflicted by snakes.
New knowledge added by this study
- This is the first case series of injuries and envenomation by exotic pets in Hong Kong.
- Reptiles, scorpions, and fish that are kept as exotic pets can potentially cause injuries to and envenomation of their owners.
- All cases of major envenomation were inflicted by snakes. Envenomation by a highly venomous exotic snake was also encountered.
- A variety of exotic animals, including venomous species, are kept as pets in Hong Kong. Emergency physicians in Hong Kong, however, have limited knowledge about the management of injuries caused by these exotic animals.
- The Hong Kong Poison Information Centre provides an expert consultation service for the management of injuries and envenomation by such exotic animals.
Introduction
A variety of exotic animals are kept as ‘pets’
including fish, amphibians, reptiles, and arthropods. The keeping of
exotic, and sometimes venomous pets, is becoming increasingly common
worldwide. Some of these exotic pets are capable of causing injury to or
even life-threatening envenomation of their owners.1
Reptiles are the most popular exotic pets
worldwide. It has been estimated that 1.5 to 2.0 million households in the
United States (US) own one or more pet reptiles. Snakes account for
approximately 11% of the imported reptiles in the US, and up to 9% of
these are venomous.2 Envenomation
by exotic pets, particularly snakes, is an increasing cause for concern in
both the US and Europe.3 In a study
of exotic snake envenomation in the US, data from the National Poison Data
System database revealed 258 cases of exotic snakebites involving at least
61 unique exotic venomous species between 2005 and 2011. Among these, 40%
of bites occurred in a private residence.4
Another study of bites and stings by exotic pets in Europe reported 404
cases in four poison centres in Germany and France from 1996 to 2006.
Exotic snakebites from rattlesnakes, cobras, mambas, and other venomous
snakes were the cause of approximately 40% of envenomations.5 Another survey conducted in the United Kingdom reviewed
the data from the National Health Service Health Episode Statistics from
2004 to 2010. A total of 709 hospital admissions associated with injuries
from exotic pets were reported and approximately 300 hospital admissions
were related to contact with scorpions, venomous snakes, and lizards.6 Nonetheless, no such epidemiological study has been
conducted in Hong Kong. According to the thematic household survey report
in 2006, 286 300 households in Hong Kong kept pets at home, of which 5%
were pets other than dogs, cats, turtles, tortoises, birds, hamsters, and
rabbits.7 The number of imported
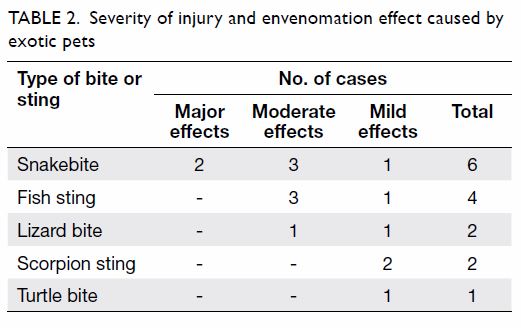
pet reptiles into Hong Kong has increased rapidly in recent years. In
2016, the Agriculture, Fisheries and Conservation Department (AFCD)
recorded that almost 1 000 000 pet reptiles were imported into Hong Kong (Table 1).
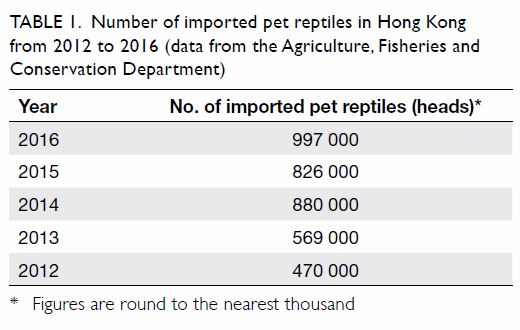
Table 1. Number of imported pet reptiles in Hong Kong from 2012 to 2016 (data from the Agriculture, Fisheries and Conservation Department)
The knowledge of local emergency physicians about
the management of injuries by these exotic animals is limited. Since 2005,
the Hong Kong Poison Information Centre (HKPIC) has provided a 24-hour
telephone consultation service (tel: 2635 1111) for health care
professionals in Hong Kong, offering poison information and clinical
management advice. The objectives of this study were to use HKPIC records
to describe the variety of reported exotic species and the clinical
features and outcomes of injuries and envenomation caused by exotic pets.
