DOI: 10.12809/hkmj166140
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
MEDICAL PRACTICE
Diabetes in older people: position statement of The
Hong Kong Geriatrics Society and the Hong Kong Society of Endocrinology,
Metabolism and Reproduction
CW Wong, FHKAM (Medicine), FHKCP1;
Jenny SW Lee, FHKAM (Medicine), MD (CUHK)2; KF Tam, FHKAM
(Medicine), FRCP (Edin, Glasg)3; HF Hung, FHKAM (Medicine),
FHKCP4; WY So, FHKAM (Medicine), MD (CUHK)5; CK
Shum, FHKAM (Medicine), FHKCP6; CY Lam, FHKAM (Medicine), FHKCP7;
JN Cheng, FHKAM (Medicine), FHKCP1; SP Man, FHKAM (Medicine),
FHKCP8; TW Auyeung, FHKAM (Medicine), FHKCP8
1 Department of Medicine and
Geriatrics, Caritas Medical Centre, Sham Shui Po, Hong Kong
2 Department of Medicine and
Geriatrics, Tai Po Hospital, Tai Po, Hong Kong
3 Department of Medicine, Hong Kong
Buddhist Hospital, Lok Fu, Hong Kong
4 Department of Medicine and
Geriatrics, Princess Margaret Hospital, Lai Chi Kok, Hong Kong
5 Department of Medicine and
Therapeutics, Prince of Wales Hospital, Shatin, Hong Kong
6 Department of Medicine and
Geriatrics, Tuen Mun Hospital, Tuen Mun, Hong Kong
7 Department of Medicine, Queen
Elizabeth Hospital, Jordan, Hong Kong
8 Department of Medicine and
Geriatrics, Pok Oi Hospital, Yuen Long, Hong Kong
Corresponding author: Dr CW Wong (chitwaiwong@hotmail.com)
Abstract
Following a survey on the clinical practice of
geriatricians in the management of older people with diabetes and a study
of hypoglycaemia in diabetic patients, a round-table discussion with
geriatricians and endocrinologists was held in January 2015. Consensus was
reached for six domains specifically related to older diabetic people: (1)
the considerations when setting an individualised diabetic management; (2)
inclusion of geriatric syndrome screening in assessment; (3) glycaemic and
blood pressure targets; (4) pharmacotherapy; (5) restrictive diabetic
diet; and (6) management goals for nursing home residents.
Introduction
The prevalence of diabetes increases with age such
that among the older population (age ≥65 years), it was 6 times that of
the younger population (age 18-64 years), reaching 21.4% in Hong Kong in
2004 to 2005.1 Although the
prevalence among older people is quite constant over time, with an ageing
population the number of older people with diabetes is expected to
continuously increase in the future.
In addition to the increasing population of older
diabetic people, heterogeneity among older people with varying levels of
cognitive and functional ability, life expectancy, and social support
present a challenge in clinical practice because there is no single
treatment goal or management plan that can address all of the issues in
this patient group. Recently, individualised and tailored care approaches
to cater for the individual characteristics of older people have been
promoted.2 3 4 5 6 7 Increasing attention to avoid treatment-related
hypoglycaemia has also been emphasised.2
3 4
5 6
7 However, there is a gap in
knowledge of the optimal management due to the paucity of clinical trials
among older diabetic people, in particular those with frailty. This has
led to a lack of consensus and variation of management in clinical
practice.
A special interest group on diabetes mellitus,
under the auspices of The Hong Kong Geriatrics Society (HKGS), has been
established to raise the awareness of diabetes among older people; to
address the special issues of older people associated with their varied
physical, cognitive, and social needs; and to enhance their care. A survey
on the opinions of local geriatricians about diabetes management in older
people and data analysis of hypoglycaemia among diabetic patients in the
local public sector were performed. A round-table discussion with
geriatricians from the HKGS and endocrinologists from the Hong Kong
Society of Endocrinology, Metabolism and Reproduction was then held on 24
January 2015. Discussion was based on evidence-based review of the current
literature, scientific presentations by experts in the field, opinions
from both geriatricians and endocrinologists, and the analysis of local
data on hypoglycaemia of the diabetic patients. After the meeting,
statements were drafted and circulated among the council members of HKGS
and the Hong Kong Society of Endocrinology, Metabolism and Reproduction
for comments. The final version was approved by all participants. The
purpose of the round-table discussion was to arrive at a consensus on the
management approach for older people with diabetes. This position
statement was developed to serve as a reference for local clinicians.
Survey on the clinical practice of geriatricians in the
management of older people with diabetes
An online survey was conducted to collect the
opinions of geriatricians about the management of type 2 diabetes in older
people between December 2014 and January 2015 (Appendix 1). The
questionnaires were distributed to all 113 members of the HKGS.
Approximately half (46.3%) of the HKGS members returned the
questionnaires. The following summarises the results of the questionnaire;
details are shown in Appendix 2.
Individualised diabetes management
Most (60%) of the respondents ranked risk of
hypoglycaemia as the most important domain in setting an individualised
diabetes management plan. Physical and mental functions, and
co-morbidities and associated vascular diseases were also considered to be
important.
Geriatric syndromes
Almost all of the respondents agreed that physical
frailty (98%) and cognitive impairment (96%) should be assessed when
managing older people with diabetes. More than 80% of respondents agreed
that polypharmacy and nutritional problems should also be assessed.
Target glycaemic and blood pressure control
Respondents agreed that an individual’s
co-morbidities, cognitive and functional status, and life expectancy must
be considered when determining a glycaemic goal, such that more stringent
control (target glycated haemoglobin [HbA1c] 6.5%-7%) should be considered
for robust elderly people (59% of respondents), less stringent control
(target HbA1c 7%-9%) for those who are physically frail or cognitively
impaired (52%-57% of respondents), and relaxed control (target HbA1c ≥9%)
for those receiving end-of-life care (50% of respondents). Blood pressure
targets set for older diabetic people were quite varied among the
respondents; these ranged from ≤130/80 mm Hg to ≤150/90 mm Hg for robust
elderly people, and ≤160/100 mm Hg and avoidance of diastolic blood
pressure of <60 mm Hg for those at the end of life.
Pharmacotherapy
The risk of hypoglycaemia was the most important
concern for almost all the respondents (98%) when prescribing
glucose-lowering therapy. Dosing frequency was also a major concern (76%
of respondents). A vast majority (93% of respondents) would prescribe
metformin as the first-line glucose-lowering therapy for robust elderly
people, while a dipeptidyl peptidase-IV (DPP-IV) inhibitor (45%) or
sulphonylurea (45%) was considered suitable for older people with organ
failure or estimated glomerular filtration rate of <30 mL/min, and
metformin (52%) and a DPP-IV inhibitor (34%) was considered suitable for
those at high risk of hypoglycaemia.
