DOI: 10.12809/hkmj164957
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Primary hyperparathyroidism caused by mediastinal ectopic parathyroid adenoma
M Chen, MM1; WB Zhou, PhD, MD1; JF Xu, MM2; K Sun, MM3
1 Department of Endocrinology, The First Affiliated Hospital, College of Medicine, Zhejiang University, #79, Qingchun Road, Hangzhou, Zhejiang, 310003, China
2 Department of Radiology, The First Affiliated Hospital, College of Medicine, Zhejiang University, #79, Qingchun Road, Hangzhou, Zhejiang, 310003, China
3 Department of Pathology, The First Affiliated Hospital, College of Medicine, Zhejiang University, #79, Qingchun Road, Hangzhou, Zhejiang, 310003, China
Corresponding author: Dr WB Zhou (zjuzwb@126.com)
Case report
A 37-year-old Chinese woman was admitted to
the First Affiliated Hospital, College of Medicine,
Zhejiang University, China in July 2009 with pain in
the upper back and hip for 9 months. She denied any
chronic medication or illness. Her serum calcium
level was 2.73 mmol/L (reference range [RR], 2.08-2.60 mmol/L), phosphorus 0.68 mmol/L (RR, 0.81-1.62 mmol/L), alkaline phosphatase 366 IU/L (RR,
30-115 IU/L), and intact parathyroid hormone (iPTH)
1154 pg/mL (RR, 12-65 pg/mL). T-score and Z-score
for femoral bone mineral density were -2.7 and
-2.8, respectively. Cervical computed tomography
(CT) scan and thyroid, parathyroid, and abdominal (including pancreas, adrenals) ultrasonography
were unremarkable. Anterior planar technetium
(99mTc) sestamibi (MIBI) scintigraphy images of the
neck and chest showed a focal shadow with intense
tracer uptake in the superior thorax at 15 minutes (Fig a) and 120 minutes (Fig b) following injection of 99mTc-MIBI. Thoracic CT revealed a contrast-enhanced
nodule with soft tissue density of 2.9 x 1.3 cm in
the anterior mediastinum (Fig c). Thoracic and
abdominal CT showed a brown tumour in the right
omoplate, the fourth posterior left rib, and iliac bone
(Figs d and e).
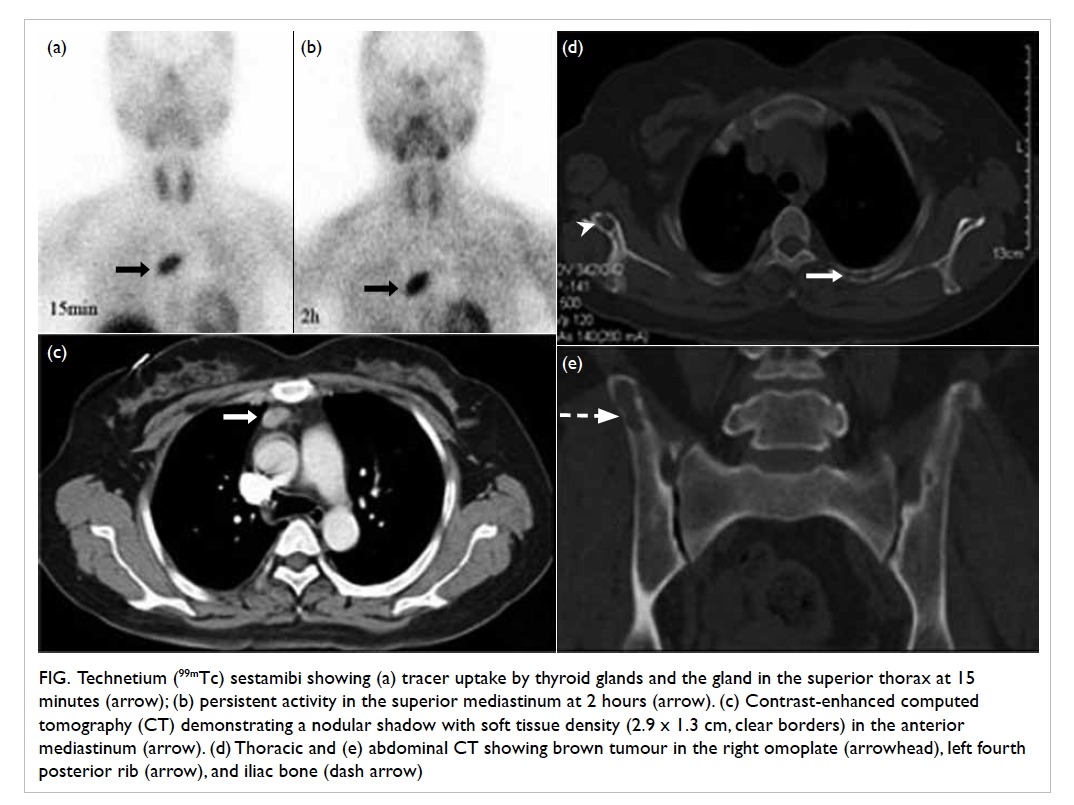
