Hong Kong Med J 2017 Aug;23(4):340–8 | Epub 7 Jul 2017
DOI: 10.12809/hkmj176217
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Secular trends in caesarean section rates over 20 years in a regional obstetric unit in Hong Kong
WH Chung, MRCOG, FHKAM (Obstetrics and Gynaecology); CW Kong, FHKAM (Obstetrics and Gynaecology); William WK To, FRCOG, FHKAM (Obstetrics and Gynaecology)
Department of Obstetrics and Gynaecology, United Christian Hospital, Kwun Tong, Hong Kong
Corresponding author: Dr WH Chung (vivianchung1228@hotmail.com)
Abstract
Introduction: Although caesarean section rates
have been increasing over the years in both public
and private sectors in Hong Kong, there has been
a paucity of formal surveys on local trends in such
rates. This study aimed to examine the trends in
caesarean section rates over a 20-year period at a
public regional obstetric unit in Hong Kong using
the Robson’s Ten-group Classification System.
Methods: All deliveries in a single obstetric unit
during a 20-year period (1995-2014) were classified
into 10 subgroups according to the Robson’s
classification. The annual caesarean section rate for
each subgroup was calculated and then stratified into
5-year intervals to analyse any significant trends.
Results: The caesarean section rates in a total of
86 262 births with complete data were analysed.
The overall caesarean section rate increased
modestly from 15.4% to 24.6% during the study
period. There was an obvious increasing trend for
caesarean section in those with previous caesarean
section (Robson’s category 5), breech presentation
at delivery (category 6 and 7), multiple pregnancy
(category 8), and preterm labour (category 10). A
gradual fall in caesarean section rate from 14.4% to 10.8% was seen in primiparous women with
term spontaneous labour (category 1). Statistically
significant differences (P<0.001) in these trends were
confirmed when the data were stratified into 5-year
intervals for comparison.
Conclusion: The rising caesarean section rate may
be associated with clinical management policies
that allow women with relative risk factors (such
as breech, previous caesarean section, or multiple
pregnancy) to opt for caesarean section. This rise
was counterbalanced by a decrease in primary
caesarean section rate in primiparous women with
spontaneous labour. The trend for caesarean section
was more in line with patient expectations rather
than evidence-based practice.
New knowledge added by this study
- Pregnancy with previous caesarean section (CS) was the principal contributing factor to rising CS trend.
- In addition, a significant increase in CS rate was observed in those with breech presentation, multiple pregnancy, and preterm labour.
- To reverse this rise, policies should aim to reduce CS rate for first births by adopting external cephalic version and safe vaginal delivery technique for twins. Vaginal delivery after previous CS can be promoted to reduce repeat CS.
- The results of this study should encourage obstetric units to audit their own CS trends using the Robson’s classification, analyse the extent of rise for each class, identify areas for improvement, and institute appropriate changes in clinical practice.
Introduction
The crude rate of caesarean section (CS) deliveries
is considered an important global indicator when
measuring access to obstetric care.1 Previous
ecological analysis in primitive lower-income
countries revealed that with the introduction of
safe CS deliveries, small increases in CS rates, if
performed in women with a medical indication,
could dramatically reduce maternal and newborn
mortality.1 2 3 On the other hand, CS rates in developed
countries have risen steeply since the 1970s and 1980s4 without any obvious evidence of significant
improvements in pregnancy outcome.1 5 High CS
rates have since been an issue of international
public health concern. In 1985, the World Health
Organization (WHO) stated that there was no
justification for any region to have a CS rate higher
than 10% to 15%.6 There is a lack of scientific evidence
of any substantial maternal or perinatal benefit from
increasing CS rates and some studies contrarily
have shown that higher rates may be associated
with negative consequences to maternal and child health.7 8 Despite this, CS rates have continued to
increase worldwide in middle- and high-income
countries. The WHO-recommended upper limit of
15% has been grossly exceeded by most centres in
developed countries over the last two decades.9
The lack of a standardised classification system
to facilitate monitoring and comparison of CS rates
in a consistent and action-oriented manner is one of
the factors that makes changes to CS trends difficult
to understand.10 Previous discussions often focused
on total CS rates and did not yield information about
the underlying reasons. The Robson’s Ten-group
Classification System is one of the best methods that
fulfils current international and institutional needs
to monitor and analyse CS rates.11 The classification
system divides women into 10 groups based on
basic epidemiological and obstetric characteristics,
including parity, previous uterine scar, preterm
(<37 weeks) or term delivery, fetal presentation,
singleton or multiple pregnancy, or whether labour
is spontaneous or induced. The actual indication
for CS is not needed for such categorisation. As
the groups are totally inclusive and mutually
exclusive, the classification system can be applied
prospectively. All women who present to the labour
ward for delivery can be promptly classified based on
these readily available parameters. Specifically, these
categories are11:
(1) Primiparous women with a single cephalic pregnancy, ≥37 weeks’ gestation, in spontaneous labour;
(2) Primiparous women with a single cephalic pregnancy, ≥37 weeks’ gestation, who have induction of labour or CS prior to labour onset;
(3) Multiparous women without a previous uterine scar, with a single cephalic pregnancy of ≥37 weeks’ gestation in spontaneous labour;
(4) Multiparous women without a previous uterine scar, with a single cephalic pregnancy of ≥37 weeks’ gestation, with induction of labour or CS prior to labour onset;
(5) Multiparous women with one or more previous uterine scar(s) and a single cephalic pregnancy of ≥37 weeks’ gestation;
(6) Primiparous women with a single breech pregnancy;
(7) Multiparous women with a single breech pregnancy, with/without previous uterine scar(s);
(8) Women with multiple pregnancies with/without previous uterine scar(s);
(9) Women with a single pregnancy with a transverse or oblique lie, with/without previous uterine scar(s); and
(10) Women with a single cephalic pregnancy at ≤36 weeks’ gestation.
