Hong
Kong Med J 2017 Dec;23(6):562–9 | Epub 13 Oct 2017
DOI: 10.12809/hkmj166102
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE CME
Patient opinion of lower urinary tract symptoms and
their treatment: a cross-sectional survey in Hong Kong public urology
clinics
LY Ho, FRCSEd (Urol), FHKAM (Surgery)1;
CK Chan, FRCSEd (Urol), FHKAM (Surgery)2; Peggy SK Chu, FRCS
(Edin), FHKAM (Surgery)3
1 Division of Urology, Department
of Surgery, Queen Elizabeth Hospital, Jordan, Hong Kong
2 Division of Urology, Department
of Surgery, Prince of Wales Hospital, The Chinese University of Hong Kong,
Shatin, Hong Kong
3 Division of Urology, Department
of Surgery, Tuen Mun Hospital, Tuen Mun, Hong Kong
Corresponding author: Dr LY Ho (holapyin@yahoo.com.hk)
Abstract
Introduction: Lower urinary
tract symptoms collectively represent a common condition among ageing
men. There are, however, limited data on the frequency of individual
symptoms in patients who seek specialist care. We conducted a
multinational survey in South-East Asia to evaluate patients’
self-reported prevalence, bother, treatment, and treatment satisfaction
of four lower urinary tract symptoms namely, urgency, nocturia, slow
stream, and post-micturition dribble. This report presents the analysis
of the Hong Kong subpopulation.
Methods: This cross-sectional
survey involved adult men aged over 18 years who attended a urology
out-patient clinic because of lower urinary tract symptoms. A structured
questionnaire, translated and validated in the local languages, was
self-administered by patients.
Results: Of 1436 respondents
surveyed in the region, 225 were from Hong Kong of whom most were aged
56 to 75 years, retired, and had no history of any previous prostate
surgery. Overall, the self-reported prevalence of nocturia of at least
one void per night was 93% (95% confidence interval, 90%-97%), slow
stream 76% (71%-82%), post-micturition dribble 70% (64%-76%), and
urgency 50% (43%-56%). Symptoms for which most respondents reported
“some” or “a lot” of bother included: nocturia, defined as at least two
voids per night (77%), and urgency and post-micturition dribble (73%).
Only 39% to 54% of patients had previously received treatment but were
not entirely satisfied with it. An understanding of their condition
remained suboptimal.
Conclusions: In Hong Kong,
nocturia emerged as the most prevalent and one of the most bothersome
symptoms among men who sought urologist care for lower urinary tract
symptoms. Compared with the non–Hong Kong population, Hong Kong
respondents tended to be highly symptomatic and bothered. They were,
however, less likely to have received treatment and were generally less
satisfied with previous treatment.
New knowledge added by this study
- Although day-time voiding symptoms have long been regarded as the more bothersome lower urinary tract symptom, results from this survey showed that nocturia was exceedingly common and could be highly bothersome to Hong Kong patients.
- Patients who presented to urologists in Hong Kong were highly symptomatic and bothered, and were less likely to have been treated before or were less satisfied with previous treatment compared with patients in other South-East Asian countries.
- To continuously improve quality of care and accommodate an increasing service demand, there is a need to further strengthen the provision of resources and education along the continuum of care for lower urinary tract symptoms, including the primary and secondary care, for the general public and patients.
Introduction
Lower urinary tract symptoms (LUTS) collectively
represent a common condition among ageing men.1
2 There are limited data on the
frequency of individual symptoms in patients who seek specialist care. It
is well established that LUTS have far reaching impacts on patients’ daily
lives.3 4
There are standard tools available to assess the severity of LUTS, such as
the International Prostate Symptom Score, but they do not reflect the
degree to which patients are subjectively bothered by symptoms. Patient
perception also depends on their cultural and religious background.
Treatment satisfaction and other patient-reported
outcomes are increasingly recognised as important measures of the
effectiveness of care delivery in addition to clinical parameters.5 These measures allow health care providers to assess
the quality of care that takes account of patient expectations and
preferences. As more treatment options have become available, it would be
of interest to assess this dimension of health care quality in patients
with LUTS.
