DOI: 10.12809/hkmj166090
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
MEDICAL PRACTICE
In-situ medical simulation for pre-implementation testing of clinical service in a regional hospital in Hong Kong
PP Chen, FHKAM (Anaesthesiology)1; Nick TK Tsui, FHKAM (Anaesthesiology)1; Arthur SW Fung, MB, BS1; Alick HF Chiu, BScN1; Wendy CW Wong, FHKAM (Anaesthesiology)1; HT Leong, FHKAM (Surgery)2;
Paul SF Lee, FHKAM (Radiology)3; James YW Lau, FHKAM (Surgery)4
1 Department of Anaesthesiology and Operating Services, North District
Hospital, Sheung Shui, Hong Kong
2 Department of Surgery, North District Hospital, Sheung Shui, Hong Kong
3 Department of Radiology, North District Hospital, Sheung Shui, Hong
Kong
4 Department of Surgery, Prince of Wales Hospital, The Chinese University
of Hong Kong, Shatin, Hong Kong
Corresponding author: Dr PP Chen (chenpp@ha.org.hk)
Abstract
The implementation of a new clinical service is
associated with anxiety and challenges that may
prevent smooth and safe execution of the service.
Unexpected issues may not be apparent until the
actual clinical service commences. We present a
novel approach to test the new clinical setting before
actual implementation of our endovascular aortic
repair service. In-situ simulation at the new clinical
location would enable identification of potential
process and system issues prior to implementation of
the service. After preliminary planning, a simulation
test utilising a case scenario with actual simulation
of the entire care process was carried out to identify
any logistic, equipment, settings or clinical workflow
issues, and to trial a contingency plan for a surgical
complication. All patient care including anaesthetic,
surgical, and nursing procedures and processes were
simulated and tested. Overall, 17 vital process and
system issues were identified during the simulation
as potential clinical concerns. They included
difficult patient positioning, draping pattern,
unsatisfactory equipment setup, inadequate critical
surgical instruments, blood products logistics, and
inadequate nursing support during crisis. In-situ
simulation provides an innovative method to
identify critical deficiencies and unexpected issues before implementation of a new clinical service.
Life-threatening and serious practical issues can
be identified and corrected before formal service
commences. This article describes our experience
with the use of simulation in pre-implementation
testing of a clinical process or service. We found the
method useful and would recommend it to others.
Introduction
The implementation of clinical service in a new
hospital facility or location is associated with
challenges that may prevent a smooth and safe
execution of the service.1 New equipment, unfamiliar
surroundings and setup, untested emergency
care support, alarm systems and logistics, and
new interdisciplinary staff mix may contribute to
unexpected negative outcomes. Anticipated and
actual practices may differ significantly and need
to be modified to adapt to the new environment.
In addition, some unexpected issues may not be
apparent until the actual clinical service commences.
Such concerns may lead to significant anxiety
and stress in both administrative and clinical staff
involved in the planning of the new service.
Clinical simulation is commonly employed in
education and patient safety training of frontline health care professionals.2 It is now becoming
increasingly common that simulation is also used in
assessment, credentialing, and even in health care
system integration and feasibility testing of clinical
process and equipment.3 4 Advanced simulation
methods have previously been adopted to assess
and optimise workflow and setup at new facility
prior to clinical operation.5 6 Usability testing of new
equipment with simulation techniques may enhance
medical safety before clinical application. In-situ
simulation at a new clinical location offers a unique
opportunity to identify potential process and system
issues prior to implementation of a new service.
This type of simulation method is valuable to assess,
troubleshoot, or develop new system processes.7
Our hospital is a local district hospital with
about 480 beds. A new endovascular aortic repair
(EVAR) service was planned in the angiography suite located in the Department of Radiology on the
hospital ground floor. No elective surgical procedure
under anaesthesia had previously been performed
at this location. This location is remote from the
operating theatre suite and intensive care unit that
are located on the second floor of the same building.
