Hong Kong Med J 2017 Oct;23(5):441–5 | Epub 27 Jan 2017
DOI: 10.12809/hkmj164984
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Intravenous lignocaine infusion facilitates acute
rehabilitation after laparoscopic colectomy in the
Chinese patients
Matthew WH Lee, MB, ChB1;
Debriel YL Or, FHKAM (Anaesthesiology)2;
Alex CF Tsang, FHKAM (Surgery)3;
Dennis CK Ng, FHKAM (Surgery)3;
PP Chen, FHKAM (Anaesthesiology)2;
Michael HY Cheung, FHKAM (Surgery)3;
Raymond SK Li, FHKAM (Surgery)3;
HT Leong, FHKAM (Surgery)3
1 Department of Orthopaedics, Queen Elizabeth Hospital, Jordan, Hong Kong
2 Department of Anaesthesiology and Operating Service, North District
Hospital, Sheung Shui, Hong Kong
3 Department of Surgery, North District Hospital, Sheung Shui, Hong Kong
Corresponding author: Dr Alex CF Tsang (alextsang81@yahoo.com)
Abstract
Introduction: Intravenous infusion of lignocaine
has emerged in recent years as a feasible, cost-effective,
and safe method to provide postoperative
analgesia. There is, however, no literature about this
perioperative pain control modality in Chinese
patients. This study aimed to determine whether
perioperative intravenous lignocaine safely reduces
postoperative pain, shortens postoperative ileus, and
reduces the length of hospital stay in laparoscopic
colorectal surgery.
Methods: Between September 2012 and May 2015,
16 patients who underwent elective laparoscopic
resection of colorectal cancer and received a 1%
lignocaine infusion for 24 hours postoperatively were
studied. After surgery, categorical pain scores were
obtained immediately, followed by hourly pain scores
at rest. Pain scores at rest and with mobilisation,
and patient satisfaction score were documented on
postoperative day 1. Return of bowel function was
measured by time of first flatus and bowel opening.
The patient’s rehabilitation was assessed by time
taken to tolerate diet, full mobilisation, and length
of hospital stay.
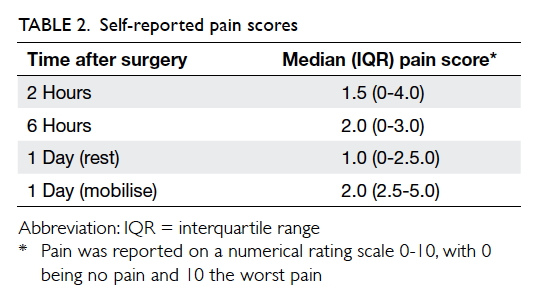
Results: The median (interquartile range) self-reported
pain scores at 2 hours and 6 hours after
surgery were 1.5 (0-4) and 2 (0-3), respectively.
The median pain scores at rest and mobilisation
on postoperative day 1 were 1 (0-2.5) and 2 (2.5-5),
respectively, with a median satisfaction score of 7.5
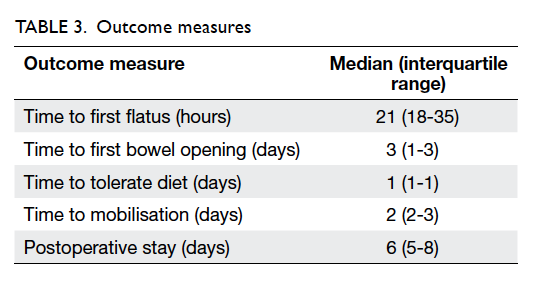
(7-9). The median times to first flatus and first bowel
opening were 21 (18-35) hours and 3 (1-3) days,
respectively. No patient had postoperative ileus. The
median times to tolerating diet and mobilisation were
1 (1-1) day and 2 (2-3) days, respectively. The median
postoperative stay was 6 (5-8) days.
Conclusions: Intravenous lignocaine is a safe
and effective postoperative analgesic in a Chinese
population. It enhances the rehabilitation process
for patients following laparoscopic resection of
colorectal cancer.
New knowledge added by this study
- This is the first case series in Hong Kong to show that intravenous lignocaine infusion is safe in a Chinese population as postoperative analgesia. Clinical safety and effectiveness was positive in this study.