Methods
This was a case series based on the database of the
HKPIC. It included cases encountered by clinical frontline staff and
surveillance data from routine reporting of poisoning cases by all
accident and emergency departments (AEDs) under the Hospital Authority
(HA). Cases of injuries and envenomation by exotic pets recorded by the
HKPIC from 1 July 2008 to 31 March 2017 were retrospectively retrieved.
Demographic data of the patients—including the involved species, clinical
presentations, and outcomes—were reviewed from the patient electronic
Health Record. This study was done in accordance with the principles
outlined in the Declaration of Helsinki.
The severity of injuries and the effects of
envenomation were defined as major (life-threatening or resulting in
significant residual disability or disfigurement), moderate (pronounced,
prolonged, or systemic signs and symptoms), or mild (minimal and rapidly
resolving signs and symptoms).
Results
During the study period, 15 cases of injuries and
envenomation by exotic pets were reported to the HKPIC. Among the 15
patients, nine consulted the HKPIC for management advice and one was
managed by the toxicology team of the AED. Local zoologists were consulted
in five cases for species identification and opinion about the venomous
nature of the species. All bites and stings were unintentional and
occurred in a private household. The mean age of the exotic pet owners was
28.2 (range, 14-59) years and the majority (73%) were male. There were six
cases of snakebite, four cases of fish sting, two cases of scorpion sting,
two cases of lizard bite, and one case of turtle bite. The severity of
injury and envenomation effect are summarised in Table 2.
All major effects occurred in patients with
snakebite. A 16-year-old boy was bitten by a short-tailed mamushi (Gloydius
blomhoffii brevicaudus; Fig 1a) on his left middle finger. The short-tailed
mamushi is not native to Hong Kong but was being kept as a pet. The
patient had a history of snakebite by a bamboo snake (Trimeresurus
albolabris) that required antivenom treatment, sustained while
attempting to catch the snake in the suburbs. Following the bite by the
short-tailed mamushi, the patient developed severe local envenomation over
his left hand and required admission to the intensive care unit for close
observation of the rapidly progressing local envenomation. No systemic
envenomation was observed. A local zoologist was consulted for snake
identification. A total of three vials of antivenom for Agkistrodon
halys were administered as treatment but ischaemia due to
compartment syndrome developed in the left hand. Debridement and
fasciotomy were eventually performed. The patient had a residual flexion
contraction deformity of his left middle finger 2 months later. He
recovered with full movement of the left middle finger 6 months after the
injury. Another boy, aged 15 years, was bitten by a bamboo snake on his
left thumb. The snake had been caught by the patient in the suburbs and
kept as a pet. He developed severe local envenomation and was given three
vials of antivenom for Agkistrodon halys and three vials of
antivenom for green pit viper. The patient developed tenosynovitis of his
left thumb and required emergency surgery for debridement. Another four
patients were bitten by ‘nonvenomous’ snakes including a rainbow boa (Epicrates
cenchria; Fig 1b), corn snake (Pantherophis guttatus),
and eastern hognose snake (Heterodon platirhinos; Fig
1c). All snakes were kept as pets. An 18-year-old girl was
accidentally bitten by a rainbow boa on her left hand but had no signs of
local or systemic envenomation after the injury. Another patient developed
a wound infection after being bitten by a corn snake 2 weeks previously (Fig 1d). She recovered after a course of antibiotic
therapy. Two young men were bitten by hognose snakes. One developed local
envenomation with progressive swelling over the injured hand (Fig
1e). The local envenomation resolved with conservative management.
The HKPIC was consulted in all cases, of which three required consultation
with a zoologist.
