Hong Kong Med J 2017 Aug;23(4):416.e1–3
DOI: 10.12809/hkmj164918
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
A child with giant tumefactive perivascular spaces
Neeraj R Mahboobani, MB, BS, FRCR; LF Cheng, FRCR, FHKAM (Radiology); Johnny KF Ma, FRCR, FHKAM (Radiology)
Department of Radiology, Princess Margaret Hospital, Laichikok, Hong Kong
Corresponding author: Dr Neeraj R Mahboobani (neeraj.mahboobani@gmail.com)
A 4-year-old girl was admitted with a 2-day history
of a high temperature up to 41°C. She developed
sudden-onset generalised tonic-clonic seizure. She
had no travel history. Physical examination showed
neck stiffness. The working diagnosis was meningitis.
Non-contrast computed tomographic (CT) brain
prior to lumbar puncture revealed clustered
well-defined cystic lesions with no calcifications
measuring up to 1.5 cm in the white matter of the
right frontal and parietal lobes (Fig 1).
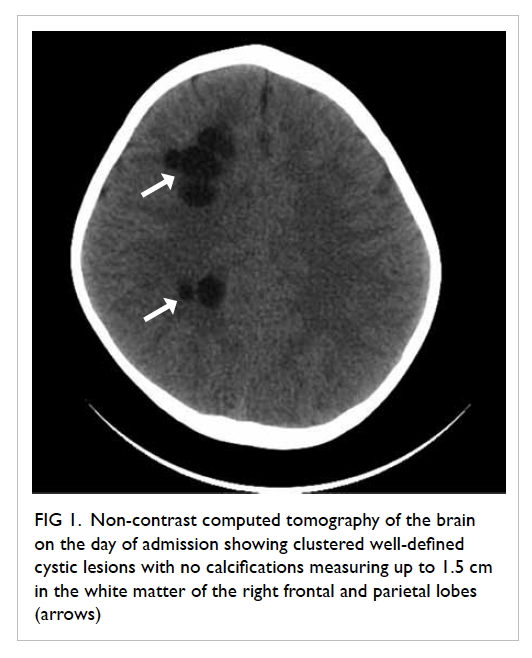
Figure 1. Non-contrast computed tomography of the brain on the day of admission showing clustered well-defined cystic lesions with no calcifications measuring up to 1.5 cm in the white matter of the right frontal and parietal lobes (arrows)
The child subsequently developed status
epilepticus. The neurosurgical unit was consulted
and brain abscesses were suspected. In view of her
clinical deterioration, burr hole and aspiration of the
cystic lesions were planned after magnetic resonance
imaging (MRI). The signal intensity of the lesions
was identical to that of cerebrospinal fluid (CSF) on
all MRI sequences (Figs 2 and 3). There was no rim enhancement
around the lesions. Minimal fluid-attenuated
inversion recovery (FLAIR) hyperintense
signals were noted in the white matter adjacent to
the lesions. There was no restricted diffusion on
diffusion-weighted imaging.