The aim of this survey was to explore South-East
Asian patients’ perception of LUTS and their treatment. Self-reported
prevalence, bother, treatment, and treatment satisfaction of selected
symptoms including storage (urgency, nocturia), voiding (slow stream), and
post-micturition symptoms (dribble) were evaluated. In addition, patients’
perception of the cause of nocturia and use of non-prescribed treatment
for this symptom were explored. The study adopted a cross-sectional design
and a convenience sample of patients who sought specialist care from
across the region, namely Hong Kong, Malaysia, Philippines, Singapore,
Thailand, and Vietnam. The study explored current unmet needs and will be
used to guide the development of patient-centred management strategies.
This sub-analysis evaluated data from the Hong Kong subpopulation.
Methods
Subjects
We performed a cross-sectional study in 15 urology
clinics—three from Hong Kong and 12 from South-East Asian countries (2
from Malaysia, 2 from the Philippines, 1 from Singapore, 3 from Thailand,
and 4 from Vietnam). Hong Kong data were derived from a survey of patients
conducted during December 2014 to October 2015. The study involved
consecutive new patients who fulfilled the following eligibility criteria:
(1) male aged ≥18 years who were attending the clinic for the first time,
and (2) sought consultation at a urology clinic because of LUTS that had
been present for at least 1 month. In this study, LUTS included increased
daytime frequency, nocturia, urinary urgency, urinary incontinence, slow
or weak stream, hesitancy, intermittency, straining, terminal dribble,
sensation of incomplete bladder emptying, and post-micturition dribble.
Such symptoms were defined according to the report from the
Standardisation Sub-committee of the International Continence Society.6 Exclusion criteria were: (1) intermittent/indwelling
catheterisation; (2) known prostate or bladder cancer; (3) spinal cord
injury; (4) urethral stricture; (5) LUTS due to other causes, such as
suspected or known urinary infection (cystitis or prostatitis); and (6)
difficulty in understanding written information.
This survey involved major urology centres in
South-East Asia. These centres were chosen because of two reasons: (1)
they were major centres that saw 50 to 500 patients per week, and (2)
there was a prior working relationship with the study group. Ethics
approval from the Research Ethics Committee and Institutional Review Board
were sought as required by the participating centres.
Questionnaire
A patient self-administered questionnaire was
developed by the Southeast Asia Urology Think Tank that comprised a group
of urology specialists. The questionnaire assessed (a) demographics
(country of residence, age-group); (b) presence/absence, bother,
treatment, and treatment satisfaction of each of the following symptoms:
urgency, nocturia, slow stream, and post-micturition dribble; (c)
perception of the cause of disease and use of non-prescribed treatment for
nocturia; and (d) where appropriate, satisfaction with transurethral
resection of the prostate (TURP). The questionnaire in Chinese used in
Hong Kong and the original questionnaire in English are shown in the Appendices.
For questions that related to the level of ‘bother’, responses ranged from
“bother me a lot”, “bother me some”, “bother me a little”, to “not at all
bothersome”. For treatment satisfaction, patients were asked to choose
from the four categories: “very satisfied”, “satisfied”, “unsatisfied”,
and “very unsatisfied”.
Translation and linguistic validation
The questionnaire was translated from the original
English language into traditional Chinese. The translation of the
questionnaire was performed in the ethnographic mode to maintain the
meaning and cultural content. The questionnaire was back translated to the
original language by an independent translator for each language. The
versions were compared and any major differences were reconciled. An
expert in survey research and a subject expert (ie a urologist) reviewed
the translations to ensure the text was accurate, equivalent to the
original, written at an appropriate level (ie understood by the general
public), and took account of any cultural differences. A pre-test was
performed in a sample of subjects prior to distribution to the entire
sample to identify and correct any issues with clarity, relevance, and
comprehensiveness, as well as user-friendliness of the questionnaire. The
translations were revised after the pre-test and finalised by the
urologist.
Data collection
A urologist or member of the clinic staff was
required to screen all consecutive new patients who presented to the
urology clinic and identify potential study participants. They approached
those patients who appeared eligible and explained the study to them. A
patient questionnaire with an information sheet was distributed to each
eligible consenting patient. Upon completion of the survey, the
respondents sealed the questionnaire in an envelope and submitted it to
the urologist who completed the eligibility checklist printed at the back
of the questionnaire. The urologist then placed the questionnaire in an
onsite lock box. Clinic staff periodically emptied the lock box and posted
the contents to the data collection centre. Written informed consent was
obtained from all eligible participants. To evaluate the response rate,
participating centres were required to return a blank questionnaire for
each eligible patient who refused to participate.