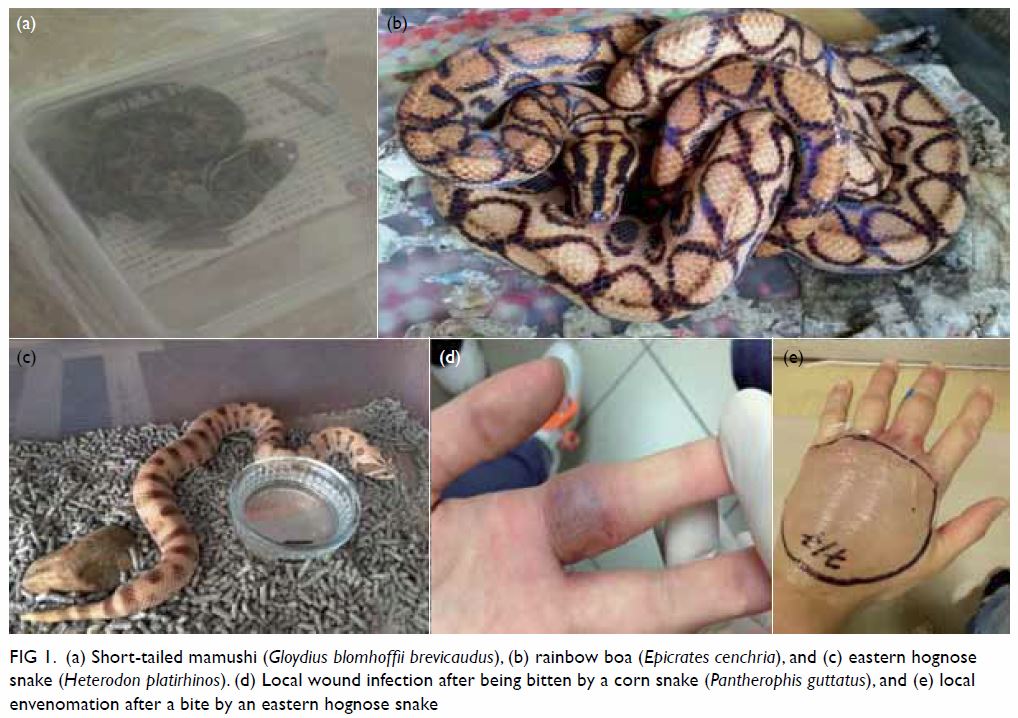
Figure 1. (a) Short-tailed mamushi (Gloydius blomhoffii brevicaudus), (b) rainbow boa (Epicrates cenchria), and (c) eastern hognose snake (Heterodon platirhinos). (d) Local wound infection after being bitten by a corn snake (Pantherophis guttatus), and (e) local envenomation after a bite by an eastern hognose snake
Injuries from reptiles other than snakes were also
recorded. There were two cases of lizard bite. In one case, a 22-year-old
man was bitten by a common iguana (Iguana iguana) on his left
wrist. In the other case, a 41-year-old man presented to the AED
approximately 2 hours after being bitten on his right hand by a Gila
monster (Fig 2a). He developed intense pain and local
swelling over the site of injury. The pain lasted for about 12 hours and
then gradually improved. His haemodynamic state remained stable and no
airway oedema or neurological symptoms were observed during his stay in
the emergency medicine ward. He was eventually discharged. A young woman
attended the AED because of a turtle bite over her left face with
consequent minor physical injury.

Figure 2. (a) Gila monster (Heloderma suspectum) and (b) freshwater stingray (Potamotrygon species). (c) Thick-tailed scorpion (Parabuthus transvaalicus) and (d) cave-claw scorpion (Pandinus cavimanus). (e) Wound infection after cave-claw scorpion sting
Stings by aquarium fish were the second most common
injuries by exotic pets. Four cases were recorded, including one sting by
a blue tang fish and three by freshwater stingrays (Fig 2b). All patients developed severe pain over the
site of injury that responded to immersion in hot water. One of the
patients with a freshwater stingray sting developed a wound infection that
required emergency surgery for wound exploration and irrigation.
Two male patients were stung by their pet
scorpions: a thick-tailed scorpion (Parabuthus transvaalicus; Fig
2c) and a cave-claw scorpion (Pandinus cavimanus; Fig
2d). No systemic envenomation was observed. The patient with the
cave-claw scorpion sting developed a local wound infection (Fig
2e) that recovered after a course of antibiotics.
The characteristics and management of the 15 cases
are summarised in Table 3.