(1) Primiparous women with a single cephalic pregnancy, ≥37 weeks’ gestation, in spontaneous labour;
(2) Primiparous women with a single cephalic pregnancy, ≥37 weeks’ gestation, who have induction of labour or CS prior to labour onset;
(3) Multiparous women without a previous uterine scar, with a single cephalic pregnancy of ≥37 weeks’ gestation in spontaneous labour;
(4) Multiparous women without a previous uterine scar, with a single cephalic pregnancy of ≥37 weeks’ gestation, with induction of labour or CS prior to labour onset;
(5) Multiparous women with one or more previous uterine scar(s) and a single cephalic pregnancy of ≥37 weeks’ gestation;
(6) Primiparous women with a single breech pregnancy;
(7) Multiparous women with a single breech pregnancy, with/without previous uterine scar(s);
(8) Women with multiple pregnancies with/without previous uterine scar(s);
(9) Women with a single pregnancy with a transverse or oblique lie, with/without previous uterine scar(s); and
(10) Women with a single cephalic pregnancy at ≤36 weeks’ gestation.
Despite this increase in CS rates over the years
in both public as well as private sectors, there has
been a paucity of formal surveys on trends in CS
rates in Hong Kong. This study attempted to analyse
the secular trends in CS rates over 20 years at a single
public tertiary training obstetric unit serving a stable
population of around 0.7 to 1 million in the Kowloon
East area. Applying the Robson’s classification to the
data should allow identification of the subgroup(s)
that are predominantly contributing to the steady
increase in overall CS rate. The results of this study
should determine whether the increase in CS rates
is genuinely due to changes in patient epidemiology
and risk factors or merely to changes in obstetric
management.
Methods
The obstetric data from a single obstetric unit
(United Christian Hospital, Kwun Tong) for the last
20 years (1995-2014) were retrieved from the Hospital
Authority (HA) Obstetrics Clinical Information
System. The annual data were supplied to the unit in
an anonymous format with only secondary identifiers
such as medical record number and hospital number.
After compiling this 20-year database, basic patient
characteristics that could constitute important
epidemiological risk factors, such as the proportion
with advanced maternal age of >35 years, percentage
with previous CS or other uterine scars, induction
of labour and multiple pregnancies, were calculated
over the study period.
All cases that underwent CS in our unit during
the study period were classified into one of the 10
groups according to the Robson’s classification,10 11 using prior characteristics or risk factors before
delivery, including primiparous versus multiparous,
preterm versus term, induction of labour versus spontaneous
labour, cephalic presentation versus breech or other
non-cephalic presentation, singleton versus multiple
pregnancy, and previous uterine scar versus no previous
scars. The CS rate of each of the 10 subgroups was
then calculated for each year, and the trends and
changes in the rate over the 20 years were examined.
The total number of patients in each category was
then stratified into four 5-year intervals to compare
the four periods using 4 x 2 contingency tables and
Mantel-Haenszel Chi squared tests for linear trends
for each category. A P value of <0.05 was considered
statistically significant. Significant trends identified
in each category were then compared with observable
trends in patient epidemiological factors over the
same period of time. This study was approved by the
Kowloon Central/Kowloon East Ethics Committee
Board.
Results
There were 86 262 births and 17 140 CSs from
January 1995 to December 2014. The annual
number of deliveries over the 20 years ranged from
3350 in 1995 to 5648 in 2011. The overall CS rate
increased modestly from 15.4% in 1996 to 24.6% in
2014. Parallel with the gradual increase in overall
CS rate, the proportion of elective CS compared
with emergency CS also gradually increased from
25%-30% for 1995-2000 to 40%-45% for 2010-2014,
indicating that an increasing number of CS were
performed electively and the decision was made
well ahead of labour, rather than as an emergency
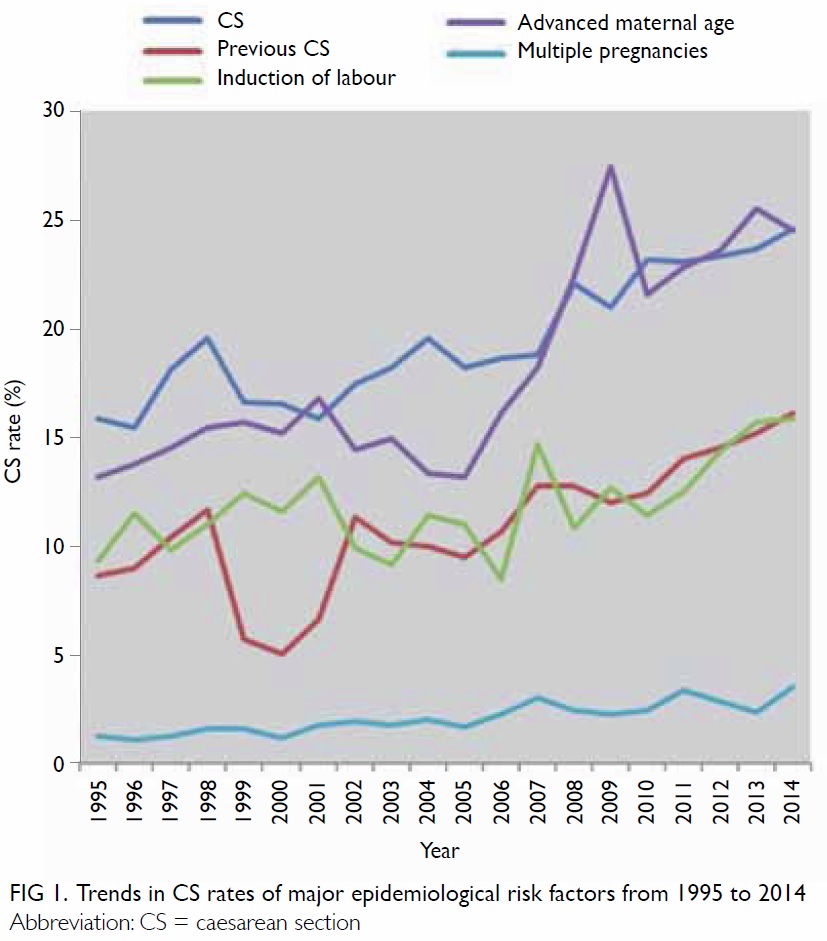
in the intrapartum period. There were significant
increases in the proportion of women with previous
CS (lowest 5% in 2000 to 16.2% in 2014), advanced
maternal age of >35 years (lowest 13.2% in 1995 to
24.5% in 2014), induction of labour (lowest 8.5% in
2006 to 15.9% in 2014), and multiple pregnancies
(1.1% in 1996 to 3.6% in 2014) during the study
period (Fig 1). The crude perinatal mortality rate also
fluctuated between 2.6 and 5.3 per 1000 deliveries;
the adjusted perinatal mortality rate (excluding
those major congenital malformations and birth
weight of <750 g) also varied with an excursion of 1.9
and 3.5 per 1000 deliveries. Due to the small number
variations with absolute crude perinatal mortality
ranging between 10 and 27 per year, however, no
obvious trends were identified during the study. The
maternal mortality rate was lower than 5 per 100 000
pregnancies throughout the two decades with
many years recorded as zero, so no trends could be
observed due to the small variations.