Statistical analysis
The sample size of 200 evaluable responses from
each country was powered to detect a prevalence rate of 46% based on a
previous study,6 with type 1 error
of 0.05 and margin error not exceeding 7%. We used the SPSS (Windows
version 24.0; IBM Corp, Armonk [NY], US) to analyse the data. Descriptive
statistics were used to calculate the prevalence of LUTS, and the
distribution of participants’ individual characteristics such as
‘bothersome level’, use of prescribed treatment, and satisfaction with
specific treatments. Means and 95% confidence intervals are reported.
Categorical variables are presented as percentages and compared using Chi
squared test. Association rule analysis (also known as market basket
analysis) was conducted using the statistical package R to examine symptom
combination. Cochran-Armitage trend test was used to test the trend for
nocturnal voiding frequency and the level of symptom-associated bother.
Results
Between March and May 2014, a pilot survey was
carried out to evaluate the applicability of the questionnaire and data
collection procedure. The field test involved centres in Hong Kong,
Malaysia, Philippines, Singapore, Thailand, and Vietnam. In each of these
regions, the questionnaire was self-administered by approximately 30
respondents. A total of 233 questionnaires were received from all regions:
high response rates of >90% were reported by the centres. Overall,
respondents rated the questionnaire positively. The mean time taken to
complete the questionnaire was 5.4 minutes.
Overall, clarity of the layout and instructions
required improvement to minimise illogical/missing responses, for example,
use of strong visual symbols such as arrows to direct respondents to the
next question if the answer was YES/NO.
Of the 1436 questionnaires collected from all
regions, 17 were deemed ineligible based on the exclusion criteria and
three were blank. A total of 225 evaluable responses from Hong Kong were
collated for analysis. Between December 2014 and October 2015, a total of
71 evaluable responses were collected from Prince of Wales Hospital, 65
from Queen Elizabeth Hospital and 89 from Tuen Mun Hospital.
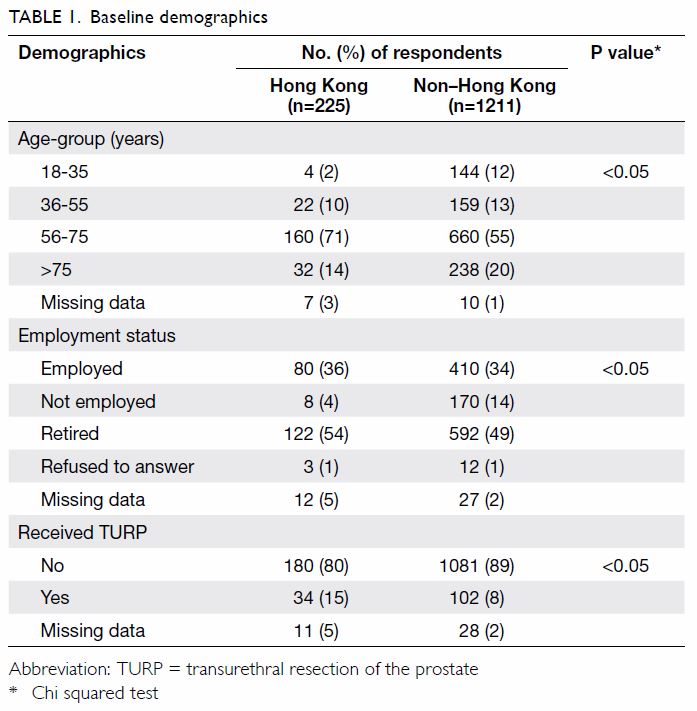
Patient characteristics
In the Hong Kong sample, most respondents were aged
56 to 75 years (71%), retired (54%), and had not undergone TURP (80%).
Compared with the non–Hong Kong population, Hong Kong respondents were
older and more likely to have received TURP (P<0.05; Table
1).