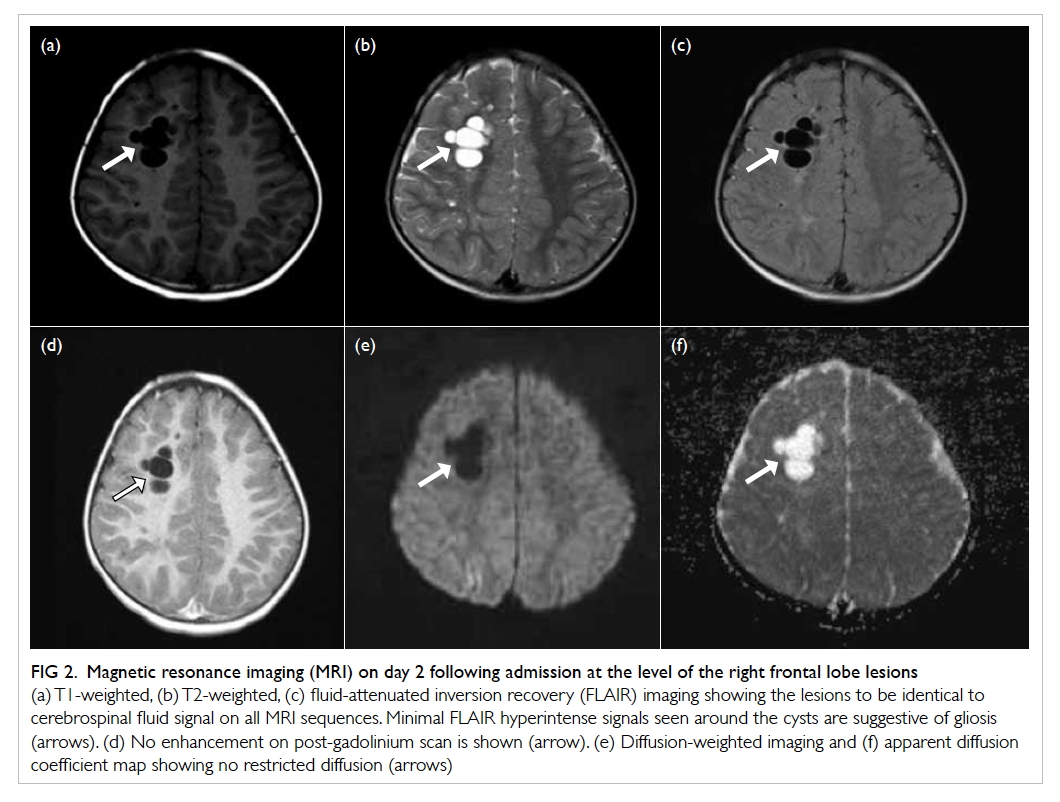
Figure 2. Magnetic resonance imaging (MRI) on day 2 following admission at the level of the right frontal lobe lesions
(a) T1-weighted, (b) T2-weighted, (c) fluid-attenuated inversion recovery (FLAIR) imaging showing the lesions to be identical to cerebrospinal fluid signal on all MRI sequences. Minimal FLAIR hyperintense signals seen around the cysts are suggestive of gliosis (arrows). (d) No enhancement on post-gadolinium scan is shown (arrow). (e) Diffusion-weighted imaging and (f) apparent diffusion coefficient map showing no restricted diffusion (arrows)
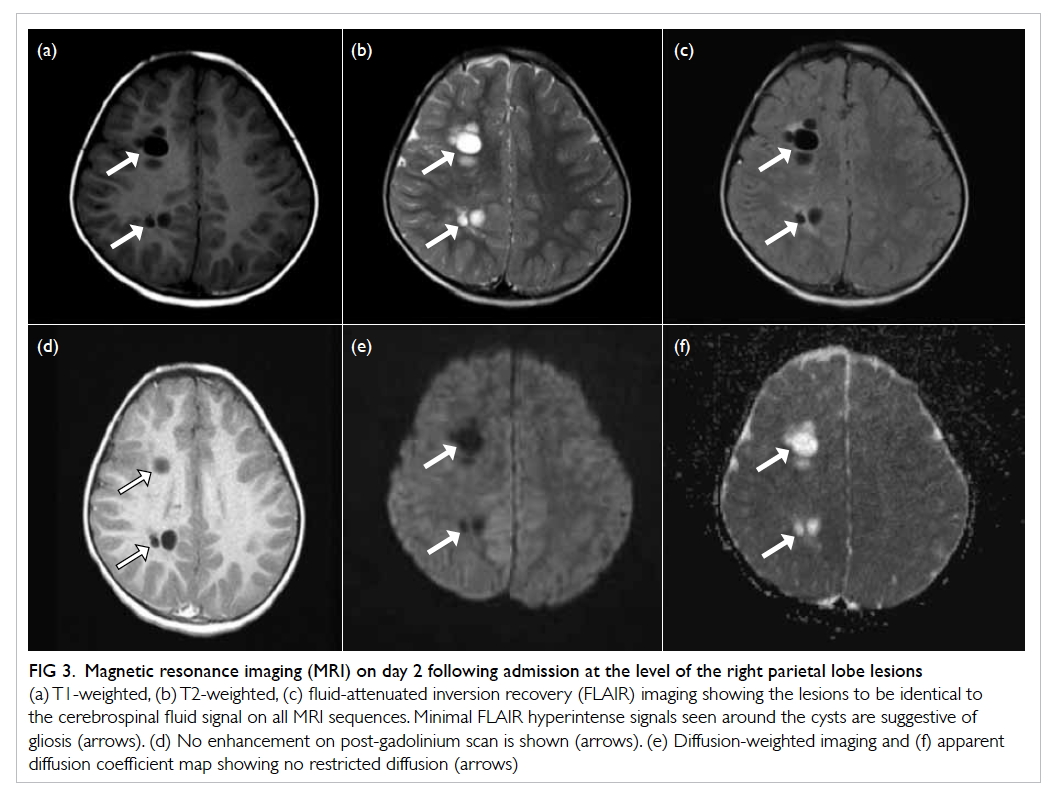
Figure 3. Magnetic resonance imaging (MRI) on day 2 following admission at the level of the right parietal lobe lesions
(a) T1-weighted, (b) T2-weighted, (c) fluid-attenuated inversion recovery (FLAIR) imaging showing the lesions to be identical to the cerebrospinal fluid signal on all MRI sequences. Minimal FLAIR hyperintense signals seen around the cysts are suggestive of gliosis (arrows). (d) No enhancement on post-gadolinium scan is shown (arrows). (e) Diffusion-weighted imaging and (f) apparent diffusion coefficient map showing no restricted diffusion (arrows)
Imaging features were not compatible with
brain abscess so surgical aspiration was withheld.
Cerebral hydatid disease was considered a possible
diagnosis based on imaging and the child was
commenced on oral albendazole 15 mg/kg/day. This
diagnosis was subsequently disproved given the
lack of an exposure history, absence of Echinococcus
granulosus antibody in serum, and absence of cysts
in the liver and spleen on ultrasonography.
Influenza A virus antigen was subsequently
detected in nasopharyngeal aspirate. The child was
prescribed antiviral treatment with consequent
cessation of seizures and clinical improvement. The
clinical diagnosis was influenza virus–associated
encephalopathy.
Follow-up CT and MRI 3 weeks later showed
the non-enhancing cystic lesions to be unchanged
in size and signal characteristics. The lesions were