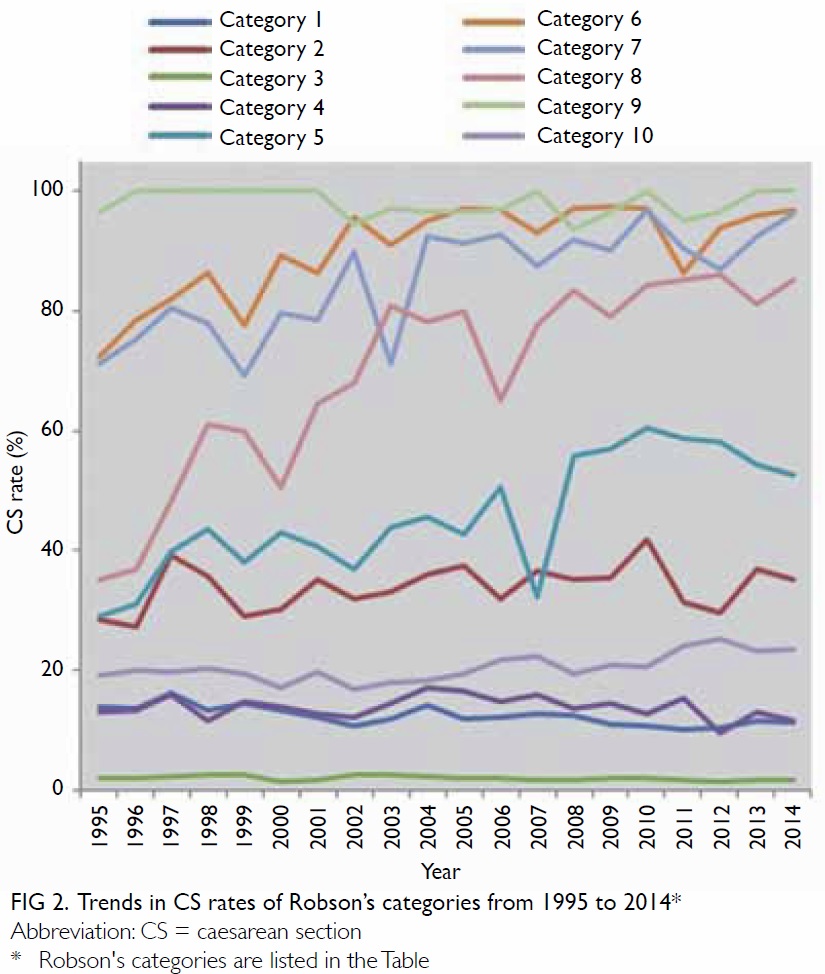
Comparison of the trend in Robson’s categories
1 to 4 for primiparous and multiparous women
with term spontaneous labour (category 1 and 3)
or induced labour or elective CS (category 2 and 4) revealed that the group of primiparous women
with term spontaneous labour (category 1) had a
consistent and gradual fall in CS rate from 14.4%
to 10.8%, while the group of multiparous women
with term spontaneous labour (category 3) also had
a slight fall from 2.1% to 1.6%. The other categories
remained quite stable (Fig 2). On the contrary,
obvious trends showing a dramatic increase in
CS rate were observed in those with previous CS
(category 5, from 29% to 61%), breech presentation at
delivery (category 6 and 7, primiparous from 72% to
97% and multiparous from 69% to 96%), and multiple pregnancy (category 8, from 35% to 86%). Although
the CS rate for abnormal lie or malpresentation
other than breech (category 9) approached 100%
throughout the period and therefore displayed no
significant trend, a subtle increase in CS rate was
seen in those with preterm labour (category 10, from
17% to 25%) [Fig 2]. The data were then stratified into
5-year intervals and the CS rate for each category
compared using a 2 x 4 contingency table. The above
observed trends were confirmed to be statistically
significantly different with P<0.05 for categories 1,
5, 6, 7, 8 and 10 (Table).