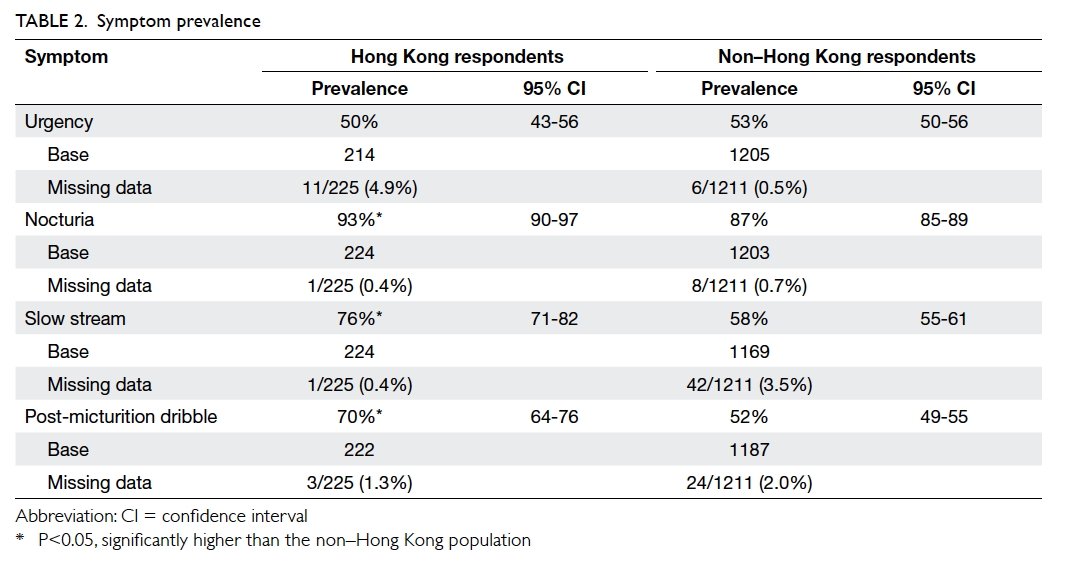
Symptom prevalence
Among the respondents in Hong Kong who sought care
at the urology clinics, LUTS were prevalent, with nocturia the most common
(93%; 95% confidence interval [CI], 90%-97%), followed by slow stream
(76%; 95% CI, 71%-82%), post-micturition dribble (70%; 95% CI, 64%-76%),
and urgency (50%; 95% CI, 43%-56%). Relative to the non–Hong Kong
respondents, the prevalence was significantly higher for all four LUTS
except urgency (Table 2).
A considerable number of respondents in Hong Kong
reported having more than one symptom to some degree: 35% of them had all
four symptoms, 32% reported three symptoms, 22% two symptoms, and only 9%
a single symptom. With regard to symptom combinations, the strongest
association was found for post-micturition dribble and co-existing
urgency, nocturia, and slow stream (support: 0.353; confidence: 0.872;
lift value: 1.249).
Symptom bother and treatment satisfaction
When asked to evaluate how bothersome their
symptoms were, more than half of respondents in Hong Kong felt at least
some degree of bother (ie “bother me some” or “bother me a lot”)—73% for
urgency and post-micturition dribble, 70% for nocturia, and 68% for slow
stream. When nocturia was defined as waking up twice or more at night, it
became the symptom with which the most respondents reported at least some
bother (77%). The Hong Kong respondents showed a consistent trend for a
higher percentage for all symptoms studied compared with the non–Hong Kong
group (Table 3).