Discussion
Injuries by a variety of exotic pets were
encountered in this study. More than half of the injuries (9/15) were
inflicted by reptiles. Reptiles are becoming increasingly popular to keep
as pets in Hong Kong. According to the records of the AFCD over the past 5
years, the top 10 most common reptile species imported to Hong Kong are
the European pond turtle (Emys orbicularis), razor-backed musk
turtle (Sternotherus carinatus), common snapping turtle (Chelydra
serpentina), red-bellied cooter (Pseudemys nelsoni), yellow-spotted Amazon
River turtle (Podocnemis unifilis), Hermann’s tortoise (Testudo
hermanni), African spurred tortoise (Geochelone sulcata),
leopard tortoise (Stigmochelys pardalis), common iguana (Iguana
iguana), and ball python (Python regius). Commonly imported
pet snakes include the ball python (Python regius), king snake (Lampropeltis
getula), corn snake (Pantherophis guttatus), rat snake (Elaphe
obsoleta), milk snake (Lampropeltis triangulum), and western
hognose snake (Heterodon nasicus). With the exception of the
hognose snake, which is a mildly venomous species, they are all
nonvenomous. Nonetheless, a much wider variety of species, including
venomous reptiles, may be sold on the black market. Bites may occur during
the care and handling of these exotic animals.3
Envenomation by exotic venomous species is an uncommon but often serious
medical emergency.
The keeping of venomous snakes is common in the US.4 Amateur collectors are at risk of
bites and envenomation and fatalities have been reported.8 Although envenomation from exotic snakes is rarely
encountered in Hong Kong, it poses a great challenge to emergency
physicians owing to their lack of experience and limited supplies of
antivenom, as illustrated by our case of bite by a short-tailed mamushi.
Currently, the HA stocks principally snake antivenom for local venomous
species (Table 4). Bites by nonvenomous pet snakes may also
result in local envenomation and complications; for instance, although the
hognose snake is known as a nonvenomous species, one patient developed
local envenomation after being bitten. Another patient developed a wound
infection after being bitten by a corn snake.
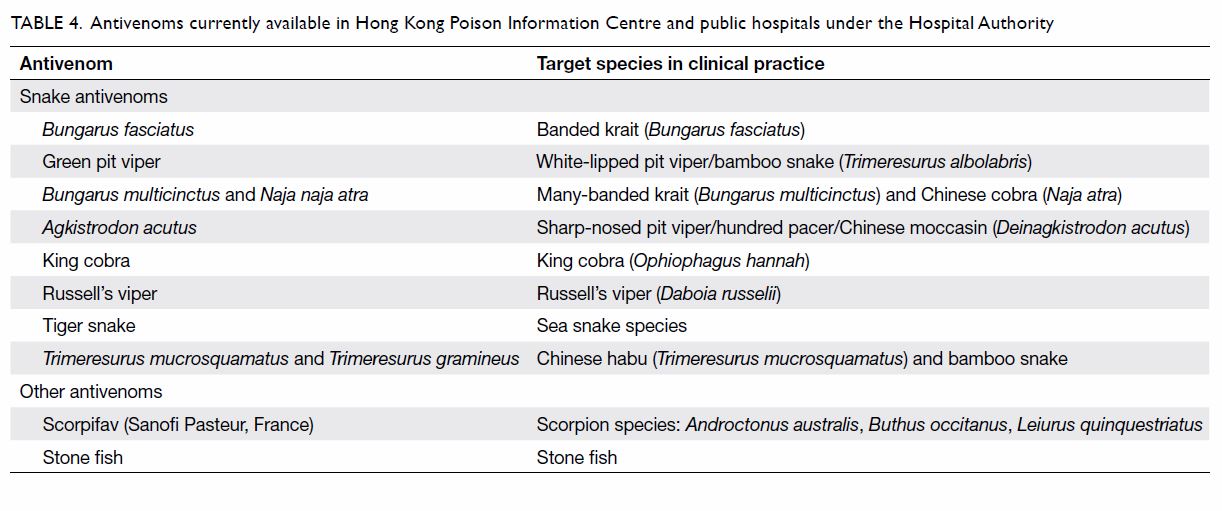
Table 4. Antivenoms currently available in the Hong Kong Poison Information Centre and public hospitals under the Hospital Authority
As well as snakes, lizards are popular as pets.
Bites by large species such as the common green iguana (Iguana iguana)
can result in serious injury.9
Envenomation from lizard bites is rare in Hong Kong. Two lizards are well
known to be venomous: the Gila monster (Heloderma suspectum)10 and the Mexican beaded lizard (Heloderma horridum).11 12
Both have venom-secreting glands and bites. The Gila monster is native to
the southwestern US extending into Mexico, whereas the beaded lizard is
native only to Mexico. The Gila monster is listed in the Convention on
International Trade in Endangered Species of Wild Fauna and Flora (CITES)
as a protected species.13
Captive-bred Gila monsters are traded in international pet markets. Venom
of the Gila monster consists of a variety of proteins including gilatoxin,
a kallikrein-like protease that can hydrolyse kininogen and produce
bradykinin.11 14 The common envenomation effects are intense pain at
the injured site, oedema, paraesthesia, weakness, dizziness, and nausea.