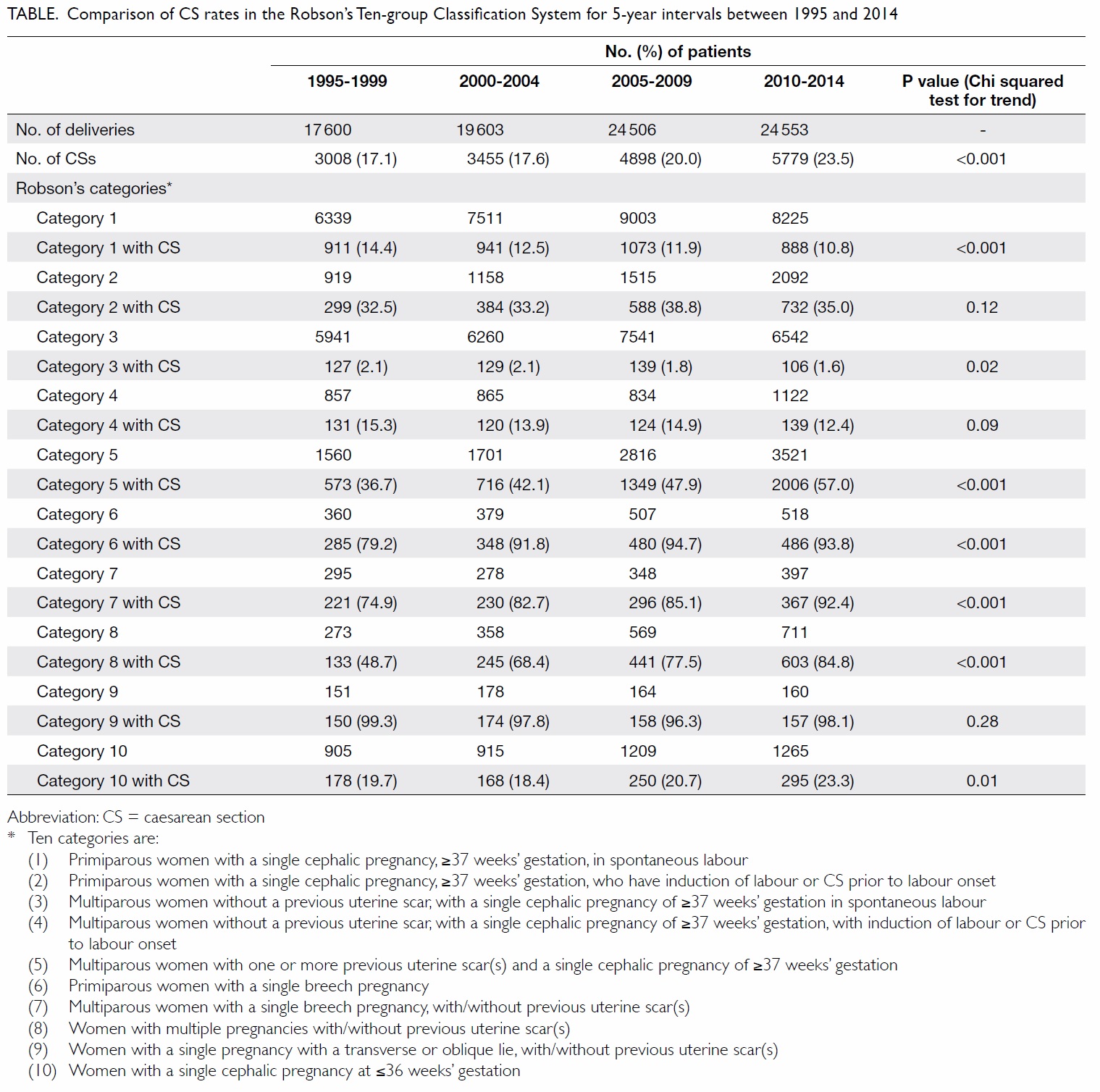
Table. Comparison of CS rates in the Robson’s Ten-group Classification System for 5-year intervals between 1995 and 2014
The data were then reorganised to show the
percentage contribution of each Robson’s category to
the total CS rate for each 5-year interval (Fig 3a). As
there were wide differences in the absolute number
of women in these categories, it could be seen that
the contribution of categories 1, 2, 5, 6 and 8 tended
to overwhelm the contribution of other categories.
Thus, despite the modest fall in CS rates in category
1 over the four interims from approximately 14% to
11%, the impact on reducing the overall CS rates
was predominant over other categories, amounting
to almost 10% of all CS recorded. This effect,
however, was counterbalanced by the contribution
of categories 5 and 8 that increased the CS rates, and
to the accumulated effects on increasing CS rates by
other categories (Fig 3b), so that the net balance was
an overall rise in CS rates from 15% to 24% within
the study period.