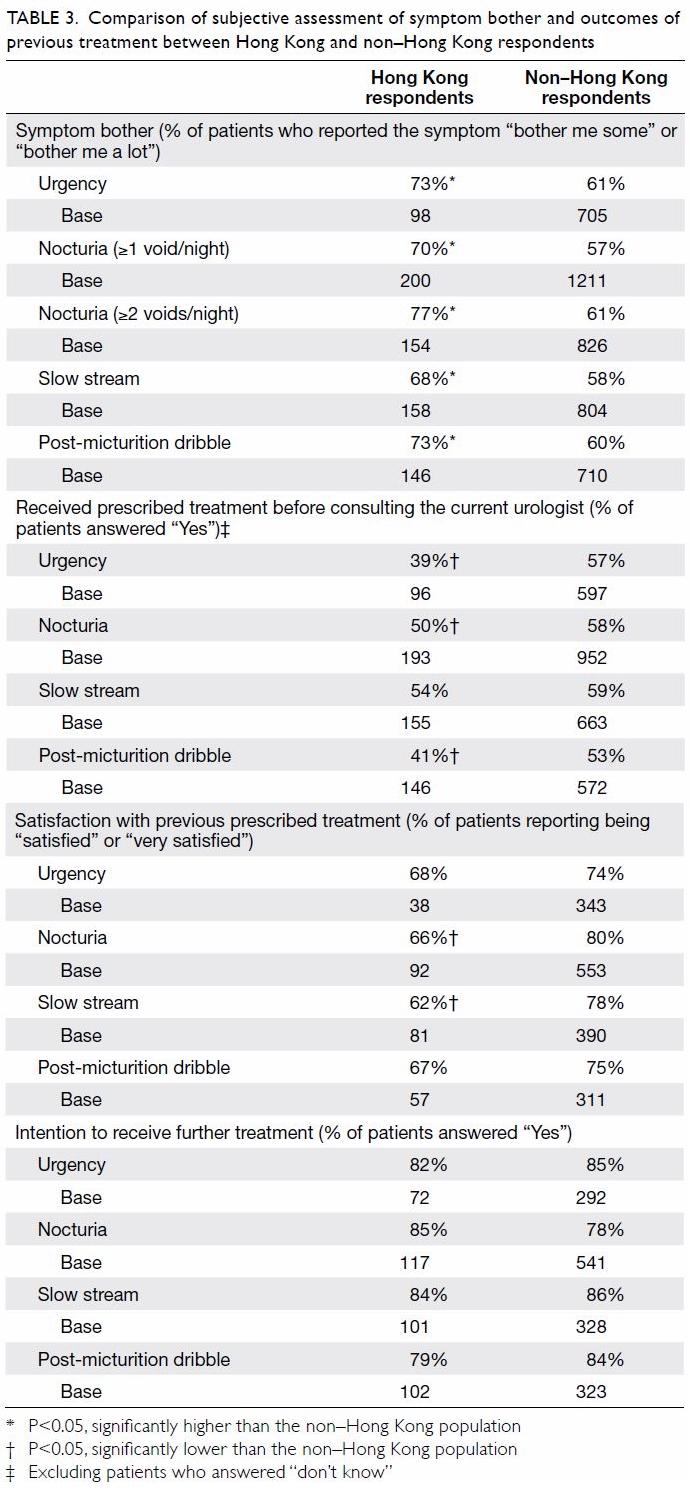
Table 3. Comparison of subjective assessment of symptom bother and outcomes of previous treatment between Hong Kong and non–Hong Kong respondents
Among the respondents in Hong Kong, 39% to 54% had
received prescribed treatment. Less respondents with nocturia in Hong Kong
received prescribed treatment compared with the non–Hong Kong population.
The same applied to those with post-micturition dribble and urgency (Table
3).
More than 60% of respondents in Hong Kong reported
being “satisfied” or “very satisfied” with previous prescribed treatment.
Among the symptoms, the overall satisfaction rate was lower for nocturia
and slow stream compared with the non–Hong Kong population. Most
respondents in Hong Kong (79%-85%) indicated they would like to receive
further treatment (Table 3).
A comparison of respondents’ subjective assessment
of symptom bother, and outcomes of previous treatment from all regions is
shown in Table 4.

Table 4. Comparison of subjective assessment of symptom bother and outcomes of previous treatment among all regions
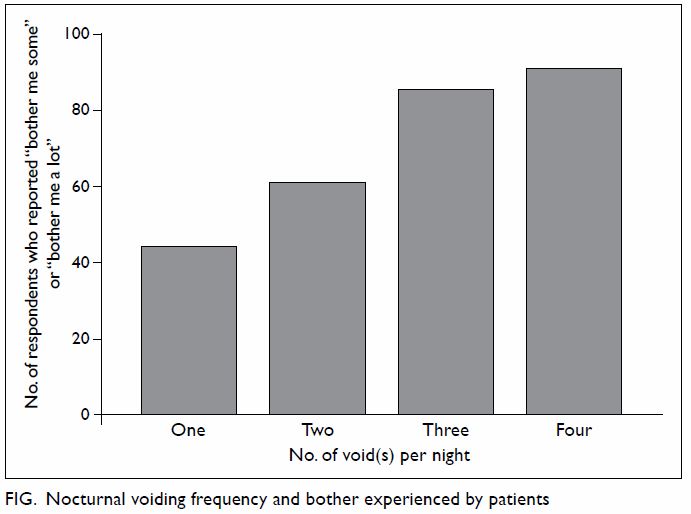
Nocturia: patient perception
Of those respondents who claimed to have nocturia,
77% reported at least two voids per night (Table 3). More frequent voiding was associated with
a higher level of bother, ie more respondents reported “bother me some” or
“bother me a lot” (Cochran-Armitage trend test, Z= –5.3044, P<0.0001; Fig). More than half (53%) of respondents regarded
the prostate as the main cause of nocturia, and 39% answered “don’t know”.