Non-pharmacotherapy
A majority (>80%) of respondents considered that
a restrictive diabetic diet should only be allocated for robust elderly
people, but not for octogenarians, physically frail or cognitively
impaired patients, and nursing home residents.
Goals for nursing home residents
Preventing hypoglycaemia was the goal of almost all
the respondents (98%). This was followed by preventing hospitalisation and
avoiding acute metabolic complications (approximately 80% of respondents).
A study of hypoglycaemia in diabetic patients in Hong
Kong
A study of hypoglycaemia in the older diabetic
population was performed. The study involved collection of data from the
Clinical Data Analysis and Reporting System. Clinical data on diabetic
people attending the accident and emergency department (AED) with the
diagnosis of hypoglycaemia were collected. The study involved two parts:
(1) analysis of all the AED attendance data on diabetic patients diagnosed
with hypoglycaemia during the period between 1 July 2013 and 30 June 2014;
and (2) subanalysis of data of diabetic patients attending the AED for
hypoglycaemia from five hospitals (Alice Ho Miu Ling Nethersole Hospital,
Caritas Medical Centre, Pok Oi Hospital, Queen Elizabeth Hospital, and
Tuen Mun Hospital) during the period between 1 January 2014 and 31 January
2014.
Accident and emergency department visits for
hypoglycaemia among diabetic patients in Hong Kong during a 1-year period
between 1 July 2013 and 30 June 2014
A total of 2416 diabetic patients had attended all
AEDs under the Hospital Authority in Hong Kong for hypoglycaemia between 1
July 2013 and 30 June 2014. The majority (78.2%) of them were aged 65
years or older; 14.4% were from old-age homes, and the hospital admission
rate was 81.1% (Table 1). Older patients (≥65 years) had a
significantly higher rate of hospital admission and 12-month mortality
than patients younger than 65 years.
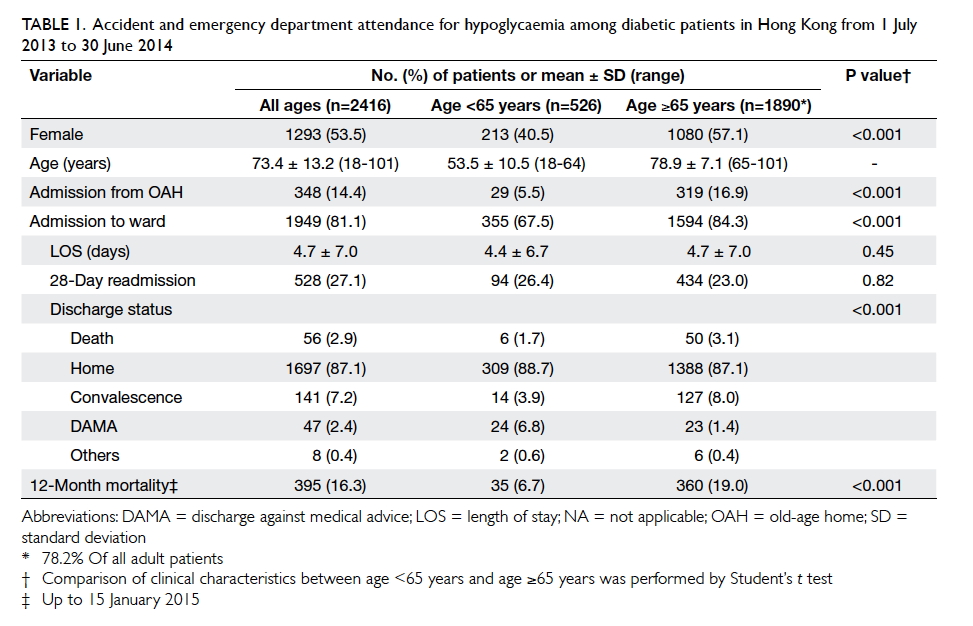
Table 1. Accident and emergency department attendance for hypoglycaemia among diabetic patients in Hong Kong from 1 July 2013 to 30 June 2014
Subanalysis of accident and emergency department visits
for hypoglycaemia from five hospitals between 1 January 2014 and 31
January 2014
Of the 133 diabetic patients included in the
subanalysis, 105 (78.9%) were older patients (≥65 years) [Table
2]. Tight glycaemic control with HbA1c of ≤7% was associated with a
significantly higher 12-month mortality in older diabetic patients than
those with less stringent control (27.8% vs 11.8%; P=0.04). In addition,
older patients with very tight glycaemic control (HbA1c ≤6%) had a longer
duration of stay in hospital than those with less stringent control (6.8
days vs 3.8 days; P=0.001). On the other hand, loose glycaemic control
with HbA1c of ≤8% and patients aged younger than 65 years were not
associated with increased short-term (28-day readmission) and long-term
(12-month mortality) adverse outcomes. Multivariate analysis showed that
male sex, higher Charlson Comorbidity Index score, dementia, and lower
HbA1c level were independent predictors for 12-month mortality among the
older diabetic patients (Table 3).