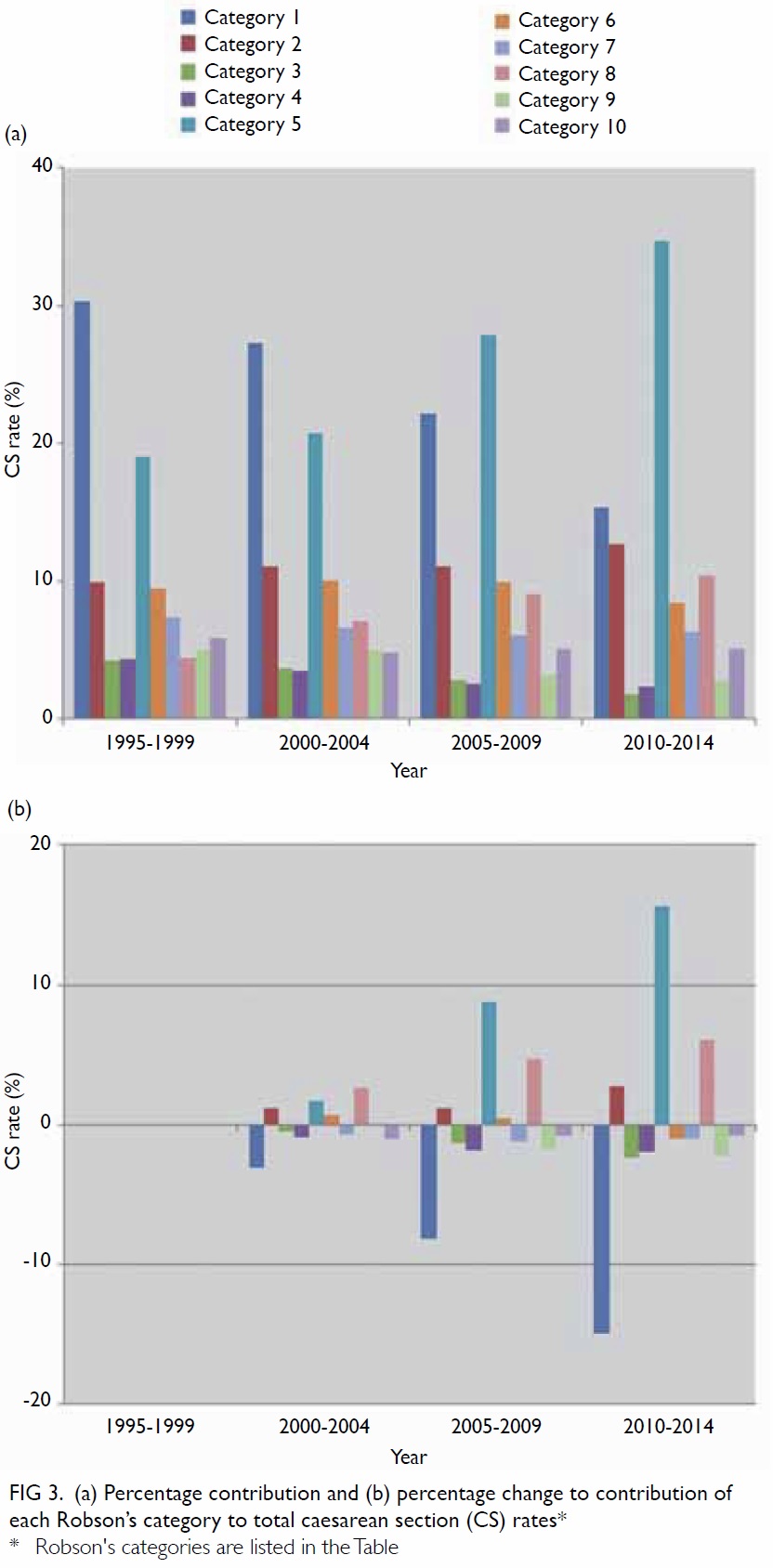
Figure 3. (a) Percentage contribution and (b) percentage change to contribution of each Robson’s category to total caesarean section (CS) rates
Discussion
The data presented above revealed a gradual
increase in overall CS rate of approximately 10%
over the 20-year study period. While there was a
significant reduction in the primary CS rate in low-risk
primiparous women with spontaneous labour,
this was counterbalanced by the ever-increasing CS
rate in those with previous CS, breech presentation,
multiple pregnancies, and to a lesser extent those
with preterm labour. The data have demonstrated
the advantages of using the Robson’s classification to
analyse factors that will influence the overall CS rate.
The use of the Robson’s classification is
increasing rapidly and spontaneously worldwide.
Despite some limitations, the 10-group classification
is easy to implement and interpret.11 12 It allows
standardised comparisons of data across countries
and time points, and identifies the subpopulations
that drive changes in CS rates. The 10-group
classification was easily applied to different levels
of analysis from single-centre to multi-country
datasets without problems of inconsistencies or
misclassification,12 13 14 15 16 enabling specific groups
of women to be clearly identified as the main
contributors to the overall CS rate. Indeed, it has
been demonstrated that this classification can help
health care providers plan practical and effective care
that targets specific groups of women to improve
maternal and perinatal care.13 14 16 17
According to the WHO multi-country survey,9 CS rate was as high as 46% in China, 42% in Paraguay,
and 40% in Ecuador with an overall mean of 26.4%
for the 21 countries in the survey. Incremental rates
as high as 18% within 3 to 4 years and a total CS rate
of up to 80% have been reported in some parts of
China.9 18 In Hong Kong, the annual CS rate rose
steadily from 16.6% to 27.4% from 1987 to 1999,
indicating a 65% increase over 12 years, with the CS
rates in private institutions of approximately 27.4% higher than those in the public sector.4 The Hong
Kong College of Obstetricians and Gynaecologists
territory-wide audit has documented an increase in
overall CS rates in Hong Kong from 27.1% in 1999 to
30.4% in 2004 and 42.1% in 2009,19 a drastic increase
of 12% over a 5-year interval. The annual obstetric report of the HA in 2014 also showed varying CS
rates among the eight public hospitals with obstetric
services, ranging from 22.7% to 32%.20 The overall
increase in CS rates of approximately 10% over the
20-year period to 24%-25% (approximately 0.5% per
year on average) reported in the current study was
modest in rate as well as lower in absolute value
compared with the figures reported above, and those
reported in other countries. The slight drop in CS
rates for primiparous pregnancies with spontaneous
term labour may be an important factor that
mitigates the surge in CS rates in the study period.