Figure. Technetium (99mTc) sestamibi showing (a) tracer uptake by thyroid glands and the gland in the superior thorax at 15 minutes (arrow); (b) persistent activity in the superior mediastinum at 2 hours (arrow). (c) Contrast-enhanced computed tomography (CT) demonstrating a nodular shadow with soft tissue density (2.9 x 1.3 cm, clear borders) in the anterior mediastinum (arrow). (d) Thoracic and (e) abdominal CT showing brown tumour in the right omoplate (arrowhead), left fourth posterior rib (arrow), and iliac bone (dash arrow)
A mid-sternal thoracotomy was performed. A
dark red mass of 4 x 2.4 x 1 cm was found in the thymus isthmus and resected. The mediastinal
mass was covered with a thin fibrous capsule and
on section showed a greyish cut surface. Histology
confirmed the presence of ectopic parathyroid
adenoma composed predominantly of oxyphil cells
arranged in acinar pattern. Serum calcium level was 2.18
mmol/L and iPTH 17.2 pg/mL 16 hours after surgery.
Hypocalcaemia (serum calcium, 1.68 mmol/L) and
hungry bone syndrome occurred 3 days after surgery
and gradually improved over a week with calcium
carbonate and calcitriol supplementation that was
started after surgery and continued thereafter.
Serum calcium and iPTH remained normal after 5
years’ follow-up.
Discussion
A diagnosis of primary hyperparathyroidism in
a symptomatic patient is made in the presence
of hypercalcaemia, hypophosphataemia, and
raised levels of alkaline phosphatase and
iPTH,1 as demonstrated in our case. Primary
hyperparathyroidism occurs in approximately
1% of the adult population, commonly due to
solitary parathyroid adenomas (85%).1 Primary
hyperparathyroidism due to ectopic parathyroid
adenomas can pose diagnostic and management
challenges, especially when imaging studies provide
limited sensitivity.2
The embryological origin of the parathyroid
glands is the endoderm of the third and fourth
pharyngeal pouches, from where these glands
migrate to their usual position behind the thyroid
gland. It is well known that parathyroid glands
can be found in aberrant locations, mainly in the
thyroid parenchyma or in the mediastinum.3 The
high incidence of ectopic inferior parathyroid glands
has been attributed to abnormal migration during
embryogenesis. Since parathyroid glands lack
capsular fixation, an ectopic parathyroid gland may
also develop from a gland that is initially present in a
normal anatomic position but which enlarges and is
displaced to an ectopic location where there is little
resistance.