We conducted an in-situ simulation of a clinical case
2 weeks before the first procedure in a real patient
to assess the readiness of our preparation for the
clinical service.
Definitions
Simulation is defined as a technique that creates a
situation or environment that allows a person to
experience a representation of a real event for the
purpose of practice, learning, evaluation and testing,
or to gain an understanding of systems or human
actions.7 In-situ simulation refers to simulation
exercises that take place in the actual patient care
setting/environment in an effort to achieve a high
level of fidelity and realism.7
Planning a new service
Effective and safe planning of a new service is not only
challenging but often a tedious and fretful procedure.
In our case, key stakeholders including the operating
theatre nursing team, anaesthesiologists, surgeons,
and angiography suite staff met on four occasions
over 2 months to discuss the logistics of patient flow,
clinical service needs, and setup. Patient selection criteria, preparation, transfer logistics, location
setup, equipment, drugs and consumables stocks,
and postoperative care were discussed. Workflow
logistics; clinical care plans; detailed emergency and
contingency plans; and lists of essential surgical,
anaesthetic, and nursing consumables and equipment
were worked out and agreed by all parties. Several
visits to the angiography suites were held to assess
the site and familiarise staff. The position of patient
and health care staff, equipment, and overall setup
were tried out.
At the last planning session, a simulated case
was proposed to be performed at the new clinical
location to test our preparation before the first real
patient case was conducted.
Research approval and informed consent
Clinical research ethics committee approval was not
required as this was a simulated site-testing exercise
with no study participant or data involved. All
parties involved consented to participate voluntarily,
and the project was supported and approved by
the Hospital’s Chief Executive and the Hospital’s
Working Group on EVAR service.
Clinical scenario
In order to facilitate the simulation test, a clinical
case scenario was developed by two co-authors (TTK
and WCW) who are simulation education–trained
instructors and were the main coordinators of the
exercise. The scenario was of a routine case scheduled
for EVAR procedure under general anaesthesia in
the angiography suite. The case background involved
a 78-year-old man with multiple stable medical
conditions including hypertension, history of
congestive cardiac failure, chronic renal impairment,
and a 7-cm infrarenal abdominal aortic aneurysm
scheduled for endovascular aortic surgery. He was
on aspirin, metoprolol, lisinopril, amlodipine, and
isosorbide dinitrate. Echocardiography assessment
had reported a left ventricular ejection fraction of
35%. Blood type and screen, and a postoperative
bed in intensive care unit were available before the
operation. Premedication with oral N-acetylcysteine,
midazolam, and his usual medications was prescribed
and administered in the ward prior to transfer to the
angiography suite.
The scenario began with patient transferring to
the angiography suite by ward staff and on arrival,
checking by the angiography suite nurse. Timeout
was then performed with the anaesthesiologists,
surgeon, and nurse in the angiography suite before the
anaesthetic procedure commenced. Invasive arterial
pressure monitoring was set up, and the patient was
anaesthetised on the transfer trolley before being
moved onto the angiography table. An anaesthetic
workstation (Primus; Drägerwerk AG & Co. KGaA,
Germany) with Infinity C700 physiological monitor
(Drägerwerk AG & Co. KGaA, Germany) was used
for the general anaesthesia. The anaesthesiologist
simulated the induction of general anaesthesia on
a training simulator with full virtual physiological
monitoring. The anaesthetic procedure tested the
setup at the head of the ‘operating table’ and the
logistics of delivering anaesthesia to the patient in
the small and compact room.
Following general anaesthesia, the surgeon
cleaned and draped the surgical field, and
commenced the surgical procedure according to
his usual practice at another hospital. One nurse
scrubbed in and another two circulating nurses
assisted the procedure. All required surgical
instruments and equipment were laid out on sterile
trolleys. The surgical team performed each step of
the procedure as in a real clinical case including
imitating the femoral arterial puncture and insertion
of the guidewire and aortic stent to test the surgical
setup, equipment locations, and the positions of
staff and patient. No EVAR simulator or manikin was
used for the surgical procedure part as we did not
intend to assess the technical aspects of the surgical
procedure.