Primary caesarean section (categories 1 to 4)
The current data have demonstrated a modest
drop in CS rate for primiparous women with
spontaneous labour (category 1) and a slight fall
in multiparous women with spontaneous labour
(category 3) although the rate for all women with
induced labour or prelabour CS (category 2 and 4)
has remained constant. Review of the labour ward
management protocol in the unit during the study
period revealed that the adoption of evidence-based
active management of labour protocols since
the late 90s (including regular formal audits in CS
rates and indications), the implementation of ‘best
practices’ such as vigilant use of partograms,21 early
amniotomy,22 and prompt oxytocin augmentation
for slow progress23 could have contributed to the
gradual but progressive fall in CS rates in these low-risk
women. Similar measures in labour management
have been shown in cluster-randomised trials to be
associated with significant, albeit small declines
in primary CS rates driven by the effects in low-risk
pregnancies.24 Indeed the magnitude of fall of
1% to 2% in CS rates in such studies was similar to
that observed over the two decades in the current
study. As this category of low-risk primiparous
women with spontaneous labour usually constitutes
approximately ≥30% of the entire obstetric
population, the effects of a modest fall in CS rates
in this group will have a major impact on the overall
rate. Other national studies to evaluate the effect of
labour attempts and labour success on primary CS
rates have shown that the fall in CS rates might not
be persistent. After a slight drop in the late 90s, the
rate started to rise again between 2004 and 2010.25
In addition, other meta-analyses have shown that
the effects of such active management of labour,
while consistently associated with shorter duration
of labour and no discernible differences in neonatal
and maternal outcome, might not be associated
with significant reductions in CS rates.26 It remains
to be seen whether the modest fall in CS rate in
primiparous low-risk women in the current study
will persist in future years. The effects of still other
more drastic attempts to curb primary CS rates in
primiparous women, including redefining labour dystocia,27 postponing the cut-off for active labour at
6-cm dilatation, allowing adequate time for second
stage of labour, and encouraging operative vaginal
delivery28 require further evaluation.
Previous caesarean section (category 5)
The rising proportion of women with previous CS
who undergo repeat CS has been shown by various
studies to contribute significantly to the overall rise
in CS rates. For instance, at a single tertiary hospital
level, it was shown that the Robson’s classification
easily identified multiparous women with a previous
CS scar as the leading patient group that contributed
to an increase in CS rates from 38% in 1998 to 43.7%
in 2011.13 Similarly, on a national scale, a French
population–based study using perinatal survey data
showed that a continuous rise in the CS rate was
observed in three patient groups, one of which was
women with previous CS.16 On an even larger scale, a
WHO global survey of 97 095 women who delivered
in one of 120 facilities in eight countries showed that
although women with a previous CS (category 5)
represented only 11.4% of the obstetric population,
they were the largest contributor to the overall CS
rate (26.7% of all the CSs). This highlights the great
burden of repeat CS and the need to curb primary
CS in order to control CS rates.17 In our study, the
repeat CS rate escalated sharply from approximately
30% to 50%-60% over the two decades. This could
be explained by the abandonment of the use of
X-ray and computed tomographic pelvimetry as a
selection tool 15 years ago to decide which patients
with previous CS can undergo a trial of labour.29 As
evidence accumulated that pelvimetry is imprecise
and fails to predict successful trial of vaginal birth
after CS,30 a liberal policy of allowing women with
previous CS to choose between elective repeat CS
or trial of labour was adopted since 2001. Although
this policy is not based on strong evidence, the
progressive increase in CS rate in this category
indicates the preference of a large proportion of
patients to elect repeat CS based on the relative
indication of previous CS.
Breech presentation (category 6 and 7)
The Term Breech Trial published in 2000 is a good
example of an important landmark study that has
affected clinical protocols adopted by the unit
and thus the CS rates in the study period.31 This
was an authoritative randomised controlled trial
which concluded that planned CS carries a reduced
perinatal mortality and early neonatal morbidity for
babies with breech presentation at term compared
with planned vaginal birth. Although these findings
have been challenged in subsequent studies,32 33 the policy of sectioning all breech babies has been
widely adopted in international guidelines.34 35 Thus,
while the CS rate for breech presentation was already high at approximately 70%-75% at the beginning
of the study period, it increased to well over 90%
in the subsequent 10 to 15 years to comply with
these recommendations. Within this study period,
10%-12% of women with breech presentation at
term opted for external cephalic version (ECV) and
approximately 65% had achieved a successful vaginal
delivery. With better counselling to achieve a higher
acceptance of a trial of ECV, a decline in CS in this
category can be anticipated.
Multiple pregnancies (category 8) and preterm deliveries (category 10)
The policy of allowing women with a twin pregnancy
to opt for CS delivery was even more controversial.
Over 90% of these CS deliveries were elective,
based on maternal choice rather than emergency
intrapartum obstetric indications. Over the 20
years of the study, women with a twin pregnancy in
which one fetus was breech opted for CS in order to
avoid a vaginal breech delivery at all costs, despite
the lack of good clinical supporting evidence if the
first twin is in vertex presentation.36 This further evolved
into a patient expectation that all twin pregnancies
should be sectioned, again despite contrary evidence
from randomised controlled trials that elective CS in
uncomplicated twins offers no perinatal advantage.37
The data from the current study showed that the
liberal clinical policy we have adopted gradually
since 2003 to accommodate such expectations
has resulted in an overwhelming rise in CS rates
in multiple pregnancies from >40% to >80%, far in
excess of that which could be explained by a breech
presentation38 or other risk factors in either twin.
Similarly, the literature has not shown any
particular perinatal survival benefit for CS in
preterm delivery of a cephalic-presenting fetus.39
There is also good evidence that CS delivery at
very early gestations is associated with increased
morbidity in the mother.40 Despite this, we observed
that a large proportion of the increase in preterm CS
was a result of planned iatrogenic preterm deliveries
largely due to specific maternal or fetal conditions
such as pre-eclampsia or early-onset fetal growth
restriction with evidence of fetal compromise. The
modest increase in the use of CS in these cases from
approximately 19% to 23%-24% more likely reflects
the obstetrician’s increasing preference for CS in
the management of these cases rather than women’s
choice. Nevertheless, the increase was modest and
comparable with that reported in other centres.41
Transverse or oblique presentation (category 9)
The overall contribution of this class to the overall
CS rate was low. Stabilising induction after ECV was
performed in only a small number of highly selected cases largely because of the low success rate (<30%),
so that the impact of such a practice on CS rates in
this category was limited. Hence the CS rate in this
class remained high throughout the study period
(>96%).