Some respondents (17%) had taken non-prescribed treatment for nocturia,
including herbal medicines and supplements.
Symptom improvement after transurethral resection of
the prostate
Only a small proportion (15%) of respondents had
previously undergone TURP. More than half of respondents reported improved
symptoms following surgery (Table 5). The small number of respondents and
occurrence of multiple symptoms in individual respondents made it
difficult to compare the improvement rates across symptoms.
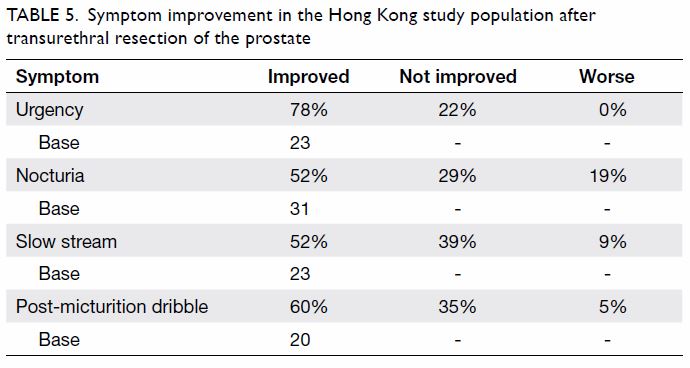
Table 5. Symptom improvement in the Hong Kong study population after transurethral resection of the prostate
Discussion
Symptom profiles of respondents
The survey provided information on the
characteristics of men with LUTS who attended urology clinics in Hong
Kong. The respondents were mostly elderly, retired, and had not undergone
any prostate surgery. The most commonly reported symptoms were nocturia
and slow stream. Almost 80% of respondents with nocturia awoke at least
twice per night to void. This was by far the most bothersome symptom
followed by daytime symptoms, urgency, and post-micturition dribble. This
finding is in line with results from previous studies conducted in a
primary care setting that reported nocturia as a significant driving
factor to trigger medical consultations.7
8 Nocturia could be highly
bothersome to patients. Waking during the night to void disrupts sleep for
both the patient and their partner, and impaired sleep is known to affect
quality of life. We also established that LUTS often co-exist, and are in
line with the EpiLUTS in Korea9 and
Europe.10 In this study, the
association rules analysis further revealed that in the local population,
for respondents with urgency, slow stream and nocturia, there was an 87%
risk of co-existing post-micturition dribble.
Respondent’s perception of bother and satisfaction with
previous treatment
The survey findings help identify patient needs by
exploring respondents’ perceived degree of bother and treatment
satisfaction. Compared with the non–Hong Kong population, Hong Kong
respondents tended to report a higher level of symptom bother
(approximately 70% experiencing “some” or “a lot” bother), were less
likely to have received prescribed treatment before consulting the current
urologist, and reported lower treatment satisfaction. This could be due to
several reasons: (1) cultural differences in patient perception of the
symptom bother and their treatment expectation; (2) higher referral
threshold for primary care practitioners in Hong Kong; (3) more
conservative practice of primary care physicians (eg more use of watchful
waiting); and (4) a longer waiting time to access urology specialty
services.
One distinguishing feature of the Hong Kong health
care system from other participating countries is that a primary care
physician referral system is in place in Hong Kong. A greater involvement
of the primary care sector in the management of LUTS is believed to allow
a more rational use of resources as a result of reduced time spent on
waiting lists, earlier therapy, and increased access to specialist
services for those in need of extensive investigations or surgery.11 In this sense, it is understandable that it is those
mostly highly symptomatic patients who have failed medical therapy are
referred to urologists. Intriguingly, fewer respondents in Hong Kong than
in other South-East Asian countries reported being given prescribed
treatment, suggesting that primary care physicians adopt a more
conservative approach to the treatment of LUTS, although this remains to
be confirmed with findings from medical records.