classified as giant tumefactive perivascular spaces
(GTPVS).
The perivascular spaces (PVS) of the brain are
pial-lined, interstitial fluid-filled cystic spaces. They
accompany penetrating arteries as they enter the
brain parenchyma. These are normal structures that
can be found in all ages.1 Most PVS are small in size
and usually measure less than 5 mm.1 Larger (>1 cm)
PVS have been reported and these are called GTPVS,
which can occur as single or multiple clustered cysts.2
Such GTPVS in cerebral white matter can have mild
FLAIR hyperintensities in the surrounding white
matter1 that can be due to gliosis.2
Of note, GTPVS are often incidental
findings on imaging. They occur in characteristic
locations alongside penetrating vessels in the
mesencephalothalamic area, cerebral white matter,
and cerebellar dentate nuclei.2 They follow the CSF
signal on MRI and do not enhance.
Sometimes, GTPVS can be misinterpreted
as other pathological processes.1 2 3 Lack of a solid
component and complete suppression on FLAIR
differentiates them from cystic neoplasms.1 Nil
to minimal peri-lesional FLAIR signals help to
differentiate them from cystic infarction and
mucopolysaccharidosis. Parasitic cysts, in particular
hydatid cysts, can have identical imaging features
and necessitate clinical correlation for exclusion as
in this case. Neuroepithelial cysts also have identical
imaging features but can only be differentiated from
GTPVS by histopathology.1 Knowledge of this entity,
its imaging features, and characteristic locations is essential to avoid unnecessary medical treatment
and surgical biopsy/intervention.
References
1. Kwee RM, Kwee TC. Virchow-Robin spaces at MR
imaging. Radiographics 2007;21:1071-86. Crossref
2. Salzman KL, Osborn AG, House P, et al. Giant tumefactive
perivascular spaces. AJNR Am J Neuroradiol 2005;26:298-305.
3. Sankararaman S, Velayuthan S, Ambekar S, Gonzalez-Toledo E. Giant tumefactive perivascular spaces: A
further case. J Pediatr Neurosci 2013;8:108-10. Crossref