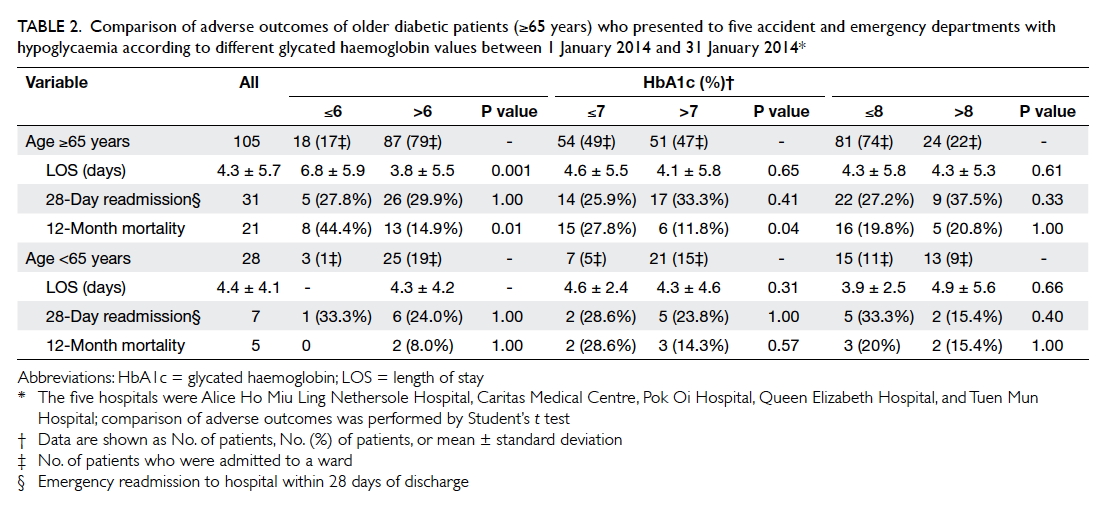
Table 2. Comparison of adverse outcomes of older diabetic patients (≥65 years) who presented to five accident and emergency departments with hypoglycaemia according to different glycated haemoglobin values between 1 January 2014 and 31 January 2014
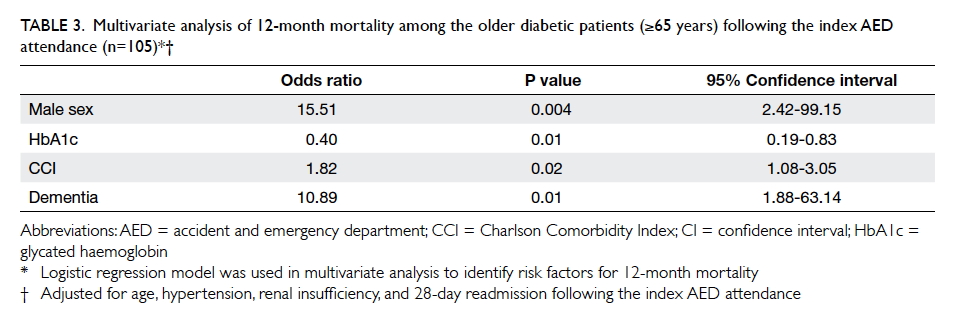
Table 3. Multivariate analysis of 12-month mortality among the older diabetic patients (≥65 years) following the index AED attendance (n=105)
Factors to be considered in the management of older
people with type 2 diabetes mellitus
Hypoglycaemic risk
Advanced age is an independent risk factor for
hypoglycaemia.8 Older people are
intrinsically prone to hypoglycaemia. With increasing age, hypoglycaemic
warning symptoms become less intense and hypoglycaemic unawareness becomes
more common even with intact physiological glucose counter-regulatory
response (ie decreased insulin secretion, and increased glucagon and
epinephrine secretion).9 10 11 12 Furthermore, the physiologically higher blood glucose
level for the initiation of neurogenic warning symptoms (eg palpitation,
tremor, and sweating—the result of automonic activation) than that for
onset of neuroglycopenic symptoms (eg confusion, seizure, and loss of
consciousness—the result of brain glucose deprivation), which allows time
to take measures to avoid neuroglycopenia and severe hypoglycaemia, tends
to be lost in the older people.12
The impaired perception of the warning symptoms of hypoglycaemia and the
narrower or even absence of a glycaemic threshold gap between the
development of neurogenic and neuroglycopenic symptoms put elderly people
at a high risk for severe hypoglycaemia.
Furthermore, with a longer duration of type 2
diabetes and subsequent progression to endogenous insulin deficiency,
counter-regulatory responses to hypoglycaemia are compromised.
Additionally, the neurogenic warning symptoms become attenuated and lead
to hypoglycaemic unawareness. Compromised glucose counter-regulation and
hypoglycaemia unawareness increase the risk of severe iatrogenic
hypoglycaemia by 25-fold and 6-fold, respectively.13 14 Multiple
co-morbidities, polypharmacy, and cognitive dysfunction associated with
advancing age are also risk factors for hypoglycaemia (see below).
Geriatric syndromes
Diabetes predisposes older people to the
development of geriatric syndromes as it is associated with risk for
dementia, depression, polypharmacy, fall and fracture, urinary
incontinence, visual impairment, and chronic pain. The presence of
geriatric syndromes is linked with functional decline and increasing
frailty that would limit a patient’s functional independence and
complicate medical management. Early recognition and including geriatric
syndromes in the management plan are recommended.
Cognitive dysfunction
Patients with diabetes are at increased risk for
dementia. They have been shown to have a 1.2- to 1.5-fold higher rate of
decline in cognitive function than those without diabetes,15 and were at a higher risk for developing Alzheimer’s
disease and vascular dementia by approximately 1.5-fold and 2.5-fold,
respectively.16 Additionally,
adverse effect of treatment-related hypoglycaemia, especially if it is
severe, has been shown to be associated with subsequent dementia in older
diabetic patients.17 18 19 There was
also a graded increase in dementia risk with the number of severe
hypoglycaemic episodes experienced, such that the risk was almost double
for three or more episodes when compared with only one episode.17 Furthermore, there is a bidirectional association of
hypoglycaemia with dementia in which hypoglycaemia damages the brain and
that, in turn, decreases one’s ability to manage diabetes or recognise
hypoglycaemic symptoms leading to the subsequent risk of hypoglycaemia,
that further impairs cognitive function in a vicious cycle.20
Depression
A systematic review and meta-analysis found people
with type 2 diabetes had a 24% increased risk of developing depression.21 On the other hand, depression
was associated with a 60% increased risk of type 2 diabetes in another
systematic review.22 Despite the
fact that depression in diabetic patients is common, it is often
undiagnosed and untreated.23 Like
cognitive dysfunction, depression may impede functionality and diabetic
self-management causing erratic timing of medication intake, irregular
eating, inability to self-monitor blood glucose, and failure to recognise
hypoglycaemic symptoms to enable prompt management. These may worsen
glycaemic control and increase the risk of diabetic and treatment-related
complications. Early detection of depression, especially in those with
unexplained decline in clinical status, is warranted.24
Polypharmacy
Medications prescribed for co-morbidities
predispose patients to the impact of polypharmacy. Because of the
age-related changes in pharmacokinetics and pharmacodynamics, the adverse
effects of drugs and drug-drug interactions are further exacerbated in
older patients. Older diabetic patients using four or more concomitant
medications have been found to be at increased risk for developing serious
hypoglycaemia.8 25 Polypharmacy can also precipitate geriatric syndromes
such as fall, cognitive impairment, urinary incontinence, and
malnutrition.26 27
Fall and fracture
Diabetic complications (such as autonomic
dysfunction with orthostatic hypotension, peripheral neuropathy with gait
disorder, and diabetic retinopathy with poor vision)28 and treatment complications (such as
metformin-associated vitamin B12 deficiency with resultant
neuropathy)29 increase the
susceptibility of diabetic patients to fall. Besides, diabetes has been
shown to be an independent risk factor for fracture.30 Patients who have longer diabetes duration,
suboptimal glucose control, diabetic retinopathy, insulin use or
thiazolidinedione use in women, and increased risk for fall are
particularly at high risk for fracture.30
31 32
Chronic pain and urinary incontinence
Neuropathic pain affects up to one third of
patients with diabetes and is more prevalent in women.33 Its occurrence may not relate to the severity of
neuropathy and may even occur in patients without clinical neuropathy.