Local data are limited whereas overseas studies
showed that primary care physicians are more likely to engage in watchful
waiting than urologists. Fewer men received recommended diagnostic
evaluations from primary care physicians than from urologists, such as
uroflowmetry, bladder scans, and cystoscopy. Primary care physicians
ordered tests such as creatinine measurement that are less frequently used
by urologists. Primary care physicians were also more likely to prescribe
an older, long-acting alpha blocker that requires dose titration, and less
likely to prescribe combination therapy such as 5-alpha-reductase
inhibitor and anticholinergic therapy.12
13 Interdisciplinary care plans,
detailed inter-physician referral and consultation letters, and integrated
clinics have been suggested to improve physician communication and patient
care.14 15
Satisfaction with care is an important outcome. It
is multidimensional, comprising satisfaction with the care process and
with care outcomes, and involves the patient’s personality and
expectations and the health care provider’s interpersonal skills as well
as technical excellence. The components of the care process may include
waiting times, provision of information, access to care, adequacy of care
environment, and speed of treatment. The other major element of the
satisfaction domain concerns care outcome. Individuals whose outcome is
either below personal expectations or who experience treatment
side-effects may be less satisfied with the care they have received.16
Respondents’ understanding of lower urinary tract
symptoms
In terms of the cause of nocturia, 39% of
respondents responded “don’t know” and 53% regarded the prostate as the
primary cause. This indicates a need for more education and better
physician-patient communication. Surveys conducted in Korea and Europe
showed that it is the complications of LUTS more than the actual symptoms
with which respondents are most concerned.17
18 Because primary care physicians
are usually the first point of medical contact for men with LUTS, they can
play an important role in educating patients and diagnosing the condition.13
Study strengths and limitations
This is a large-scale multinational study that
assesses LUTS and their treatment from the patients’ perspective at a
secondary care level. Our study had several limitations. First, the
subjects surveyed were patients who were bothered by their symptoms and
who sought a urology opinion and agreed to participate in this study.
Results of this self-administered survey were subject to recall bias, for
examples, about medication received, number of voids at night, and quality
of treatment received from their previous physicians. Further study is
required to explore an association with clinical assessment. Second,
convenience sampling limited the representativeness of the study sample.
Third, the response rates of this study were estimated by the number of
blank questionnaires returned; each of which indicated a refusal to
participate. Centres might not follow this closely in practice and the
reasons for non-participation were not recorded. This may have introduced
potential response bias. Fourth, missing data are attributed to the
involvement of older adults in this survey. Fifth, following the
completion of the pilot survey, the questionnaire was later revised to
improve clarity of the layout and instructions to minimise
illogical/missing responses, for example, use of strong visual symbols
such as arrows to direct respondents to the next question if the answer is
YES/NO. Lastly, the questionnaires included only four predominant LUTS.
Although these core symptoms are the main factors in the assessment of
LUTS, it is possible that lack of assessment of other symptoms limited our
understanding of all LUTS symptomatology. When interpreting the results,
it is important to take into account the differences among
cities/countries, referral systems, waiting list times, and socio-economic
composition of the samples.
The way forward
The demand for specialist care in the management of
LUTS is expected to rise with increasing life-expectancy. Currently, TURP
is the most common elective surgery in Hong Kong—about 3000 operations are
performed at hospitals managed by the Hospital Authority each year.19 To keep pace with the increasing patient load and to
improve the quality of care, findings from this study call for better
streamlining of the shared-care model between general practitioners and
urologists. More resources are required that will enable increased access
to urology specialty services. This study provides an insight into the
overall patient satisfaction with previous treatment before presentation
to a specialist clinic. A complete evaluation of health care quality that
examines different dimensions—such as structure, process, and quality of
care—is warranted.
Conclusions
The survey provided much-needed information about
patient perspectives regarding symptoms, bother, and treatment of LUTS.
There is room for improvement in the quality of care provided to LUTS
patients.
Declaration
All authors have disclosed no conflicts of
interest.