Hypotension occurs in severe envenomation.15
The intense pain, oedema, and hypotension are likely due to the
bradykinin-mediated effects. Airway oedema has been reported regardless of
the site of bite and may occur up to 12 hours after the bite.14 Nevertheless, severe envenomation from the Gila
monster occurs in only a minority of patients. In a retrospective study of
all cases of Gila monster bite reported to the two Arizona poison control
centres from 2000 to 2011, 105 cases of human exposure to Gila monsters
were recorded and 70 cases were referred to health care facilities for
medical treatment. Eleven cases required admission to hospital and five
required care in an intensive care unit. Six patients developed airway
oedema and three required emergent airway management including one
cricothyrotomy.14 Treatment of
Gila monster bites is mainly supportive. Intravenous crystalloid infusion
and vasopressors may be required for treatment of hypotension in severe
envenomation. Radiographic assessment is needed to look for retained teeth
and subcutaneous air due to the chewing-like action during the bites.16 No antivenom to Gila monster is commercially
available.17 Observation for at
least 12 hours after the bite for delayed-onset airway oedema is
recommended.14
Among all the reptiles, tortoises and turtles are
the most popular in pet markets. All species of tortoises and turtles are
nonvenomous although some, such as the alligator snapping turtle (Macrochelys
temminckii) and the common snapping turtle (Chelydra serpentina),
are aggressive and can grow to a very large size. Bites by these large
species can result in severe limb injuries.18
Stings by aquarium fish contributed to the second
largest group of injuries in our case series. The most commonly
encountered aquarium fish was freshwater stingray. Freshwater stingrays (Potamotrygon
species) are native to South America. They are regarded as dangerous by
the native people of the Amazon and frequent sting during fishing season.19 Freshwater stingrays are not
aggressive by nature; stings frequently occur when people step on them or
handle them improperly. Different species of freshwater stingrays have
different colour patterns on their body. They are popular aquarium fish as
they are easy to keep although stings may result in severe envenomation.20 The most common feature of
envenomation from freshwater stingrays is intense local pain. Systemic
manifestations are rare. Skin necrosis is frequently observed in victims
wounded by large freshwater stingrays in the wild.21 In addition, skin necrosis is more commonly observed
in victims injured by freshwater stingrays than marine stingrays. A study
of tissue extracts from the stingers of freshwater and marine stingrays
showed that both tissue extracts had gelatinolytic, caseinolytic, and
fibrinogenolytic activity but hyaluronidase activity was detected only in
the extracts from freshwater stingrays.22
In our case series, no patient injured by a freshwater stingray developed
skin necrosis. The risk of developing skin necrosis is likely related to
the venom load. Larger stingrays possess a much larger venom load in their
stingers. Small freshwater stingrays are commonly kept in an aquarium and
skin necrosis as a result of their sting is uncommon. Hot water immersion
is effective in controlling acute pain but does not prevent skin necrosis.21 Wounds caused by freshwater
stingray stings such as the Aeromonas species can be complicated
by severe secondary infection with virulent bacteria.23 Prophylactic antibiotic is often required.
Apart from freshwater stingrays, the stinging
catfish (Heteropneustes fossilis) is another commonly reported
freshwater aquarium fish that can cause injuries and envenomation. It
possesses venom in the sting that is located in front of the soft-rayed
portion of the pectoral and dorsal fins. Apart from intense local pain,
systemic envenomation including weakness and hypotension can result from a
sting.24 25 There was no case reported to the HKPIC of injury by
this venomous catfish during the study period. Coral reef fish are also
popular pets in Hong Kong. Some coral reef fish, such as the lionfish (Pterois
volitans), are venomous.26
Nonetheless, injuries by aquarium coral reef fish were rarely encountered
in the AED of Hong Kong.
Exotic pet owners also enjoy keeping arthropods
such as scorpions and spiders. There are approximately 2000 species of
scorpion in the world but only a few (30 to 40) are highly venomous and
able to cause severe envenomation in humans.27
Scorpion envenomation is reported throughout the world, mainly in
subtropical and tropical regions.28
The majority of scorpion stings cause mild or no envenomation. Species
that cause serious medical problems mainly belong to the Buthidae family.