Besides, pain from other sources such as bone, joint, and back is common
in older people. Urinary incontinence is also common in diabetic patients,
especially women. Up to one third of female patients with diabetes had
reported incontinence at least weekly in a survey in which urge
incontinence was associated with advancing age.34
Managing treatable causes such as urinary tract infection, faecal
impaction, use of offensive medications, and poor glycaemic control with
polyuria may alleviate incontinence.24
Both pain and urinary incontinence are often neglected in clinical
practice and may lead to adverse outcomes such as anxiety, depression,
decreased socialisation, fall and fracture if left untreated.35 36 37
Co-morbidities and other cardiovascular risk factors
As many as 40% of older people with diabetes have
four or more chronic conditions.38
Multiple co-morbidities may have profound effects on patients’ ability to
self-care. Additionally, the level of co-morbidities affects treatment
outcomes. Diabetic patients with low-to-moderate co-morbidity have been
found to have a lower incidence of cardiovascular events than those with
high co-morbidity, even with comparable HbA1c levels.39 Furthermore, co-morbidity, especially renal
impairment, hepatic disease and cognitive dysfunction increase the risk of
severe hypoglycaemia,25 which is
associated with twice the risk of cardiovascular disease (myocardial
infarction, congestive heart failure, stroke, and cardiovascular death) in
diabetic patients.40 Diabetic
patients with concomitant coronary artery disease who experience
hypoglycaemia are particularly prone to ischaemic heart attack.41 These have clinical implications—in patients with
multiple co-morbidities, intensive glucose treatment may not be beneficial,
but might make patients prone to treatment-related hypoglycaemia which, in
turn, may exacerbate the cardiovascular event, especially in those at risk
for cardiovascular disease.
Management of other cardiovascular factors to lower
the cardiovascular risk is also important. Systolic blood pressure (SBP)
of ≥140 mm Hg increases the risk of cardiovascular events, whereas
lowering blood pressure from a high level reduces both cardiovascular and
microvascular complications in older diabetic patients.42 43 44 There is no further benefit to lowering SBP to
<130 mm Hg however, as compared to SBP of 130-140 mm Hg, but may
increase mortality.45 46 Furthermore, a low diastolic blood pressure of <70
mm Hg that may result from SBP reduction is associated with higher
cardiovascular disease risk.42
Thus, the recommended target blood pressure for older diabetic patients is
<140/90 mm Hg, if tolerated.2
Lipid lowering by statins has been shown to reduce
the incidents of major vascular events by approximately 20% per mmol/L
low-density lipoprotein cholesterol reduction in diabetic patients and in
patients age ≥65 years.47 This
benefit emerges quite rapidly, within 1 to 2 years of treatment,
suggesting that most older people could benefit from statins except for
those with very limited life expectancy. There is limited evidence with
drugs other than statins for reduction of cardiovascular risk.
Is stringent glycaemic control beneficial?
The UKPDS (UK Prospective Diabetes Study) that
recruited patients with newly diagnosed type 2 diabetes (mean age, 53
years) showed a 25% risk reduction in microvascular complications in the
intensive-therapy group (HbA1c achieved, 7%) after a median follow-up of
11 years.48 Macrovascular benefit,
in terms of a 15% risk reduction for myocardial infarction, emerged only
during 10 years of extended post-trial follow-up.49
In three more recent large-scale trials—ACCORD (Action to Control
Cardiovascular Risk in Diabetes), ADVANCE (Action in Diabetes and Vascular
Disease: Preterax and Diamicron Modified Release Controlled Evaluation),
and VADT (Veterans Affairs Diabetes Trial)—which recruited older people
(mean age, 60-66 years) with type 2 diabetes duration of 8 to 11.5 years
and of whom 32% to 40% had a history of cardiovascular events, the
intensive-therapy group (HbA1c achieved, 6.4%-6.9%) showed no benefit in
the reduction of overall major cardiovascular events and death over 5
years of follow-up but only a lower rate of non-fatal myocardial
infarction in the ACCORD trial.50
51 52
53 Instead, there was higher
mortality in the intensive-therapy group of the ACCORD trial that led to
premature discontinuation of intensive therapy after 3.5 years of
follow-up. For the microvascular outcomes, the intensive-therapy group had
lowered macroalbuminuria by 30%, decreased progression of retinopathy by
33%, and a modest risk reduction in the development of peripheral
neuropathy.51 54 55 All of
these trials revealed that intensive therapy was associated with a higher
rate of hypoglycaemic episodes, with up to 2- to 3-fold increase in severe
hypoglycaemia. The findings imply that good glycaemic control is most
beneficial if it commences earlier, before the establishment of long-term
complications. Furthermore, it takes time for intensive glycaemic control
to reap microvascular benefit (over 5 years) and even longer for
macrovascular benefit (over 10-20 years).48
49 51
52 54
55 For patients with limited life
expectancy and multiple co-morbidities, the adverse effects are likely to
outweigh the benefits.
Individualised approach
The primary aim of diabetes management is to
optimise glycaemic control to avoid acute hyperglycaemia complications and
prevent long-term diabetic complications, both microvascular and
macrovascular, and to minimise the adverse effect of treatment-related
hypoglycaemia. Given the heterogeneous health status of older people,
diabetes intervention strategies designed for long-term benefits may not
be appropriate for all older people. A patient-centred approach for
diabetes management that takes account of the potential benefits and risks
of treatment, health and functional state, and social background for an
individual patient has been increasingly emphasised. Accordingly, various
frameworks or guidelines have been developed to assist in determining
glycaemic treatment goals in older diabetic patients.2 3 4 5 6 In general, for older people who are relatively young,
healthy and active, the same glycaemic target as for young people may be
worthwhile to prevent long-term complications. For frail older people with
multiple co-morbidities and limited life expectancy, the aim of glycaemic
control is to prevent acute hyperglycaemic complications (polyuria,
dehydration, hyperglycaemic hyperosmolar syndrome, infection, and poor
wound healing) while avoiding treatment adverse effects, rather than to
gain long-term benefit. The suggested target HbA1c varies from 7.0% to
7.5% for healthy older people to 8% to 9% for those who are in very poor
health.2 3
4 5
6 The choice of anti-glycaemic
agents should focus on safety, with low risk for hypoglycaemia, and
metformin is generally considered to be the first-line therapy for older
people.2 3
4 5
6 Avoidance of drugs with potential
adverse effects that may exacerbate underlying conditions such as heart
failure, osteoporosis with risk of fracture, and renal dysfunction is also
advised.