Ultrasonography is commonly used to locate
enlarged parathyroid glands due to its convenience
and low cost. Its ability to detect abnormalities,
however, depends on the experience and skill of the
operator so sensitivity in the localisation of enlarged
parathyroid glands varies greatly (44%-87%).2 Ectopic
parathyroid adenomas may be detected with MIBI at a
sensitivity level almost identical to that of orthotopic
adenomas. Focal increased activity separated from
the lower pole of the thyroid on MIBI images gives
a high probability for locating ectopic parathyroid
adenoma in the thymus. Of note, 99mTc-MIBI is a
non-specific tracer that is taken up by mitochondria
so any mitochondria-rich cells may show uptake.
Mitochondrial density in an adenoma is also a major factor that can cause prolonged retention of 99mTc.
This is evidenced by the number of mitochondrion in
lesions detected by scintigraphy that is significantly
higher than in those that are missed, with the highest
ratio of mitochondria per cell found in oxyphil
cells. The typical pattern in a parathyroid adenoma
demonstrates a prolonged retention of 99mTc-MIBI
in the adenoma with rapid washout of the tracer
from normal thyroid tissue. The degree of MIBI
uptake in parathyroid adenomas has been reportedly
correlated with the size of gland and the cytological
composition (greater uptake seen in adenomas with
dominance of oxyphil cells over chief cells).2
Of note, CT may further contribute to the
identification of ectopic parathyroids and the
differential diagnosis from other lesions. In our
cases, the parathyroid glands were not located
by ultrasonography although a combination of
MIBI scintigraphy and CT imaging accurately
localised the tumour in the anterior mediastinum.
This highlights the usefulness of combining multiple
imaging techniques to locate an ectopic active
parathyroid gland. These combinations are cost-effective,
and considered an approach to routine
preoperative localisation of ectopic parathyroid
adenomas, especially in cases with a negative MIBI
scan.4
Hungry bone syndrome refers to the
rapid, profound, and prolonged hypocalcaemia
associated with hypophosphataemia following
parathyroidectomy as a result of extensive
remineralisation.5 Various risk factors of hungry
bone syndrome include older age, large parathyroid
adenoma, overt bone disease, and vitamin D
deficiency. Consequently, transient hypocalcaemia
is frequently encountered postoperatively;
the presence of mild hypocalcaemia provides
reassurance that the hyperactive adenomatous gland
has been successfully removed.
For any hypercalcaemia and high level of PTH
without parathyroid adenoma in the neck, physicians
should remain alert and continue to search for
ectopic locations using a combination of imaging
techniques. The mediastinum must be cautiously
explored since it is a very common location for
ectopic parathyroid adenoma. The combination of
several imaging techniques has an incremental effect
on the localisation of ectopic parathyroid adenomas
compared with use of either one technique alone.
References
1. AACE/AAES Task Force on Primary Hyperparathyroidism.
The American Association of Clinical Endocrinologists
and the American Association of Endocrine Surgeons
position statement on the diagnosis and management of
primary hyperparathyroidism. Endocr Pract 2005;11:49-54. Crossref
2. Haber RS, Kim CK, Inabnet WB. Ultrasonography for
preoperative localization of enlarged parathyroid glands in primary hyperparathyroidism: comparison with (99m)
technetium sestamibi scintigraphy. Clin Endocrinol (Oxf) 2002;57:241-9. Crossref
3. Noussios G, Anagnostis P, Natsis K. Ectopic parathyroid
glands and their anatomical, clinical and surgical
implications. Exp Clin Endocrinol Diabetes 2012;120:604-10. Crossref
4. Elaraj DM, Sippel RS, Lindsay S, et al. Are additional localization studies and referral indicated for patients with
primary hyperparathyroidism who have negative sestamibi scan results? Arch Surg 2010;145:578-81. Crossref
5. Witteveen JE, van Thiel S, Romijn JA, Hamdy NA. Hungry
bone syndrome: still a challenge in the post-operative
management of primary hyperparathyroidism: a systematic
review of the literature. Eur J Endocrinol 2013;168:R45-53. Crossref