When the surgical part of the exercise was
completed, the scenario proceeded to evaluate the
contingency plan in case of a surgical complication
resulting in haemorrhagic shock. The patient would
need to be transferred to the operating theatre for
open surgery to stop the bleeding, instead of directly
to the intensive care unit from the angiography suite
after completion of the procedure as per preoperative
plan. The surgeon was able to test the availability
of surgical instruments for haemostasis while the
anaesthesiology team was able to test the logistics,
clinical support, and treatment protocols for fluid
and blood resuscitation, and urgent arrangements
for transferring to the main operating theatre. The
site of surgical complication was not specified and
the surgeon went through a mental exercise with
the surgical team of different surgical management
requirements during the crisis.
Simulation exercise
Two co-authors were responsible for coordinating,
directing, and running the exercise. Frontline
representatives from the anaesthetic, vascular
surgery, operating theatre nursing, and angiography
suite teams who will be involved in the new future
clinical service were nominated by their heads of
department to participate in the simulation exercise.
An actor who was a ward nurse played the role of
the patient during transfer from the ward to the
angiography suite as it facilitated the checking
procedure. The patient checking part of the scenario
also involved a participant nurse from the surgical
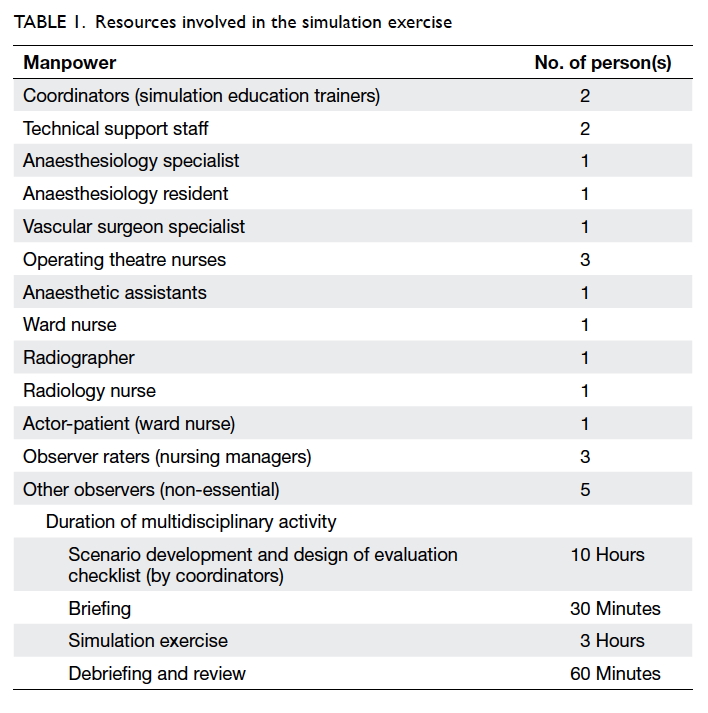
ward who accompanied the patient from the ward. The participants involved are shown in Table 1.
A high-fidelity simulator (SimMan 3G;
Laerdal, Stavanger, Norway) was used during
the perioperative phase from timeout procedure
onwards. The SimMan 3G can be controlled by a
wireless laptop, and is able to generate virtual vital
signs on a monitor. This simulator has peripheral
pulses, chest expansion, pupillary responses, and
can simulate normal and abnormal breath sounds,
heart sounds, pupil size, and normal and difficult
airway, among other functions. The entire induction
of anaesthesia including tracheal intubation was
performed on the simulator. The technical part of
the simulation was supported by two staff from the
Simulation and Training Centre.