Restrictive diabetic diet
Because of altered taste and smell, anorexia of
ageing, difficulty in swallowing, and decreased functional state, food
intake tends to decline with advancing age. A restrictive diet for
glycaemic control that is designed for young and middle-aged diabetic
patients may not be suitable for all older diabetic patients.56 Instead, a restrictive diet may limit the variety and
flavour of food offered, which may exacerbate poor food intake leading to
unintentional weight loss and undernutrition. Those who are frail,
institutionalised, or underweight are particularly at risk, with increased
morbidity and mortality.57 Thus, a
less restrictive diet or even a liberal diet with modification of
medications to control blood glucose may be advisable for susceptible
patients.58 Nutritional assessment
taking account of a patient’s circumstances to guide individual
nutritional intervention is advocated.
Consensus statement for the management of older people
with diabetes
After the round-table discussion, consensus was
reached on the following six domains to address the management of older
diabetic people:
(1) When setting an individualised glycaemic goal, the important considerations should include:
(a) risk of hypoglycaemia;
(b) physical and mental function;
(c) co-morbidities and associated vascular disease; and
(d) family support and community resources.
(2) In view of the high risk of the associated co-morbidities with functional and cognitive impairment, use of an extended diabetic complication screening tool to include the geriatric syndromes is recommended. Other important reasons for screening include the close association of geriatric syndromes with diabetes, implications for choosing therapeutic interventions, and the considerable impact on quality of life. Common syndromes that could be included are:
(a) frailty;
(b) cognitive dysfunction;
(c) polypharmacy;
(d) nutrition;
(e) falls;
(f) hearing, visual impairment;
(g) depression;
(h) pain; and
(i) urinary incontinence.
(3) Because of the heterogeneous health status of older people, glucose and blood pressure targets should be individualised. An important consideration would be whether the time frame of potential benefits from treatment in long-term clinical trials is within the life expectancy of an individual patient:
(a) glycaemic target:
(i) HbA1c goal similar to that of general adults, but without excessive hypoglycaemia, should be considered for robust elderly people;
(ii) higher HbA1c up to 8.5% can be considered for those who are physically and cognitively frail or in nursing homes; and
(iii) liberal HbA1c without setting a target, aiming at symptomatic control, for those at the end of life.
(NB: HbA1c level would be potentially influenced by co-morbidities such as anaemia, which is more prevalent in older adults.)
(b) blood pressure target:
(i) similar to general adults (≤140/90 mm Hg) for robust elderly people;
(ii) ≤150/90 mm Hg for physically or cognitively frail elderly people, with avoidance of hypotension; and
(iii) liberal without setting a target for those at the end of life.
(4) In view of the risk of polypharmacy and the age-related changes in pharmacokinetics and pharmacodynamics, the following points need to be noted:
(a) when prescribing glucose-lowering agent(s), the major considerations should include:
(i) risk of hypoglycaemia;
(ii) dosing frequency and complexity of drug regimen;
(iii) tolerability and adverse effects such as gastrointestinal intolerance, change in fluid status, heart failure, fracture risk, weight change, and risk of urogenital infection;
(iv) glucose-lowering effect; and
(v) overall health status and quality of life of the patient.
(b) Choice of drugs:
(i) Metformin is generally chosen as a first-line agent because of robust clinical efficacy and low risk of hypoglycaemia. Its use is mainly limited by gastrointestinal tolerability, renal insufficiency, risk of lactic acidosis, and subclinical vitamin B12 deficiency.
(ii) Sulphonylureas are of low cost with high anti-glycaemic efficacy. However, they are associated with higher risk of hypoglycaemia and should be used with caution in older people. A long-acting sulphonylurea such as glibenclamide should be avoided because of the high incidence of prolonged hypoglycaemia and possibly increased mortality.
(iii) DPP-IV inhibitors have a low hypoglycaemia risk, modest clinical efficacy, good tolerability, and convenient dosing. The disadvantage is their higher cost.
(iv) Thiazolidinediones have low hypoglycaemia risk, and good efficacy and durability. The adverse effects include fluid retention, weight gain, and increased fractures. Lower doses are generally better tolerated.
(v) Sodium-glucose cotransporter 2 inhibitors have low hypoglycaemia risk, with decreased body weight, and modest clinical efficacy with some favourable cardiovascular safety data. Adverse effects include urogenital infection, urinary frequency, and dehydration. There may also be reduction of blood pressure so dose adjustment of any anti-hypertensive agent may be needed. They are of a higher cost with limited efficacy in patients with impaired renal function.
(vi) Alpha-glucosidase inhibitors have modest anti-glycaemic efficacy and low hypoglycaemic risk. Adverse effects include bloating, flatulence, and diarrhoea.
(vii) Glucagon-like peptide 1 agonists have low hypoglycaemia risk and good antiglycaemic efficacy with associated weight loss. The disadvantages are the high cost; the need for injections; and adverse effects of nausea, vomiting, and anorexia.
(viii) Insulins are highly effective in lowering glucose with various regimens. They are associated with significant hypoglycaemic risk and weight gain. The requirement for a high level of self-management education may be difficult for older people with physical or mental disabilities.
(5) A restrictive (therapeutic) diabetic diet may not be beneficial for some elderly diabetic people and may lead to decreased intake, unintentional weight loss, and undernutrition. Individualised nutritional approaches addressing personal food preferences and goals with a wider variety of food choices should be adopted. This is particularly applicable to those who are:
(a) >80 years old;
(b) physically frail;
(c) cognitively frail;
(d) underweight; and
(e) nursing home residents.
(6) Nursing home residents are distinct from community-dwelling older people because they are generally more frail with co-morbidities requiring high levels of care. The staff at long-term care facilities should be offered appropriate education and training in diabetes. The management of elderly nursing home residents with diabetes should aim to:
(a) prevent hypoglycaemia;
(b) prevent hospitalisation;
(c) avoid acute metabolic complications; and
(d) provide timely end-of-life care and advance care planning.
(1) When setting an individualised glycaemic goal, the important considerations should include:
(a) risk of hypoglycaemia;
(b) physical and mental function;
(c) co-morbidities and associated vascular disease; and
(d) family support and community resources.