Strengths and limitations
A strength of the current study was the large sample
size collected over a long duration of two decades to
allow significant trends to be observed. As a single-centre
study, the impact of authoritative scientific
guidelines or a change to liberal management policies
that allowed patients with relative indications to
undergo CS delivery could be readily identified.
Although patient epidemiology, risk factors, and
case-mix were believed to contribute to the rising CS
rates observed within the study period, such effects
were not observed in all categories. For example,
advanced maternal age should have caused an
increase in CS rates for low-risk primiparous women
yet this was not observed. Changes in obstetric
management protocols could also play an important
role in these increasing trends. For instance, the
rising repeat CS rate for women with previous CS
from 36.7% to 57.0% during the study period grossly
exaggerated the absolute increase in the number
of CS performed in women with previous uterine
scars. Liberal rules for multiple pregnancies as
described above were not entirely evidence-based,
but were often adopted to meet patient expectations.
It remained a limitation that we could not test the
temporal relationship of CS trend to changes in
obstetric practice to establish a causal relationship.
In this study, it could be argued that the trends
observed are specific to a public obstetric unit that
did not entertain CS at the mother’s request in
the absence of any clinical indications. However,
CS rates have been observed to rise similarly in all
other HA hospitals as reflected in the HA annual
obstetric reports since 1999. We believe that our
practice is similar to that of other public institutions
in Hong Kong and that our observations can serve
to encourage other obstetric units to audit their own
trends, analyse the extent of rise in each Robson’s
category, and identify the target groups that
contribute most significantly to the rise in CS rates.
Appropriate changes may then be made to clinical
management protocols.
Conclusion
The most significant trends in an increase in CS rates
were in line with the clinical practice towards CS for
those with relative indications such as previous CS,
breech presentation, and multiple pregnancies. The
drop in CS rates for primiparous pregnancies with
spontaneous term labour could be ascribed to more
vigilant active labour management, and because the large absolute number in this group had the effect of
mitigating the overall surge in CS rates. The overall
increase in CS rates of approximately 10% over the
20-year period was modest compared with figures
reported previously in Hong Kong and in other
developed countries.
Declaration
All authors have disclosed no conflicts of interest.
References
1. Betran AP, Torloni MR, Zhang J, et al. What is the optimal
rate of caesarean section at population level? A systematic
review of ecologic studies. Reprod Health 2015;12:57. Crossref
2. Belizán JM, Althabe F, Cafferata ML. Health consequences
of the increasing caesarean section rates. Epidemiology
2007;18:485-6. Crossref
3. Betrán AP, Ye J, Moller AB, Zhang J, Gülmezoglu AM,
Torloni MR. The increasing trend in caesarean section
rates: global, regional and national estimates: 1990-2014.
PLoS ONE 2016;11:e0148343. Crossref
4. Leung GM, Lam TH, Thach TQ, Wan S, Ho LM. Rates
of cesarean births in Hong Kong: 1987-1999. Birth
2001;28:166-72. Crossref
5. Notzon FC. International differences in the use of obstetric
interventions. JAMA 1990;263:3286-91. Crossref
6. Appropriate technology for birth. Lancet 1985;2:436-7.
7. Villar J, Valladares E, Wojdyla D, et al. Caesarean delivery
rates and pregnancy outcomes: the 2005 WHO global
survey on maternal and perinatal health in Latin America.
Lancet 2006;367:1819-29. Crossref
8. Lumbiganon P, Laopaiboon M, Gulmezoglu AM, et al.
Method of delivery and pregnancy outcomes in Asia: the
WHO global survey on maternal and perinatal health
2007-08. Lancet 2010;375:490-9. Crossref
9. Vogel JP, Betrán AP, Vindevoghel N, et al. Use of the Robson
classification to assess caesarean section trends in 21
countries: a secondary analysis of two WHO multicountry
surveys. Lancet Glob Health 2015;3:e260-70. Crossref
10. Robson MS. Classification of caesarean sections. Fetal
Matern Med Rev 2001;12:23-39. Crossref
11. Betrán AP, Vindevoghel N, Souza JP, Gülmezoglu
AM, Torloni MR. A systematic review of the Robson
classification for caesarean section: what works, doesn’t
work and how to improve it. PLoS One 2014;9:e97769. Crossref
12. Torloni MR, Betran AP, Souza JP, et al. Classifications
for cesarean section: a systematic review. PLoS One
2011;6:e14566. Crossref
13. Triunfo S, Ferrazzani S, Lanzone A, Scambia G.
Identification of obstetric targets for reducing cesarean
section rate using the Robson ten group classification in
a tertiary level hospital. Eur J Obstet Gynecol Reprod Biol
2015;189:91-5. Crossref
14. Colais P, Fantini MP, Fusco D, et al. Risk adjustment models
for interhospital comparison of CS rates using Robson’s ten
group classification system and other socio-demographic
and clinical variables. BMC Pregnancy Childbirth
2012;12:54. Crossref
15. Stavrou EP, Ford JB, Shand AW, Morris JM, Roberts CL.
Epidemiology and trends for caesarean section births in
New South Wales, Australia: a population-based study.