The simulation exercise took place in the
afternoon of a normal working day. The area of
simulation exercise was an isolated part of the
Department of Radiology with minimal patient
traffic. A half-hour briefing of involved parties
was conducted prior to the commencement of the
exercise. The objective of the exercise to test the
workflow logistics, setup, and care plans of the
new service was explained. All participants were
instructed to play their professional role during the
simulated exercise, as they would in the real clinical
situation (Fig 1). The exercise was carried out in
four phases: a pre-anaesthetic phase, anaesthesia induction phase, operative phase, and postoperative
phase.
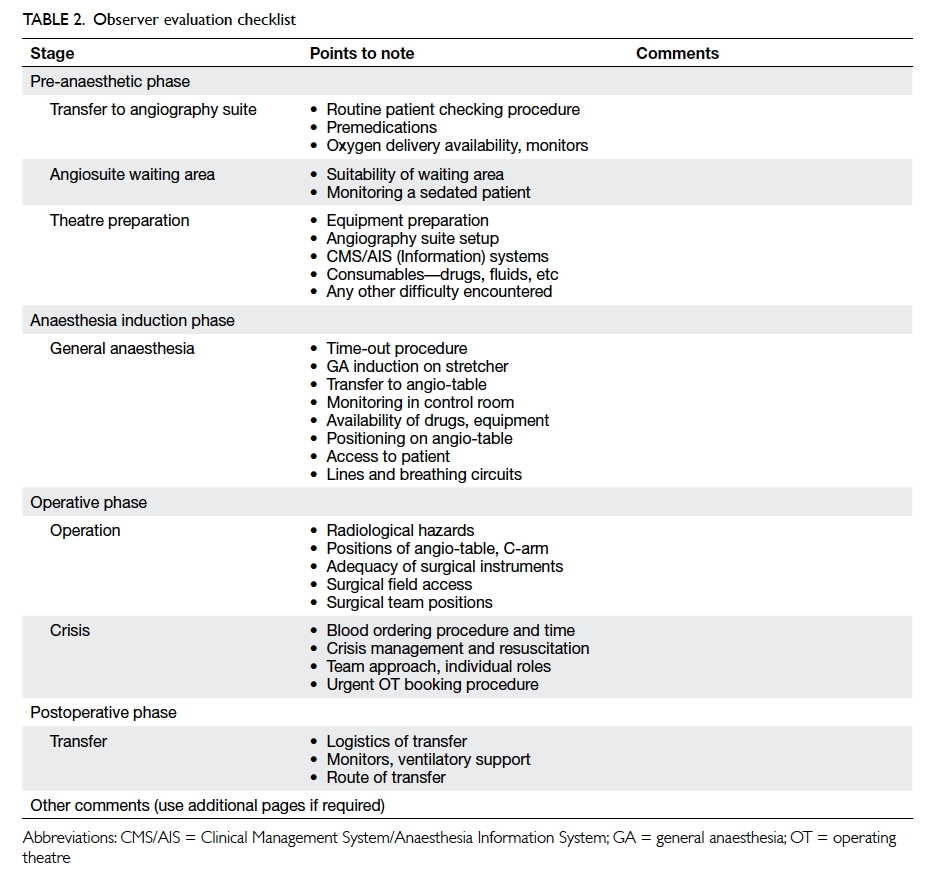
Data collection and evaluation
Three observers who were nurse managers from the
operating theatre and surgical wards evaluated the scenario and made comments independently. An
evaluation checklist was designed by the exercise
coordinators together with members of the planning
team for observers to identify any deficiency and
safety issues associated with the event at each phase
(Table 2). The checklist followed the anticipated
flow of events during the case. The evaluation began
with pre-medication and sending of the patient to
the angiography suite. Positioning, surgical draping,
range of X-ray table, and blood ordering logistics
were tested. After the scenario, all participants were
debriefed, and observers were invited to share their
observations. Areas of improvement were noted
and required alterations made by relevant team
members before scheduling first real patient for the
EVAR procedure in the angiography suite.