- Intravenous infusion of lignocaine can help to enhance postoperative recovery for patients following laparoscopic resection of colorectal cancer. Large-scale structured studies should be carried out to confirm these findings.
Introduction
Over the past couple of decades, there has been
a move towards fast-track surgery designed to
reduce postoperative morbidities and length of
hospital stay.1 Laparoscopic methods for colonic
surgery have accelerated postoperative recovery
by reducing the time required for bowel function
recovery and enhancing postoperative mobilisation.2
Postoperative ileus, however, remains a common
reason for prolonged hospital stay following major
abdominal surgery. Although its pathophysiology
is multifactorial, use of opioids as postoperative
analgesia is thought to contribute to the problem.3 4 Therefore, safe and effective postoperative pain
control with minimal use of opioids is essential to
enhance recovery.5
The advantages of continuous infusion of
thoracic epidural analgesia (TEA) compared with
intravenous (IV) patient-controlled analgesia with
opioid have been studied. The results show that TEA
significantly improves early analgesia requirement
following laparoscopic colectomy with an opioid-sparing
effect. Nonetheless TEA is associated with
other adverse reactions such as urinary retention,
hypotension, epidural haematoma, and abscess
formation.6 Intravenous infusion of lignocaine
has emerged in recent years as a feasible, cost-effective,
and safe method to provide postoperative
analgesia.7 Recent randomised controlled trials
have shown that the combined analgesic, anti-inflammatory,
and antihyperalgesic properties
of IV lignocaine improve outcomes and shorten
hospital stay following colorectal surgery.8 There
is level I (PRISMA: Preferred Reporting Items for
Systematic Reviews and Meta-Analyses) evidence
that IV lignocaine infusions are opioid-sparing and
significantly reduce pain scores at rest and during
activity, nausea, vomiting, duration of ileus after
abdominal surgery, and length of hospital stay. Peri-operative
IV administration of lignocaine also has a
preventive analgesic effect following a wide range of
operations.9 10 11
Currently there is no literature about this
perioperative pain control modality in the Chinese
patients. In the following account, we present a
case series of Chinese patients who underwent
laparoscopic colorectal surgery and received a peri-operative
IV lignocaine infusion.
Methods
We reviewed cases of patients who underwent
elective laparoscopic resection of colorectal cancer
and received a lignocaine infusion as postoperative
analgesia between September 2012 and May 2015 at
North District Hospital in Hong Kong. This study aimed to determine whether postoperative
IV lignocaine infusion would provide adequate
analgesia, shorten the duration of postoperative
ileus, reduce postoperative complications, enhance
rehabilitation, and shorten hospital stay. This study was done in accordance with the principles outlined in the Declaration of Helsinki.
Anaesthesia
All patients were assessed preoperatively by an
anaesthetist to exclude any contra-indications to use
of IV lignocaine. Routine consent for anaesthesia was
obtained with clear choices offered for postoperative
analgesia and the relevant risks explained to the
patient. The choices for postoperative analgesia
included epidural analgesia, IV lignocaine infusion,
and IV patient-controlled analgesia with morphine.
Intravenous lignocaine was offered when patients
refused or were contra-indicated for epidural
analgesia. If patients were not suitable for either
epidural analgesia or IV lignocaine, IV patient-controlled
analgesia with morphine was offered.
The anaesthetic technique was standardised for all
patients.
All patients received an IV bolus injection of
lignocaine 1.5 mg/kg over 20 minutes on induction
followed by a continuous infusion of 1.5 mg/kg/h
intra-operatively. The 1% lignocaine infusion
was continued at a rate of 1 mg/kg/h for 24 hours
postoperatively, delivered through a GemStar
infusion device with the fixed calculated dose set
up by the case anaesthetist. For safety reasons, the
lignocaine infusion was connected to a dedicated IV
line to avoid accidental bolus administration. General
anaesthesia was induced with fentanyl 1-2 µg/kg,
propofol 2-3 mg/kg, and cisatracurium 0.15-0.2
mg/kg for intubation. Anaesthesia was maintained
with oxygen in room air or nitrous oxide and
isoflurane or sevoflurane at an end-tidal anaesthetic
concentration of approximately 1 minimal alveolar
concentration. Ketorolac 15-30 mg was administered
on induction if not contra-indicated clinically.