The genera of the Buthidae family include Centruroides, Tityus,
Leiurus, Androctonus, Buthus and Parabuthus.29 Scorpions have a special venom
apparatus, the telson, that produces venom. Scorpion venom comprises
numerous toxins including several neurotoxins. Unlike snake venom,
scorpion venom generally lacks enzyme activity. The main molecular targets
of scorpion neurotoxins are the voltage-gated sodium channels and the
voltage-gated potassium channels. Scorpion α-toxin, one of the most
medically important neurotoxins in the scorpion venom, acts on the
voltage-gated sodium channels. Once the toxin binds to voltage-gated
sodium channels, it inhibits inactivation of the channel with consequent
prolonged depolarisation and, hence, neuronal excitation. The autonomic
centres, both sympathetic and parasympathetic, are stimulated. In most
situations of scorpion envenomation, the sympathetic nerves are
predominantly affected. Scorpion envenomation is characterised by
relatively similar neurotoxic excitation syndromes, irrespective of the
species. Parasympathetic effects tend to occur early and then sympathetic
effects persist due to the release of catecholamines that are responsible
for the severe envenomation. Parasympathetic (cholinergic) effects include
hypersalivation, diaphoresis, lacrimation, miosis, diarrhoea, vomiting,
bradycardia, hypotension, increased respiratory secretion, and priapism.
Sympathetic (adrenergic) effects are manifested as tachycardia,
hypertension, mydriasis, hyperthermia, hyperglycaemia, and agitation.
Fatal effects of scorpion envenomation are largely due to cardiovascular
effects. Various cardiac conduction abnormalities have been reported in
patients with scorpion envenomation as well as catecholamine-induced
cardiomyopathy, pulmonary oedema, and cardiogenic shock. Other
manifestations of systemic envenomation include vomiting, abdominal pain,
abnormal oculomotor movements, muscle fasciculation, and spasms of the
face and limbs.29 Pancreatitis is
also a well-reported complication of envenomation by certain species, such
as Leiurus quinquestriatus.30
Nonetheless, severe local envenomation is generally uncommon. Differences
in the clinical manifestations of systemic envenomation exist in some
species. Delayed localised necrosis has been reported in patients stung by
an Iranian scorpion (Hemiscorpius lepturus).31 Patients with envenomation from the thick-tailed
scorpion (Parabuthus transvaalicus) in Zimbabwe have been reported
to develop predominant symptoms from parasympathetic nerve system
stimulation, including profuse sialorrhoea, sweating, and urinary
retention, in the absence of sympathetic stimulation.32
Scorpion stings and envenomation are uncommon in
Hong Kong. Most of the locally reported cases of scorpion sting occurred
while patients were handling langsat, a type of tropical fruit from
South-East Asia. The Chinese stropped bark scorpion (Lychas mucronatus)
hides in the fruit and is subsequently imported into Hong Kong.33 Scorpions are also sold as fish food in aquarium
shops in Hong Kong. People use scorpions to feed arowana, which are
popular aquarium fish. Importation of endangered scorpion species
(CITES-listed species) for commercial purposes is regulated by the
Protection of Endangered Species of Animals and Plants Ordinance Cap. 586
in Hong Kong.34 According to the
data from the AFCD for importation of CITES-listed scorpions, more than
1000 heads of emperor scorpion (Pandinus imperator) have been
imported as pets to Hong Kong each year for the last 4 years. The emperor
scorpion is a nonvenomous species and is native to the rainforests and
savannas of West Africa. Most scorpions in the pet trade, such as the
forest scorpion (Heterometrus species), have no potential for
dangerous envenomation. Nonetheless venomous species may also be kept by
hobbyists and severe envenomation may occur after stings.
Management of scorpion stings includes local wound
care and supportive care for systemic envenomation. Expert opinion should
be sought from a zoologist for species identification and to determine the
venomous nature of the species. Patients with severe systemic envenomation
may require antivenom therapy. Specific antivenom (Scorpifav; Sanofi
Pasteur, France) for Androctonus australis, Buthus occitanus,
and Leiurus quinquestriatus is currently available in the HKPIC.