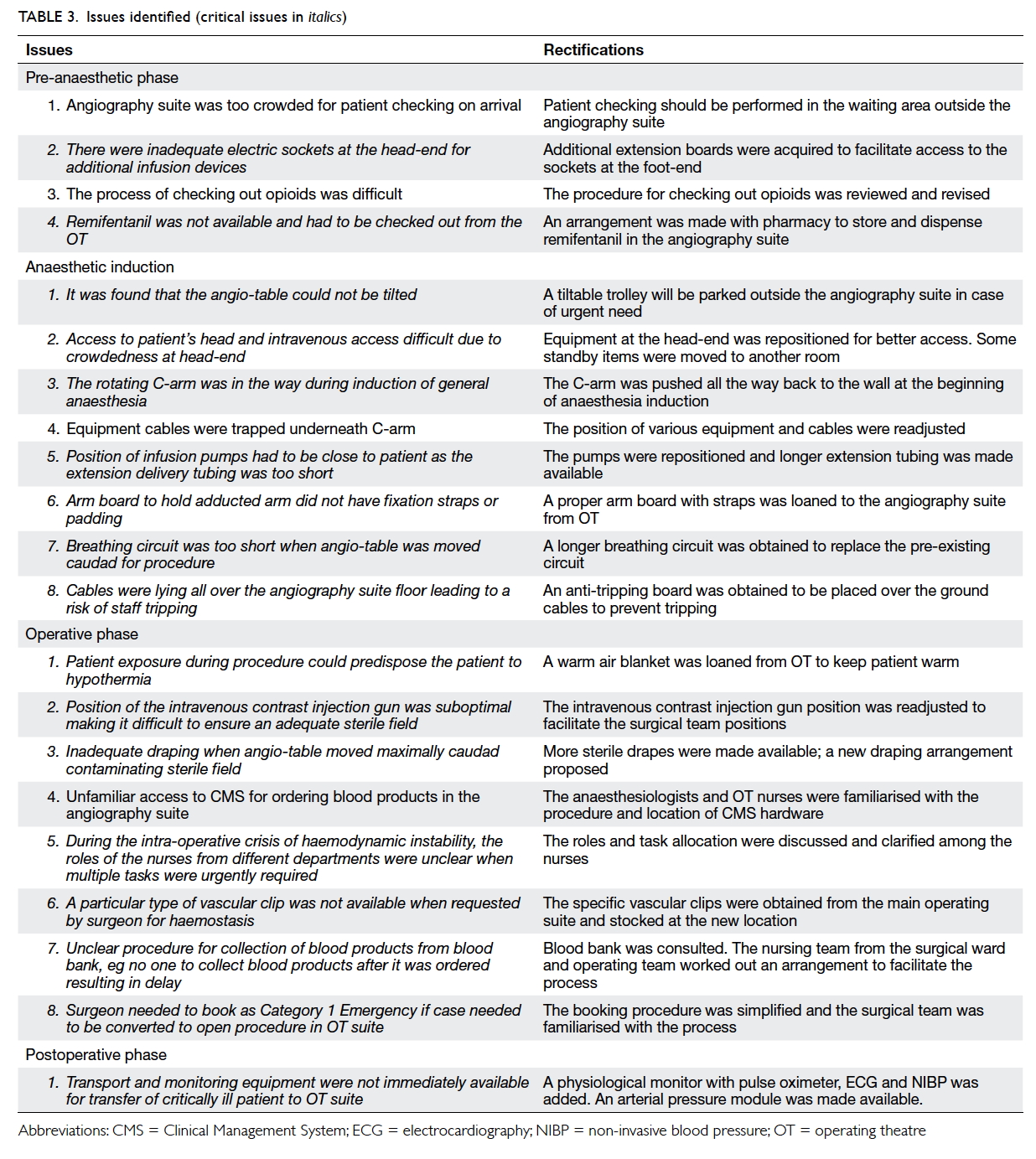
Issues identified
The in-situ simulation took place in the angiography suite over four phases in 3 hours. During the
simulation, 17 vital process and system issues were
identified, including anaesthetic and surgical issues
such as poor patient positioning, draping pattern,
unsatisfactory equipment setup, inadequate critical
surgical instruments, blood products requesting logistics, and inadequate nursing support during
the crisis (Table 3). Some of these deficiencies
were corrected immediately during the simulation
exercise. During the post-exercise, observer
checklist deficiencies and participant experience
were reviewed and discussed, and solutions devised.