Intravenous tramadol 50-100 mg and morphine
was used intra-operatively for analgesia as decided
by the list anaesthetist. Wound infiltration of local
anaesthetic, 0.25% levobupivacaine 20 mL, was
administered by the surgeon at the end of surgery.
Surgical procedure
Patients who had colorectal cancer and underwent
elective laparoscopic colorectal resection were
recruited into the study. All patients had colorectal
cancer but the surgical procedure performed
depended on the location of the tumour and the
international standard. The surgeries included:
laparoscopic right hemicolectomy (n=2),
laparoscopic left hemicolectomy (n=3), laparoscopic
sigmoidectomy (n=5), laparoscopic anterior
resection of rectum (n=1), laparoscopic lower
anterior resection with total mesorectal excision
and stoma formation (n=4), and laparoscopic
abdominoperineal resection (n=1). All patients
had four to five small incisions for the laparoscopic
procedure together with one larger 6- to 8-cm
abdominal incision for specimen retrieval. For
the patient with laparoscopic abdominoperineal
resection, a larger wound for specimen retrieval
was made over the perineal region instead of the
abdomen.
Postoperative analgesia
All patients were prescribed regular oral paracetamol
500 mg to 1 g 3 to 4 times per day. Regular oral
diclofenac SR 100 mg daily for 3 days was prescribed
if not contra-indicated. As required, IV tramadol
50 mg every 6 to 8 hours was given if pain was
not adequately controlled. Rescue subcutaneous
morphine was prescribed in the protocol for severe
uncontrolled pain.
Outcome measures
All postoperative data were collected prospectively.
The acute pain service and ward nurses followed the
clinical plan that was devised by both the surgical
and pain team.
After surgery, a categorical pain score (divided
into none, mild, moderate, or severe pain) was
obtained immediately in the postoperative care unit
by recovery nurses. After the patient was discharged
to the ward, pain scores were obtained by ward nurses
on a numerical rating scale at rest hourly for 24 hours
until lignocaine infusion was stopped. Patients would
be reviewed by acute pain management team before
lignocaine infusion was stopped and pain scores on
postoperative day 1 were obtained at rest and during
mobilisation. The numerical rating scale scored pain
from 0 to 10 with 0 being no pain and 10 being the
worst pain imaginable. Pain scores are continuous
variables and are presented as median (interquartile
range [IQR]) scores against time. Patient satisfaction
score from 0 to 10 was also assessed by the acute
pain management team. The presence of nausea,
vomiting, dizziness, and other possible side-effects
was documented. Intra-operative and postoperative
analgesic consumption was recorded. All patients
were monitored by cardiac monitor intra-operatively
by anaesthetists and postoperatively in the recovery
room by nurses. When patients were discharged to
the ward, they were monitored for the next 24 hours
until the end of IV lignocaine infusion with vital signs
recorded every hour, including blood pressure, pulse,
saturation, and continuous cardiac monitoring.
There was no recorded cardiac arrhythmia event
noted for any patient.
Return of bowel function was assessed by
calculating the time from end of surgery to the
passage of first flatus and first bowel opening.
Postoperative rehabilitation was assessed by the time
taken to tolerate diet and achieve full mobilisation
and the length of hospital stay. These data are
expressed as median (IQR) scores.
Results
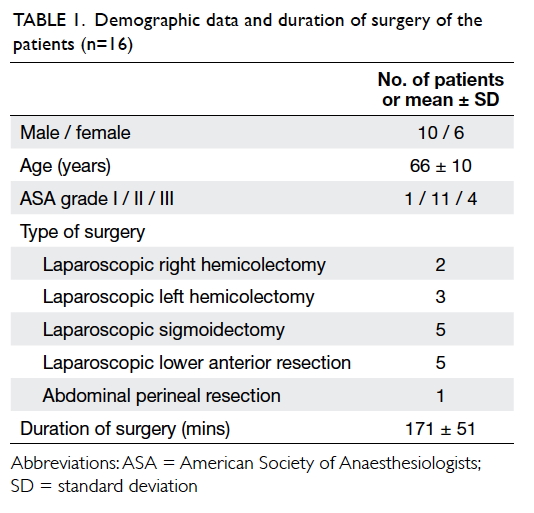
Sixteen patients were studied with a mean (±
standard deviation) age of 66 ± 10 years. All were
classified as American Society of Anesthesiologists
grade I to III. Demographic data and duration of
surgery are shown in Table 1.
