DOI: 10.12809/hkmj166086
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Management of an incidental finding of right internal jugular vein agenesis
Vincent KF Kong, FANZCA, FHKAM (Anaesthesiology); CJ Jian, MB, BS; R Ji, MS, MB, BS; Michael G Irwin, MD, FHKAM (Anaesthesiology)
Department of Anaesthesia, HKU-Shenzhen Hospital, 1 Haiyuan Road, Futian District, Shenzhen, China
Corresponding author: Dr Vincent KF Kong (vincentkong@hku.hk)
Case report
A 43-year-old woman was referred to the University
of Hong Kong–Shenzhen Hospital in August
2016 with a 10-year history of hepatolithiasis.
Computed tomography (CT) of the abdomen
demonstrated multiple stones in the right posterior
portion of the liver, the common biliary duct, and
the gallbladder. Dilatation and inflammation of
both intra- and extra-hepatic ducts were apparent
and an elective right hepatectomy along with a
Roux-en-Y hepaticojejunostomy was arranged.
Preoperative physical examination was normal apart
from hypertension (168/105 mm Hg). Laboratory
tests revealed a microcytic, hypochromic anaemia
(haemoglobin, 97 g/L), hyperuricaemia, and mildly
elevated alkaline phosphatase. Liver/renal function,
clotting profile, chest X-ray, and electrocardiogram
were all normal. General anaesthesia was induced
intravenously with propofol and remifentanil using
a target-controlled infusion (Marsh model) under
the guidance of the Bispectral Index monitoring
system (Covidien, Boulder [CO], US). Tracheal
intubation was performed following administration
of rocuronium and anaesthesia maintained
intravenously with intermittent positive pressure
ventilation in oxygen and air. The patient was
positioned for right internal jugular vein (IJV)
cannulation.
Pre-insertion sonographic evaluation of the
right cervical region (SonoSite M-Turbo, Bothell
[WA], US) using a linear, high-frequency transducer
(HFL38, 6-13 MHz) revealed only a single pulsatile
vessel that was non-compressible and suggestive of
the right carotid artery. The characteristic pulsatile
blood flow was confirmed by Doppler. There was
no evidence of the right IJV despite repositioning of
the patient’s head, use of minimal pressure on the
probe with colour flow mapping, and the application
of Valsalva manoeuvre. Ultrasonography of the
left side showed normal anatomy with good size
of IJV. Following a brief discussion, the consultant
anaesthetist and the surgeon decided to proceed
with surgery without a central venous catheter. At the
end of liver resection, the patient began to develop
hypotension that was marginally responsive to fluid resuscitation and moderate-dose phenylephrine
infusion through the large-bore peripheral lines.
The operation lasted approximately 5 hours with
a total blood loss of 350 mL. Tracheal intubation
was continued postoperatively and the patient
was transferred to the intensive care unit (ICU).
Central venous cannulation was not attempted by
ICU physicians and the patient was extubated on
postoperative day 1 and discharged from the ICU
on postoperative day 4. The patient was followed up
by the attending and consultant anaesthetists after
surgery. The incidental finding of her neck condition
was explained and she agreed to undergo further
investigations for a possible vascular anomaly.
Ultrasonography (iU Elite model with a L12-5
transducer; Philips Medical System, Bothell [WA],
US) of the neck by a radiologist on postoperative day
5 confirmed the absence of thrombosis and the right
IJV. The left IJV was normal (diameter, 15-19 mm).
Multisection CT angiography of the head and neck
region revealed agenesis of the right IJV (Fig). There
was no other vascular anomaly in the head and neck
region. The patient was discharged from hospital on
day 11 postoperatively.