Benefits of simulation testing
This is the first reported use of simulation for the
purpose of testing a new service in Hong Kong.
Previous publications have reported the effectiveness
of simulation-based methodology to identify
process gaps before major institutional change.5 6
Kobayashi et al5 found the utility of simulated patient
encounters in testing a new emergency department
functions and operational capabilities useful. The
trial run also helped in the design of an optimal
clinical care environment. In their experience, most
issues that arose were not apparent with traditional
preparation efforts. Staff also felt more comfortable
and confident attending to critical patients in the new
facility after participating in simulated scenarios.
Bender et al6 evaluated the function of a new
neonatal intensive care unit using simulation-based
technology and methodology. The exercise involved
multidisciplinary stakeholders in two simulated
clinical scenarios. They identified 164 latent safety
hazards in communication, facilities, supplies,
staffing, and training with over 90% of them resolved
at transition to the new facility. They concluded that
it provided valuable benefits for system refinement
and patient safety.6
Issues such as inadequate electrical sockets
and equipment electrical cables, breathing circuit
too short, and various positioning difficulties were
encountered in our simulation exercise despite
earlier planning and preparation (Fig 2). One may attribute such deficiencies to poor planning in
some situations, but simulation testing is in fact a
most suitable method to identify and iron out these
unanticipated problems, regardless of whether or not
they were the result of poor planning. Some issues
that may appear trivial and simple to correct were
identified as potential patient safety concerns in real
life. It was critical that these life-threatening problems
and other serious practical issues were identified
during the in-situ simulation as this enabled us to
make improvements to facilitate a more efficient
and safe service. Another example was related to the
management of a surgical complication during the
procedure, resulting in some urgency for the surgeon
to control the bleeding, a sudden and urgent blood
request for resuscitation by the anaesthesiologists,
and immediate need for emergency surgery in the
main theatre suite, all happening simultaneously.
An essential surgical vascular clip was found lacking
while there was confusion about the logistics of
getting blood products requested urgently. Other
concerns and difficulties were identified during the
crisis and were eventually rectified.
We did not repeat the simulation testing
after correcting the deficiencies identified at the
initial exercise because of lack of time. We did not
feel that it was necessary to repeat the simulation
although a second test may still have produced some
unexpected results. The first real case therefore
became an assessment of the final preparation. The
case was conducted 3 weeks after the simulation
testing. The procedures at each stage went as
anticipated without any problem. The first patient
did not require any blood transfusion and we were
not able to test the transfusion logistics in real life
after simulation testing. In a further subsequent
patient (real case) blood transfusion was required,
and the logistics of ordering and obtaining blood
products urgently were carried out smoothly and
uneventfully, indicating successful correction of the
initial problems with the blood collection procedure.
Challenges
A significant amount of time was spent in planning
the exercise so that it resembled closely the actual
workflow and procedures. As the clinical activity
involved several different specialties, it was
challenging to organise a multispecialty group to
plan and participate in the exercise. The number
of participants depends on the usual staffing need
of the clinical activity. The two coordinators who
were experienced medical simulation trainers
were the key persons who devised the scenario
and coordinated and executed the simulation
exercise. Most participants were required to attend
the briefing and simulation exercise only on the
day. Some discussions were conducted by email.
Although different specialty teams could have conducted their own individual exercise separately,
the cross-specialty interactions and benefits may not
have been apparent.
The leadership of the exercise and the hospital’s
support were vital for the smooth conduct of the
simulation testing. All the heads of department
involved in the new service, and our Hospital Chief
Executive supported the exercise making it easy to
organise the participants and observers.