(2) In view of the high risk of the associated co-morbidities with functional and cognitive impairment, use of an extended diabetic complication screening tool to include the geriatric syndromes is recommended. Other important reasons for screening include the close association of geriatric syndromes with diabetes, implications for choosing therapeutic interventions, and the considerable impact on quality of life. Common syndromes that could be included are:
(a) frailty;
(b) cognitive dysfunction;
(c) polypharmacy;
(d) nutrition;
(e) falls;
(f) hearing, visual impairment;
(g) depression;
(h) pain; and
(i) urinary incontinence.
(3) Because of the heterogeneous health status of older people, glucose and blood pressure targets should be individualised. An important consideration would be whether the time frame of potential benefits from treatment in long-term clinical trials is within the life expectancy of an individual patient:
(a) glycaemic target:
(i) HbA1c goal similar to that of general adults, but without excessive hypoglycaemia, should be considered for robust elderly people;
(ii) higher HbA1c up to 8.5% can be considered for those who are physically and cognitively frail or in nursing homes; and
(iii) liberal HbA1c without setting a target, aiming at symptomatic control, for those at the end of life.
(NB: HbA1c level would be potentially influenced by co-morbidities such as anaemia, which is more prevalent in older adults.)
(b) blood pressure target:
(i) similar to general adults (≤140/90 mm Hg) for robust elderly people;
(ii) ≤150/90 mm Hg for physically or cognitively frail elderly people, with avoidance of hypotension; and
(iii) liberal without setting a target for those at the end of life.
(4) In view of the risk of polypharmacy and the age-related changes in pharmacokinetics and pharmacodynamics, the following points need to be noted:
(a) when prescribing glucose-lowering agent(s), the major considerations should include:
(i) risk of hypoglycaemia;
(ii) dosing frequency and complexity of drug regimen;
(iii) tolerability and adverse effects such as gastrointestinal intolerance, change in fluid status, heart failure, fracture risk, weight change, and risk of urogenital infection;
(iv) glucose-lowering effect; and
(v) overall health status and quality of life of the patient.
(b) Choice of drugs:
(i) Metformin is generally chosen as a first-line agent because of robust clinical efficacy and low risk of hypoglycaemia. Its use is mainly limited by gastrointestinal tolerability, renal insufficiency, risk of lactic acidosis, and subclinical vitamin B12 deficiency.
(ii) Sulphonylureas are of low cost with high anti-glycaemic efficacy. However, they are associated with higher risk of hypoglycaemia and should be used with caution in older people. A long-acting sulphonylurea such as glibenclamide should be avoided because of the high incidence of prolonged hypoglycaemia and possibly increased mortality.
(iii) DPP-IV inhibitors have a low hypoglycaemia risk, modest clinical efficacy, good tolerability, and convenient dosing. The disadvantage is their higher cost.
(iv) Thiazolidinediones have low hypoglycaemia risk, and good efficacy and durability. The adverse effects include fluid retention, weight gain, and increased fractures. Lower doses are generally better tolerated.
(v) Sodium-glucose cotransporter 2 inhibitors have low hypoglycaemia risk, with decreased body weight, and modest clinical efficacy with some favourable cardiovascular safety data. Adverse effects include urogenital infection, urinary frequency, and dehydration. There may also be reduction of blood pressure so dose adjustment of any anti-hypertensive agent may be needed. They are of a higher cost with limited efficacy in patients with impaired renal function.
(vi) Alpha-glucosidase inhibitors have modest anti-glycaemic efficacy and low hypoglycaemic risk. Adverse effects include bloating, flatulence, and diarrhoea.
(vii) Glucagon-like peptide 1 agonists have low hypoglycaemia risk and good antiglycaemic efficacy with associated weight loss. The disadvantages are the high cost; the need for injections; and adverse effects of nausea, vomiting, and anorexia.
(viii) Insulins are highly effective in lowering glucose with various regimens. They are associated with significant hypoglycaemic risk and weight gain. The requirement for a high level of self-management education may be difficult for older people with physical or mental disabilities.
(5) A restrictive (therapeutic) diabetic diet may not be beneficial for some elderly diabetic people and may lead to decreased intake, unintentional weight loss, and undernutrition. Individualised nutritional approaches addressing personal food preferences and goals with a wider variety of food choices should be adopted. This is particularly applicable to those who are:
(a) >80 years old;
(b) physically frail;
(c) cognitively frail;
(d) underweight; and
(e) nursing home residents.
(6) Nursing home residents are distinct from community-dwelling older people because they are generally more frail with co-morbidities requiring high levels of care. The staff at long-term care facilities should be offered appropriate education and training in diabetes. The management of elderly nursing home residents with diabetes should aim to:
(a) prevent hypoglycaemia;
(b) prevent hospitalisation;
(c) avoid acute metabolic complications; and
(d) provide timely end-of-life care and advance care planning.
Conclusion
With the increasing population of older people with
diabetes and the complexity and heterogeneity of older people, it is time
to change our clinical practice in managing diabetes in older people—management should not be solely based on the clinical guidance for younger
people with diabetes. We need to consider the course of the disease in the
context of individual characteristics (co-morbidities, frailty, cognitive
impairment, life expectancy, risk of treatment-induced hypoglycaemia,
patients’ attitudes, social support, etc) to tailor a treatment goal and
management plan. This approach has recently been advocated by several
international organisations such as the American Diabetes Association and
the American Geriatrics Society. Our consensus statement takes the
initiative in promoting better diabetes care for older people in our
locality. The guidance takes into consideration of local experience to
address issues specifically related to older diabetic people, such as the
inclusion of a comprehensive geriatric assessment to screen for geriatric
syndromes and psychosocial needs, which is often missed in a busy clinic,
and the glycaemic targets for broadly classified groups of patients, which
could guide clinicians in daily practice. Nonetheless, the consensus
statement is far from complete in addressing all the issues—the details on
how to implement the geriatric assessment for optimal therapy, the
appropriate treatment goals for all the multifaceted scenarios of older
people, the optimal level of blood pressure control, and the allocation of
social support for care in the community and much more, remain to be
determined.
Appendices
Additional material related to this article can be
found on the HKMJ website. Please go to http://www.hkmj.org,
and search for the article.
Declaration
All authors have disclosed no conflicts of
interest.
References
1. McGhee SM, Cheung WL, Woo J, et al.
Trends of disease burden consequent to diabetes in older persons in Hong
Kong: implications of population ageing. Hong Kong SAR: Hong Kong Jockey
Club; 2009.