References
1. Yee CH, Li JK, Lam HC, Chan ES, Hou SS,
Ng CF. The prevalence of lower urinary tract symptoms in a Chinese
population, and the correlation with uroflowmetry and disease perception.
Int Urol Nephrol 2014;46:703-10. Crossref
2. Wong SY, Woo J, Hong A, Leung JC, Kwok
T, Leung PC. Risk factors for lower urinary tract symptoms in southern
Chinese men. Urology 2006;68:1009-14. Crossref
3. Glover L, Gannon K, McLoughlin J,
Emberton M. Men’s experiences of having lower urinary tract symptoms:
factors relating to bother. BJU Int 2004;94:563-7. Crossref
4. Gannon K, Glover L, O’Neill M, Emberton
M. Lower urinary tract symptoms in men: self-perceptions and the concept
of bother. BJU Int 2005;96:823-7. Crossref
5. Abrams P, Andersson KE, Birder L, et al.
Fourth International Consultation on Incontinence Recommendations of the
International Scientific Committee: evaluation and treatment of urinary
incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol
Urodyn 2010;29:213-40. Crossref
6. Li MK, Garcia LA, Rosen R. Lower urinary
tract symptoms and male sexual dysfunction in Asia: a survey of ageing men
from five Asian countries. BJU Int 2005;96:1339-54. Crossref
7. Abrams P, Cardozo L, Fall M, et al. The
standardisation of terminology in lower urinary tract function: report
from the standardisation sub-committee of the International Continence
Society. Urology 2003;61:37-49. Crossref
8. Lai UC, Wun YT, Luo TC, Pang SM. In a
free healthcare system, why do men not consult for lower urinary tract
symptoms (LUTS)? Asia Pac Fam Med 2011;10:7. Crossref
9. Kim TH, Han DH, Lee KS. The prevalence
of lower urinary tract symptoms in Korean men aged 40 years or older: a
population-based survey. Int Neurourol J 2014;18:126-32. Crossref
10. Irwin DE, Milsom I, Hunskaar S, et al.
Population-based survey of urinary incontinence, overactive bladder, and
other lower urinary tract symptoms in five countries: results of the EPIC
study. Eur Urol 2006;50:1306-14; discussion 1314-5. Crossref
11. Fonseca J, Martins da Silva C. The
diagnosis and treatment of lower urinary tract symptoms due to benign
prostatic hyperplasia by primary care family physicians in Portugal. Clin
Drug Investig 2015;35(Suppl 1):19-27. Crossref
12. Spatafora S, Canepa G, Migliari R, et
al. Effects of a shared protocol between urologists and general
practitioners on referral patterns and initial diagnostic management of
men with lower urinary tract symptoms in Italy: the Prostate Destination
study. BJU Int 2005;95:563-70. Crossref
13. Miner MM. Primary care physician
versus urologist: how does their medical management of LUTS associated
with BPH differ? Curr Urol Rep 2009;10:254-60. Crossref
14. Lopéz BM, Romero AH, Ortín EO, Garcia
IL. Can primary care physicians manage benign prostatic hyperplasia
patients as urologists do? Eur Med J Urol Jul 2014:1-8.
15. Wei JT, Miner MM, Steers WD, et al.
Benign prostate hyperplasia evaluation and management by urologists and
primary care physicians: practice patterns from the observational BPH
Registry. J Urol 2011;186:971-6. Crossref
16. Roehrborn CG, Nuckolls JG, Wei JT,
Steers W; BPH Registry and Patient Survey Steering Committee. The benign
prostatic hyperplasia registry and patient survey: study design, methods
and patient baseline characteristics. BJU Int 2007;100:813-9. Crossref
17. George AK, Sandra MG. Measuring
patient satisfaction. In: Penson DF, Wei JT, editors. Clinical research
methods for surgeons. New Jersey: Humana Press; 2006: 253-65.
18. Kim SI, Kang JY, Lee HW, Seong do H,
Cho JS. A survey conducted on patients’ and urologists’ perceptions of
benign prostatic hyperplasia. Urol Int 2011;86:278-83. Crossref
19. Leung KK, So HS. Evolution of care for
patients undergoing transurethral resection of prostate. Available from:
https://www3.ha.org.hk/haconvention/hac2014/proceedings/downloads/SPPE559.pdf.
Accessed 16 May 2016.