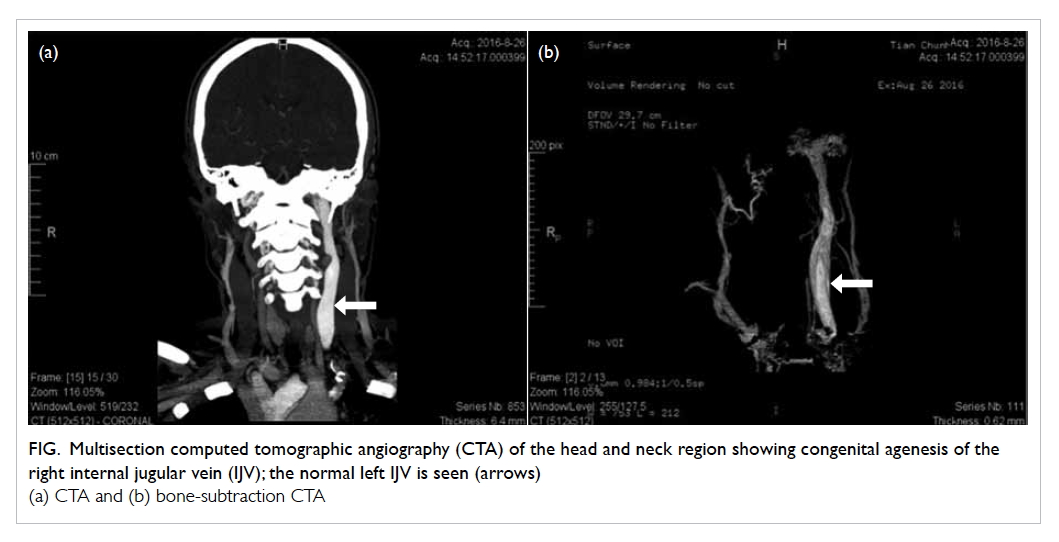
Figure. Multisection computed tomographic angiography (CTA) of the head and neck region showing congenital agenesis of the right internal jugular vein (IJV); the normal left IJV is seen (arrows)
(a) CTA and (b) bone-subtraction CTA
Discussion
Non-visualisation of the right IJV on two-dimensional
sonographic scanning can be due to operator (eg
suboptimal patient positioning, inappropriate
machine setting, and excessive pressure on the probe)
and patient (eg vascular thrombosis, congenital
anomalies such as hypoplasia, agenesis) factors.
Congenital agenesis of the IJV is an extremely rare
anomaly.1 The risks associated with central venous
cannulation of the left IJV or the right subclavian vein
in our patient before surgery may have outweighed
the benefits. The IJVs are the principal vessels for
cerebral venous drainage. Injury and/or thrombosis
of the left IJV can still occur even if proper precautions
are taken during catheterisation. Disruption of the
alternative channels of venous drainage from the
cranial cavity in a patient with congenital agenesis
of the IJV may have serious consequences. Vascular
malformations in the head and neck region result
from embryological developmental deformities and can co-exist asymptomatically. Further diagnostic
analysis before cannulation of her right subclavian
vein would have provided extra safety.
Low central venous pressure (CVP) during
anaesthesia reduces surgical blood loss in major
hepatic resection,2 and central venous cannulation
of the right IJV to enable CVP monitoring has
become a routine practice in many places prior
to major hepatectomy. Less invasive techniques
such as peripheral venous pressure and external
jugular venous pressure measurement allow
an acceptable estimation of the CVP with less
associated morbidity and mortality. Stroke volume
variation (SVV) derived from the Vigileo-FloTrac
system (Edwards Lifesciences, Irvine [CA], US) can
be a safe and effective alternative to conventional
CVP monitoring during hepatic resection.3 The
FloTrac system is based on arterial pulse contour
analysis and does not require external calibration,
thermodilution, or dye dilution. Unlike CVP that is a
favoured but static measure of intravascular volume,
SVV monitors dynamically the physiological
interactions of the heart and lungs in mechanically
ventilated patients to not only estimate fluid status
but also predict fluid responsiveness. A high SVV of
10% to 20% is associated with significantly less blood
loss during liver resection.4 Nonetheless a multi-parametric
approach should be adopted to guide
fluid management in complicated cases because
every haemodynamic variable has limitations and
interferes with other variables.
Anaesthetists should function as perioperative physicians to minimise patient harm and create
extra value to the episode of patient care. A simple,
focused ultrasound examination of the neck during
preoperative assessment can diagnose variation
in vessel position or abnormalities of the vessel. It
has been recommended by the National Institute
for Health and Care Excellence in the United Kingdom since
20025 and this report further supports its routine
use. Early recognition of these anomalies enables
extra precautions to be taken (eg discussion with
the patient and surgeons for alternative anaesthetic
plans, cannulation sites, monitoring strategies,
and further investigation before surgery) to reduce
patient harm.
References
1. Kayiran O, Calli C, Emre A, Soy FK. Congenital agenesis of
the internal jugular vein: an extremely rare anomaly. Case
Rep Surg 2015;2015:637067.
2. Wang WD, Liang LJ, Huang XQ, Yin XY. Low central
venous pressure reduces blood loss in hepatectomy. World
J Gastroenterol 2006;12:935-9. Crossref
3. Reineke R, Meroni R, Votta C, et al. Enhanced recovery after
open hepatectomy with minimally invasive haemodynamic
monitoring: A successful challenge. A comparative study
from a single institution. Clin Nutr ESPEN 2016;12:e53-4. Crossref
4. Dunki-Jacobs EM, Philips P, Scoggins CR, McMasters
KM, Martin RC 2nd. Stroke volume variation in hepatic
resection: a replacement for standard central venous
pressure monitoring. Ann Surg Oncol 2014;21:473-8. Crossref
5. Kong V, Yuen M, Irwin M. Perioperative ultrasonography:
Ultrasound and vascular cannulation. CPD Anaesthesia
2007;9:3-9.