Spiders, such as tarantulas, are popular exotic
pets and are common in the pet trade in Hong Kong. Nonetheless,
inexperienced owners may be unaware of the potential risk of ocular injury
from the barbed urticating hairs on the abdomen of the tarantulas. Eye
injuries occur when the barbed hairs come into contact with the eyes,
either directly from the tarantula’s ejection or when the owners rub their
eyes after handling the spider.35
Embedment of the hairs in the cornea can result in severe complications,
including ophthalmia nodosa, iritis, and even permanent visual impairment.36 37
Conclusion
The diversity of pets is changing and keeping
exotic animals is increasingly popular. Injuries from these exotic pets
are expected to increase and envenomation may result from stings or bites
from some species. In our case series, reptiles, scorpions, and fish were
responsible for human injuries, and all cases of major envenomation were
inflicted by snakes. Emergency physicians need to be aware of the
appropriate management of injuries and envenomation by these exotic
animals. The HKPIC plays an important role in the provision of expert
advice about management of these special toxicological cases.
Acknowledgement
The authors would like to thank AFCD for providing
the data of imported reptiles, scorpions, and spiders.
Declaration
All authors have disclosed no conflicts of
interest.
References
1. Bey TA, Boyer LV, Walter FG, McNally J,
Desai H. Exotic snakebite: envenomation by an African puff adder (Bitis
arietans). J Emerg Med 1997;15:827-31. Crossref
2. McNally J, Boesen K, Boyer L.
Toxicologic information resources for reptile envenomations. Vet Clin
North Am Exot Anim Pract 2008;11:389-401. Crossref
3. de Haro L, Pommier P. Envenomation: a
real risk of keeping exotic house pets. Vet Hum Toxicol 2003;45:214-6.
4. Warrick BJ, Boyer LV, Seifert SA.
Non-native (exotic) snake envenomations in the U.S., 2005-2011. Toxins
(Basel) 2014;6:2899-911. Crossref
5. Schaper A, Desel H, Ebbecke M, et al.
Bites and stings by exotic pets in Europe: an 11 year analysis of 404
cases from Northeastern Germany and Southeastern France. Clin Toxicol
(Phila) 2009;47:39-43. Crossref
6. Warwick C, Steedman C. Injuries,
envenomations and stings from exotic pets. J R Soc Med 2012;105:296-9. Crossref
7. Thematic household survey report 2006.
Census and Statistics Department, HKSAR Government. Available from:
http://www.statistics.gov.hk/pub/ B11302262006XXXXB0100.pdf. Accessed 1
Jun 2017.
8. Marsh N, DeRoos F, Touger M. Gaboon
viper (Bitis gabonica) envenomation resulting from captive
specimens—a review of five cases. Clin Toxicol (Phila) 2007;45:60-4. Crossref
9. Heffelfinger RN, Loftus P, Cabrera C,
Pribitkin EA. Lizard bites of the head and neck. J Emerg Med
2012;43:627-9. Crossref
10. Hooker KR, Caravati EM, Hartsell SC.
Gila monster envenomation. Ann Emerg Med 1994;24:731-5. Crossref
11. Cantrell FL. Envenomation by the
Mexican beaded lizard: a case report. J Toxicol Clin Toxicol
2003;41:241-4.Crossref
12. Ariano-Sánchez D. Envenomation by a
wild Guatemalan beaded lizard Heloderma horridum charlesbogerti.
Clin Toxicol (Phila) 2008;46:897-9. Crossref
13. Wijnstekers W. The Convention on
International Trade in Endangered Species of Wild Fauna and Flora
(CITES)—35 years of global efforts to ensure that international trade in
wild animals and plants is legal and sustainable. Forensic Sci Rev
2011;23:1-8.