BMC Pregnancy Childbirth 2011;11:8. Crossref
16. Le Ray C, Blondel B, Prunet C, Khireddine I, Deneux-Tharaux C, Goffinet F. Stabilising the caesarean rate: which
target population? BJOG 2015;122:690-9. Crossref
17. Betrán AP, Gulmezoglu AM, Robson M, et al. WHO global
survey on maternal and perinatal health in Latin America: classifying caesarean sections. Reprod Health 2009;6:18. Crossref
18. Huang K, Tao F, Bogg L, Tang S. Impact of alternative
reimbursement strategies in the new cooperative medical
scheme on caesarean delivery rates: a mixed-method study
in rural China. BMC Health Serv Res 2012;12:217. Crossref
19. Yuen PM. Territory-wide audit in obstetrics and
gynaecology 2014. Available from: http://www.hkcog.org.hk/hkcog/pages_3_77.html. Accessed Feb 2017.
20. Annual obstetric report 2014. Hong Kong: Hospital
Authority; 2014.
21. Cox KJ, King TL. Preventing primary caesarean births:
midwifery care. Clin Obstet Gynecol 2015;58:282-93. Crossref
22. Wei S, Wo BL, Qi HP, et al. Early amniotomy and early
oxytocin for prevention of, or therapy for, delay in first
stage spontaneous labour compared with routine care.
Cochrane Database Syst Rev 2013;(8):CD006794. Crossref
23. Bugg GJ, Siddiqui F, Thornton JG. Oxytocin versus no
treatment or delayed treatment for slow progress in the
first stage of spontaneous labour. Cochrane Database Syst
Rev 2013;(6):CD007123. Crossref
24. Chaillet N, Dumont A, Abrahamowicz M, et al. A cluster-randomized
trial to reduce cesarean delivery rates in
Quebec. N Engl J Med 2015;372:1710-21. Crossref
25. Simon AE, Uddin SG. National trends in primary cesarean
delivery, labor attempts, and labor success, 1990-2010. Am
J Obstet Gynecol 2013;209:554.e1-8. Crossref
26. Brown HC, Paranjothy S, Dowswell T, Thomas J. Package
of care for active management in labour for reducing
caesarean section rates in low-risk women. Cochrane
Database Syst Rev 2013;(9):CD004907. Crossref
27. Boyle A, Reddy UM, Landy HJ, Huang CC, Driggers RW,
Laughon SK. Primary cesarean delivery in the United
States. Obstet Gynecol 2013;122:33-40. Crossref
28. American College of Obstetricians and Gynecologists, Society for Maternal–Fetal Medicine, Caughey
AB, Cahill AG, Guise JM, Rouse DJ. Safe prevention of
the primary cesarean delivery. Am J Obstet Gynecol
2014;210:179-93. Crossref
29. Pattinson RC, Farrell EM. Pelvimetry for fetal cephalic
presentations at or near term. Cochrane Database Syst Rev
1997;(2):CD000161. Crossref
30. Dodd JM, Crowther CA, Huertas E, Guise JM, Horey D.
Planned elective repeat caesarean section versus planned
vaginal birth for women with a previous caesarean birth.
Cochrane Database Syst Rev 2013;(12):CD004224. Crossref
31. Hannah ME, Hannah WJ, Hewson SA, Hodnett ED, Saigal
S, Willan AR. Planned caesarean section versus planned
vaginal birth for breech presentation at term: a randomised
multicentre trial. Term Breech Trial Collaborative Group.
Lancet 2000;356:1375-83. Crossref
32. Whyte H, Hannah ME, Saigal S, et al. Outcomes of
children at 2 years after planned cesarean birth versus
planned vaginal birth for breech presentation at term: the
International Randomized Term Breech Trial. Am J Obstet
Gynecol 2004;191:864-71. Crossref
33. Hannah ME, Whyte H, Hannah WJ, et al. Maternal
outcomes at 2 years after planned cesarean section versus
planned vaginal birth for breech presentation at term: the
International Randomized Term Breech Trial. Am J Obstet
Gynecol 2004;191:917-27. Crossref
34. Committee on Obstetric Practice. ACOG committee
opinion: number 265, December 2001. Mode of term
single breech delivery. Obstet Gynecol 2001;98:1189-90. Crossref
35. Royal College of Obstetricians and Gynaecologists.
RCOG Green-top Guidelines: The management of breech
presentation. Guideline No. 20b. December 2006. Available
from: https://www.rcog.org.uk/globalassets/documents/guidelines/gtg-no-20b-breech-presentation.pdf. Accessed
Feb 2017.
36. Rabinovici J, Barkai G, Reichman B, Serr DM, Mashiach S.
Randomized management of the second nonvertex twin: vaginal delivery or cesarean section. Am J Obstet Gynecol
1987;156:52-6. Crossref
37. Barrett JF, Hannah ME, Hutton EK, et al. A randomized
trial of planned cesarean or vaginal delivery for twin pregnancy. N Engl J Med 2013;369:1295-305. Crossref
38. Lee HC, Gould JB, Boscardin WJ, El-Sayed YY, Blumenfeld
YJ. Trends in cesarean delivery for twin births in the
United States: 1995-2008. Obstet Gynecol 2011;118:1095-101. Crossref
39. Riskin A, Riskin-Mashiah S, Lusky A, Reichman B; Israel
Neonatal Network. The relationship between delivery
mode and mortality in very low birthweight singleton
vertex-presenting infants. BJOG 2004;111:1365-71. Crossref
40. Malloy MH. Impact of cesarean section on neonatal
mortality rates among very preterm infants in the United
States, 2000-2003. Pediatrics 2008;122:285-92. Crossref
41. Biswas A, Su LL, Mattar C. Caesarean section for preterm
birth and, breech presentation and twin pregnancies. Best
Pract Res Clin Obstet Gynaecol 2013;27:209-19. Crossref