2. American Geriatrics Society Expert Panel
on Care of Older Adults with Diabetes Mellitus, Moreno G, Mangione CM,
Kimbro L, Vaisberg E. Guidelines abstracted from the American Geriatrics
Society Guidelines for Improving the Care of Older Adults with Diabetes
Mellitus: 2013 update. J Am Geriatr Soc 2013;61:2020-6. Crossref
3. Ismail-Beigi F, Moghissi E, Tiktin M,
Hirsch IB, Inzucchi SE, Genuth S. Individualizing glycemic targets in type
2 diabetes mellitus: implications of recent clinical trials. Ann Intern
Med 2011;154:554-9. Crossref
4. Sinclair A, Morley JE, Rodriguez-Mañas
L, et al. Diabetes mellitus in older people: position statement on behalf
of the International Association of Gerontology and Geriatrics (IAGG), the
European Diabetes Working Party for Older People (EDWPOP), and the
International Task Force of Experts in Diabetes. J Am Med Dir Assoc
2012;13:497-502. Crossref
5. Inzucchi SE, Bergenstal RM, Buse JB, et
al. Management of hyperglycemia in type 2 diabetes: a patient-centered
approach: position statement of the American Diabetes Association (ADA)
and the European Association for the Study of Diabetes (EASD). Diabetes
Care 2012;35:1364-79. Crossref
6. Kirkman MS, Briscoe VJ, Clark N, et al.
Diabetes in older adults: a consensus report. J Am Geriatr Soc
2012;60:2342-56. Crossref
7. Inzucchi SE, Bergenstal RM, Buse JB, et
al. Management of hyperglycemia in type 2 diabetes, 2015: A
patient-centered approach: update to a position statement of American
Diabetes Association and the European Association for the Study of
Diabetes. Diabetes Care 2015;38:140-9. Crossref
8. Shorr RI, Ray WA, Daugherty JR, Griffin
MR. Incidence and risk factors for serious hypoglycemia in older persons
using insulin or sulfonylureas. Arch Intern Med 1997;157:1681-6. Crossref
9. Bremer JP, Jauch-Chara K, Hallschmid M,
Schmid S, Schultes B. Hypoglycemia unawareness in older compared with
middle-aged patients with type 2 diabetes. Diabetes Care
2009;32:1513-7. Crossref
10. Brierley EJ, Broughton DL, James OF,
Alberti KG. Reduced awareness of hypoglycaemia in the elderly despite an
intact counter-regulatory response. QJM 1995;88:439-45.
11. Meneilly GS, Cheung E, Tuokko H.
Altered responses to hypoglycemia of healthy elderly people. J Clin
Endocrinol Metab 1994;78:1341-8. Crossref
12. Matyka K, Evans M, Lomas J, Cranston
I, Macdonald I, Amiel SA. Altered hierarchy of protective responses
against severe hypoglycemia in normal aging in healthy men. Diabetes Care
1997;20:135-41. Crossref
13. White NH, Skor DA, Cryer PE,
Levandoski LA, Bier DM, Santiago JV. Identification of type I diabetic
patients at increased risk for hypoglycemia during intensive therapy. N
Engl J Med 1983;308:485-91. Crossref
14. Gold AE, Macleod KM, Frier BM,
Frequency of severe hypoglycemia in patients with type I diabetes with
impaired awareness of hypoglycemia. Diabetes Care 1994;17:697-703. Crossref
15. Cukierman T, Gerstein HC, Williamson
JD. Cognitive decline and dementia in diabetes—systematic overview of
prospective observational studies. Diabetologia 2005;48:2460-9. Crossref
16. Lu FP, Lin KP, Kuo HK. Diabetes and
the risk of multi-system aging phenotypes: a systematic review and
meta-analysis. PLoS One 2009;4:e4144. Crossref
17. Whitmer RA, Karter AJ, Yaffe K,
Quesenberry CP Jr, Selby JV. Hypoglycemic episodes and risk of dementia in
older patients with type 2 diabetes mellitus. JAMA 2009;301:1565-72. Crossref
18. Lin CH, Sheu WH. Hypoglycaemic
episodes and risk of dementia in diabetes mellitus: 7-year follow-up
study. J Intern Med 2013;273:102-10. Crossref
19. Aung PP, Strachan MW, Frier BM, et al.
Severe hypoglycaemia and late-life cognitive ability in older people with
type 2 diabetes: the Edinburgh Type 2 Diabetes Study. Diabet Med
2012;29:328-36. Crossref
20. Yaffe K, Falvey CM, Hamilton N, et al.
Association between hypoglycemia and dementia in a biracial cohort of
older adults with diabetes mellitus. JAMA Intern Med
2013;173:1300-6. Crossref
21. Nouwen A, Winkley K, Twisk J, et al.
Type 2 diabetes mellitus as a risk factor for the onset of depression: a
systematic review and meta-analysis. Diabetologia 2010;53:2480-6. Crossref
22. Mezuk B, Eaton WW, Albrecht S, Golden
SH. Depression and type 2 diabetes over the lifespan: a meta-analysis.
Diabetes Care 2008;31:2383-90. Crossref
23. Li C, Ford ES, Zhao G, Ahluwalia IB,
Pearson WS, Mokdad AH. Prevalence and correlates of undiagnosed depression
among U.S. adults with diabetes: the Behavioral Risk Factor Surveillance
System, 2006. Diabetes Res Clin Pract 2009;83:268-79. Crossref
24. Brown AF, Mangione CM, Saliba D,
Sarkisian CA; California Healthcare Foundation/American Geriatrics Society
Panel on Improving Care for Elders with Diabetes. Guidelines for improving
the care of the older person with diabetes mellitus. J Am Geriatr Soc
2003;51(5 Suppl Guidelines):S265-80.
25. Holstein A, Plaschke A, Egberts EH.
Clinical characterisation of severe hypoglycaemia—a prospective
population-based study. Exp Clin Endocrinol Diabetes 2003;111:364-9. Crossref
26. Huang ES, Karter AJ, Danielson KK,
Warton EM, Ahmed AT. The association between the number of prescription
medications and incident falls in a multi-ethnic population of adult
type-2 diabetes patients: the diabetes and aging study. J Gen Intern Med
2010;25:141-6. Crossref
27. Maher RL, Hanlon J, Hajjar ER.
Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf
2014;13:57-65. Crossref
28. Mayne D, Stout NR, Aspray TJ.
Diabetes, falls and fractures. Age Ageing 2010;39:522-5. Crossref
29. Bauman WA, Shaw S, Jayatilleke E,
Spungen AM, Herbert V. Increase intake of calcium reverses vitamin B12
malabsorption induced by metformin. Diabetes Care 2000;23:1227-31. Crossref
30. Schneider AL, Williams EK, Brancati
FL, Blecker S, Coresh J, Selvin E. Diabetes and risk of fracture-related
hospitalization: the Atherosclerosis Risk in Communities Study. Diabetes
Care 2013;36:1153-8. Crossref
31. Loke YK, Singh S, Furberg CD.
Long-term use of thiazolidinediones and fractures in type 2 diabetes: a
meta-analysis. CMAJ 2009;180:32-9. Crossref
32. Ivers RQ, Cumming RG, Mitchell P,
Peduto AJ; Blue Mountains Eye Study. Diabetes and risk of fracture: The
Blue Mountains Eye Study. Diabetes Care 2001;24:1198-203. Crossref
33. Abbott CA, Malik RA, van Ross ER,
Kulkarni J, Boulton AJ. Prevalence and characteristics of painful diabetic
neuropathy in a large community-based diabetic population in the U.K.