14. French R, Brooks D, Ruha AM, et al.
Gila monster (Heloderma suspectum) envenomation: descriptive
analysis of calls to United States Poison Centers with focus on Arizona
cases. Clin Toxicol (Phila) 2015;53:60-70. Crossref
15. Piacentine J, Curry SC, Ryan PJ.
Life-threatening anaphylaxis following gila monster bite. Ann Emerg Med
1986;15:959-61. Crossref
16. French RN, Ash J, Brooks DE. Gila
monster bite. Clin Toxicol (Phila) 2012;50:151-2. Crossref
17. Miller MF. Gila monster envenomation.
Ann Emerg Med 1995;25:720. Crossref
18. Johnson RD, Nielsen CL. Traumatic
amputation of finger from an alligator snapping turtle bite. Wilderness
Environ Med 2016;27:277-81. Crossref
19. Junior VH, Cardoso JL, Neto DG.
Injuries by marine and freshwater stingrays: history, clinical aspects of
the envenomations and current status of a neglected problem in Brazil. J
Venom Anim Toxins Incl Trop Dis 2013;19:16. Crossref
20. Brisset IB, Schaper A, Pommier P, de
Haro L. Envenomation by Amazonian freshwater stingray Potamotrygon
motoro: 2 cases reported in Europe. Toxicon 2006;47:32-4. Crossref
21. Haddad V Jr, Neto DG, de Paula Neto
JB, de Luna Marques FP, Barbaro KC. Freshwater stingrays: study of
epidemiologic, clinic and therapeutic aspects based on 84 envenomings in
humans and some enzymatic activities of the venom. Toxicon 2004;43:287-94.
Crossref
22. Barbaro KC, Lira MS, Malta MB, et al.
Comparative study on extracts from the tissue covering the stingers of
freshwater (Potamotrygon falkneri) and marine (Dasyatis guttata)
stingrays. Toxicon 2007;50:676-87. Crossref
23. Polack FP, Coluccio M, Ruttimann R,
Gaivironsky RA, Polack NR. Infected stingray injury. Pediatr Infect Dis J
1998;17:349,360.
24. Dorooshi G. Catfish stings: a report
of two cases. J Res Med Sci 2012;17:578-81.
25. Satora L, Kuciel M, Gawlikowski T.
Catfish stings and the venom apparatus of the African catfish Clarias
gariepinus (Burchell, 1822), and stinging catfish Heteropneustes
fossilis (Bloch, 1794). Ann Agric Environ Med 2008;15:163-6.
26. Chan HY, Chan YC, Tse ML, Lau FL.
Venomous fish sting cases reported to Hong Kong Poison Information Centre:
a three-year retrospective study on epidemiology and management. Hong Kong
J Emerg Med 2010;17:40-4. Crossref
27. Santos MS, Silva CG, Neto BS, et al.
Clinical and epidemiological aspects of scorpionism in the world: a
systematic review. Wilderness Environ Med 2016;27:504-18. Crossref
28. Chippaux JP, Goyffon M. Epidemiology
of scorpionism: a global appraisal. Acta Trop 2008;107:71-9. Crossref
29. Kounis NG, Soufras GD. Scorpion
envenomation. N Engl J Med 2014;371:1558-9.
30. Sofer S, Shalev H, Weizman Z, Shahak
E, Gueron M. Acute pancreatitis in children following envenomation by the
yellow scorpion Leiurus quinquestriatus. Toxicon 1991;29:125-8.Crossref
31. Pipelzadeh MH, Jalali A, Taraz M,
Pourabbas R, Zaremirakabadi A. An epidemiological and a clinical study on
scorpionism by the Iranian scorpion Hemiscorpius lepturus. Toxicon
2007;50:984-92.Crossref
32. Bergman NJ. Scorpion sting in
Zimbabwe. S Afr Med J 1997;87:163-7.
33. Centre for Food Safety, Hong Kong SAR
Government. Scorpion stings and langsat. Food Safety Focus (16th Issue,
Nov 2007). Available from: http://www.cfs.gov.hk/english/
multimedia/multimedia_pub/multimedia_pub_fsf_16_04. html. Accessed 1 Jun
2017.
34. Agriculture, Fisheries and
Conservation Department, Hong Kong SAR Government. Protection of
Endangered Species of Animals and Plants Ordinance. Available from:
http://www.afcd.gov.hk/english/conservation/con_end/
con_end_reg/con_end_reg_ord/con_end_reg_ord.html. Accessed 1 Jun 2017.
35. Waggoner TL, Nishimoto JH, Eng J. Eye
injury from tarantula. J Am Optom Assoc 1997;68:188-90.
36. Belyea DA, Tuman DC, Ward TP, Babonis
TR. The red eye revisited: ophthalmia nodosa due to tarantula hairs. South
Med J 1998;91:565-7. Crossref
37. Blaikie AJ, Ellis J, Sanders R,
MacEwen CJ. Eye disease associated with handling pet tarantulas: three
case reports. BMJ 1997;314:1524-5. Crossref