It is important to test out the actual clinical
location. The setting up of the venue required
some time prior to the simulation exercise. In our
case, the availability of the angiography suite was a
challenge as we needed to find an unused session
when all stakeholders were also available. This will
be especially difficult in a busy hospital where the
clinical area may not be available during office hours.
In such cases, running the simulation exercise after
hours may be considered.
Although in-situ simulation remains an
effective method to test out a new location and service,
the organiser should ensure that the exercise is not
confused with a real clinical case. Special attention
should be given to the use of training equipment,
drugs, and consumables in the clinical area, so that
they are not inadvertently used in a real patient. Staff
and other patients in the clinical area should also be
aware that the simulation exercise is in progress. It
was helpful in our case that the angiography suite
was located in an area where patient traffic flow was
easily controlled in the afternoon.
In this exercise, we borrowed a high-fidelity
human patient simulator from our Simulation and
Training Centre. The manikin came with physiological
features and computer-controlled virtual vital signs.
It was a bonus to have access to this simulator
although a successful simulation test such as ours
may also be performed with a lower-fidelity manikin
such as that used for cardiopulmonary resuscitation
training. The advantage for us with this exercise was
that the high-fidelity simulator provided real-time
temporal changes in vital signs of the patient during
the surgical complication, thereby creating a sense of
urgency and crisis to the situation. This facilitated the
testing of contingency plans during the emergency.
The most important aspect of the exercise, however,
was not the simulator but the actual role play of
the scenario script and evaluation of the settings,
workflows logistics, and clinical processes. We were
fortunate that technical support from the Centre
was also available. In a hospital where such expertise
and resources may not be available, this should not
be a barrier to simulation-based testing as there is
the option to consult a simulation training centre for assistance.
The procedure and results of simulation testing
should be clearly documented. One limitation of this
study was that we did not document the exercise
with video recordings. Photographs were taken but
their quality was modest. These would have been
helpful in the discussion and sharing process.
Conclusion
It is advantageous to identify critical deficiencies and
unexpected issues that may not be apparent prior
to implementation of a new service. The testing of
a new clinical service, facility, or environment with
simulation technology requires considerable time,
effort, and expense. Very often traditional checks
and testing will only evaluate individual aspects of
a new facility in isolation and separately. Exposing
the new environment and critical services to a
simulated clinical event allows actual experience
of the settings, workflow, and clinical management
to reveal issues not apparent with the usual manual
checks.
Acknowledgements
The authors would like to express their appreciation
to staff at the Department of Radiology, Department
of Anaesthesiology and Operating Services,
Department of Surgery, and New Territories East
Cluster Simulation and Training Centre for their
support and contributions.
References
1. Berwick DM. A primer on leading the improvement of
systems. BMJ 1996;312:619-22. Crossref
2. Okuda Y, Bryson EO, DeMaria S Jr, et al. The utility of
simulation in medical education: what is the evidence? Mt
Sinai J Med 2009;76:330-43. Crossref
3. Holmboe E, Rizzolo MA, Sachdeva AK, Rosenberg M,
Ziv A. Simulation-based assessment and the regulation of
healthcare professionals. Simul Healthc 2011;6 Suppl:S58-62. Crossref
4. Landman AB, Redden L, Neri P, et al. Using a medical
simulation center as an electronic health record usability
laboratory. J Am Med Inform Assoc 2014;21:558-63. Crossref
5. Kobayashi L, Shapiro MJ, Sucov A, et al. Portable advanced
medical simulation for new emergency department testing
and orientation. Acad Emerg Med 2006;13:691-5. Crossref
6. Bender J, Shields R, Kennally K. Transportable enhanced
simulation technologies for pre-implementation limited
operations testing: neonatal intensive care unit. Simul
Healthc 2011;6:204-12. Crossref
7. Healthcare simulation dictionary. Society for Simulation
in Healthcare. June 2016. Available from: http://www.ssih.org/dictionary. Accessed Dec 2016.