Daibetes Care 2011;34:2220-4. Crossref
34. Brown JS, Vittinghoff E, Lin F, Nyberg
LM, Kusek JW, Kanaya AM. Prevalence and risk factors for urinary
incontinence in women with type 2 diabetes and impaired fasting glucose:
findings from the National Health and Nutrition Examination Survey
(NHANES) 2001-2002. Diabetes Care 2006;29:1307-12. Crossref
35. AGS Panel on Persistent Pain in Older
Persons. The management of persistent pain in older persons. J Am Geriatr
Soc 2002;50(6 Suppl):S205-24.
36. Brown JS, Vittinghoff E, Wyman JF, et
al. Urinary incontinence: does it increase risk for falls and fracture? J
Am Geriatr Soc 2000;48:721-5. Crossref
37. Dugan E, Cohen SJ, Bland DR, et al.
The association of depressive symptoms and urinary incontinence among
older adults. J Am Geriatr Soc 2000:48:413-6. Crossref
38. Wolff JL, Starfield B, Anderson G.
Prevalence, expenditures, and complications of multiple chronic conditions
in the elderly. Arch Intern Med 2002;162:2269-76. Crossref
39. Greenfield S, Billmek J, Pellegrini F,
et al. Comorbidity affects the relationship between glycemic control and
cardiovascular outcomes in diabetes: a cohort study. Ann Intern Med
2009;151:854-60. Crossref
40. Goto A, Arah OA, Goto M, Terauchi Y,
Noda M. Severe hypoglycaemia and cardiovascular disease: systematic review
and meta-analysis with bias analysis. BMJ 2013;347:f4533. Crossref
41. Desouza C, Salazar H, Cheong B, Murgo
J, Fonseca V. Association of hypoglycemia and cardiac ischemia: a study
based on continuous monitoring. Diabetes Care 2003;26:1485-9. Crossref
42. Anderson RJ, Bahn GD, Moritz TE, et
al. Blood pressure and cardiovascular disease risk in the Veterans Affairs
Diabetes Trial. Diabetes Care 2011;34:34-8. Crossref
43. Curb JD, Pressel SL, Cutler JA, et al.
Effect of diuretic-based antihypertensive treatment on cardiovascular
disease risk in older diabetic patients with isolated systolic
hypertension. Systolic Hypertension in the Elderly Program Cooperative
Research Group. JAMA 1996;276:1886-92. Crossref
44. Tight blood pressure control and risk
of macrovascular and microvascular complications in type 2 diabetes: UKPDS
38. UK Prospective Diabetes Study Group. BMJ 1998:317:703-13. Crossref
45. Cooper-DeHoff RM, Gong Y, Handberg EM,
et al. Tight blood pressure control and cardiovascular outcomes among
hypertensive patients with diabetes and coronary artery disease. JAMA
2010;304:61-8. Crossref
46. Sleight P, Redon J, Verdecchia P, et
al. Prognostic value of blood pressure in patients with high vascular risk
in the Ongoing Telmisartan Alone and in combination with Ramipril Global
Endpoint Trial study. J Hypertens 2009;27:1360-9. Crossref
47. Baigent C, Keech A, Kearney PM, et al.
Efficacy and safety of cholesterol-lowering treatment: prospective
metaanalysis of data from 90,056 participants in 14 randomised trials of
statins. Lancet 2005;366:1267-78. Crossref
48. Intensive blood-glucose control with
sulphonylureas or insulin compared with conventional treatment and risk of
complications in patients with type 2 diabetes (UKPDS 33). UK Prospective
Diabetes Study (UKPDS) Group. Lancet 1998;352:837-53. Crossref
49. Holman RR, Paul SK, Bethel MA,
Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in
type 2 diabetes. N Engl J Med 2008;359:1577-89. Crossref
50. Action to Control Cardiovascular Risk
in Diabetes Study Group, Gerstein HC, Miller ME, Byington RP, et al.
Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med
2008;358:2545-59. Crossref
51. ADVANCE Collaborative Group, Patel A,
MacMahon S, Chalmers J, et al. Intensive blood glucose control and
vascular outcomes in patients with type 2 diabetes. N Engl J Med
2008;358:2560-72. Crossref
52. Duckworth W, Abraira C, Moritz T, et
al. Glucose control and vascular complications in veterans with type 2
diabetes. N Engl J Med 2009;360:129-39. Crossref
53. ACCORD Study Group, Gerstein HC,
Miller ME, Genuth S, et al. Long-term effects of intensive glucose
lowering on cardiovascular outcomes. N Engl J Med 2011;364:818-28. Crossref
54. Ismail-Beigi F, Craven T, Banerji MA,
et al. Effect of intensive treatment of hyperglycaemia on microvascular
outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial.
Lancet 2010;376:419-30. Crossref
55. ACCORD Study Group; ACCORD Eye Study
Group, Chew EY, Ambrosius WT, Davis MD, et al. Effects of medical
therapies on retinopathy progression in type 2 diabetes. N Engl J Med
2010;363:233-44. Crossref
56. Dorner B, Friedrich EK, Posthauer ME;
American Dietetic Association. Position of the American Dietetic
Association: individualized nutrition approaches for older adults in
health care communities. J Am Diet Assoc 2010;110:1549-53. Crossref
57. Schafer RG, Bohannon B, Franz MJ, et
al. Diabetes nutrition recommendations for health care institutions.
Diabetes Care 2004;27 Suppl 1:S55-7. Crossref
58. American Diabetes Association, Bantle
JP, Wylie-Rosett J, Albright AL, et al. Nutrition recommendations and
interventions for diabetes: a position statement of the American Diabetes
Association. Diabetes Care 2008;31 Suppl 1:S61-78.