During IV lignocaine infusion, four patients
experienced nausea, one vomited, and two
complained of mild dizziness. No serious adverse
reactions were reported. All patients tolerated and
completed the infusion of lignocaine.
In the postoperative care unit, most patients
experienced none or mild pain. Only one patient
complained of severe pain and required a fentanyl
bolus for rescue analgesia. The self-reported pain
scores are shown in Table 2. In addition to regular
paracetamol, five patients requested IV tramadol for
rescue analgesia in the first 24 hours postoperatively;
these patients received tramadol 50-150 mg. No
patient requested morphine during the first 24
hours postoperatively. Of the 16 patients, 11 showed
overall satisfaction with the analgesia with median
satisfaction score of 7.5 (7-9).
As seen in Table 3, the median times to first flatus
and first bowel opening in the postoperative period
were 21 (18-35) hours and 3 (1-3) days, respectively.
The median times to tolerating diet and mobilisation were 1
(1-1) day and 2 (2-3) days, respectively. No patient
had postoperative ileus. Only one patient had acute
retention of urine that delayed discharge from
hospital. Three other patients had a prolonged
hospital stay due to social problems.
There was no documented postoperative
arrhythmia for any patient.
Discussion
Although this is a small case-series review, we have
shown that lignocaine infusion is a safe and feasible
means of postoperative pain control for patients
undergoing laparoscopic colorectal resection. There
was no major or serious adverse reaction such as
cardiac arrhythmia during the lignocaine infusion.
We also demonstrated that lignocaine infusion
provided effective analgesia over the first 24 hours
with acceptable pain score, low rescue opioid
consumption, and good patient satisfaction score. Our
results are consistent with the literature. Harvey et al12 observed that pain scores were decreased when a lignocaine infusion was administered compared with
a group who received IV infusion of normal saline.
Kaba et al13 also demonstrated that their lignocaine
group required 50% less opioid during the first 24
hours postoperatively. Similar results were reported
in other randomised controlled trials demonstrating
that IV lignocaine has an opioid-sparing effect as
an adjuvant analgesic.7 14 A recent meta-analysis by McCarthy et al15 examined the overall efficacy of IV
lignocaine on postoperative analgesia and recovery
from surgery in patients undergoing various surgical
procedures. It concluded that IV lignocaine infusion
in the perioperative period has clear advantages in
patients undergoing abdominal surgery in terms of
both pain control and bowel motility.
Our study also observed that IV lignocaine
resulted in rapid recovery of bowel function and
mobilisation. The median time for return of flatus
and ability to tolerate an oral diet was within 24
hours. The median (IQR) time for bowel opening
was 3 (1-3) days. These results are similar
to the findings of Kaba et al13 who showed that
lignocaine infusion improved postoperative bowel
function. In that study, defaecation occurred almost
1 day earlier in the lignocaine group compared with
the group who received normal saline. The reasons
for postoperative ileus are multifactorial, including
use of opioid analgesia, the sympathetic response,
and visceral inflammatory response resulting from
surgery.16 A lignocaine infusion may shorten the
time to bowel opening by decreasing opioid use,
limiting the inflammatory response, and having a
direct inhibitory effect on the sympathetic nervous
system of the mesenteric nervous plexus resulting in
enhanced bowel contractility.17
A meta-analysis showed that continuous IV
administration of lignocaine significantly reduces
the length of hospital stay when compared with
controls.17 In our study, however, the median hospital
stay was 6 days, similar to our usual experience. We
are evaluating the possible reasons for the lack of
impact on hospital stay. One of the reasons may be
related to patient expectations and preference for
a longer hospital stay after major surgery. Another
possible reason is the similar rehabilitation care
pathway for the two groups of patients that when
strictly followed tended to negate the advantages of
IV lignocaine.
Conclusions
This review shows promising results demonstrating
that IV lignocaine is a safe and effective postoperative
analgesia in a Chinese population. It also provides
comparable outcomes to those reported worldwide
that postoperative lignocaine can provide a beneficial
rehabilitation effect for patients who have undergone
laparoscopic colorectal surgery. This provides a
good platform from which to design a randomised
controlled trial in the Chinese population.
Declaration
The authors declared no conflicts of interest in this study.
References
1. Kehlet H, Dahl JB. Anaesthesia, surgery, and challenges in
postoperative recovery. Lancet 2003;362:1921-8. Crossref
2. Reza MM, Blasco JA, Andradas E, Cantero R, Mayol J.
Systematic review of laparoscopic versus open surgery for
colorectal cancer. Br J Surg 2006;93:921-8. Crossref
3. Baig MK, Wexner SD. Postoperative ileus: a review. Dis
Colon Rectum 2004;47:516-26. Crossref
4. Taguchi A, Sharma N, Saleem RM, et al. Selective
postoperative inhibition of gastrointestinal opioid
receptors. N Engl J Med 2001;345:935-40. Crossref
5. Kuhry E, Schwenk W, Gaupset R, Romild U, Bonjer J.
Long-term outcome of laparoscopic surgery for colorectal
cancer: a cochrane systematic review of randomized
controlled trials. Cancer Treat Rev 2008;34:498-504. Crossref
6. Senagore AJ, Delaney CP, Mekhail N, Dugan A, Fazio VW.
Randomized clinical trial comparing epidural anaesthesia
and patient-controlled analgesia after laparoscopic
segmental colectomy. Br J Surg 2003;90:1195-9. Crossref
7. Koppert W, Weigand M, Neumann F, et al. Perioperative
intravenous lidocaine has preventive effects on
postoperative pain and morphine consumption after major
abdominal surgery. Anesth Analg 2004;98:1050-5. Crossref
8. Herroeder S, Pecher S, Schönherr ME, et al. Systemic
lidocaine shortens length of hospital stay after colorectal
surgery: a double-blinded, randomized, placebo-controlled
trial. Ann Surg 2007;246:192-200. Crossref
9. Vigneault L, Turgeon AF, Côté D, et al. Perioperative
intravenous lignocaine infusion for postoperative pain
control: a meta-analysis of randomized control trials. Can J
Anaesth 2011;58:22-37. Crossref
10. Sun Y, Li T, Wang N, Yun Y, Gan TJ. Perioperative systemic
lidocaine for postoperative analgesia and recovery after
abdominal surgery: a meta-analysis of randomized control
trials. Dis Colon Rectum 2012;55:1183-94. Crossref
11. Barreveld A, Witte J, Chahal H, Durieux ME, Strichartz
G. Preventive analgesia by local anesthetics: the reduction
of postoperative pain by peripheral nerve blocks and
intravenous drugs. Anesth Analg 2013;116:1141-61. Crossref
12. Harvey KP, Adair JD, Isho M, Robinson R. Can intravenous
lidocaine decrease postsurgical ileus and shorten hospital
stay in elective bowel surgery? A pilot study and literature
review. Am J Surg 2009;198:231-6. Crossref
13. Kaba A, Laurent SR, Detroz BJ, et al. Intravenous lidocaine
infusion facilitates acute rehabilitation after laparoscopic
colectomy. Anesthesiology 2007;106:11-8. Crossref
14. Groudine SB, Fisher HA, Kaufman RP Jr, et al. Intravenous
lidocaine speeds the return of bowel function, decreases
postoperative pain, and shortens hospital stay in patients
undergoing radical retropubic prostatectomy. Anesth
Analg 1998;86:235-9. Crossref
15. McCarthy GC, Megalla SA, Habib AS. Impact of
intravenous lidocaine infusion on postoperative analgesia
and recovery from surgery: a systematic review of
randomized controlled trials. Drugs 2010;70:1149-63. Crossref
16. Luckey A, Livingston E, Taché Y. Mechanisms and
treatment of postoperative ileus. Arch Surg 2003;138:206-14. Crossref
17. Marret E, Rolin M, Beaussier M, Bonnet F. Meta-analysis
of intravenous lidocaine and postoperative recovery after
abdominal surgery. Br J Surg 2008;95:1331-8. Crossref