DOI: 10.12809/hkmj165045
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
MEDICAL PRACTICE CME
2016 Consensus statement on prevention of atherosclerotic cardiovascular disease in the
Hong Kong population
Bernard MY Cheung, MB BChir (Cantab), PhD (Cantab)1;
CH Cheng, MB, BS2;
CP Lau, MB, BS, MD3;
Chris KY Wong, MB, ChB (Glasg)4;
Ronald CW Ma, MB BChir (Cantab)5;
Daniel WS Chu, MB, BS (NSW)2;
Duncan HK Ho, MB, BS4;
Kathy LF Lee, MB, BS2;
HF Tse, MD, PhD1;
Alexander SP Wong, MB, BS2;
Bryan PY Yan, MB, BS5;
Victor WT Yan, MB, BS2
1 Department of Medicine, The University of Hong Kong, Queen Mary
Hospital, Pokfulam, Hong Kong
2 Private practice, Hong Kong
3 Institute of Cardiovascular Science and Medicine, The University of Hong Kong, Pokfulam, Hong Kong
4 Hong Kong Sanatorium & Hospital, Happy Valley, Hong Kong
5 Department of Medicine and Therapeutics, The Chinese University of Hong Kong, Prince of Wales Hospital, Shatin, Hong Kong
Corresponding author: Prof Bernard MY Cheung (mycheung@hku.hk)
Abstract
Introduction: In Hong Kong, the prevalence of
atherosclerotic cardiovascular disease has increased
markedly over the past few decades, and further
increases are expected. In 2008, the Hong Kong
Cardiovascular Task Force released a consensus
statement on preventing cardiovascular disease
in the Hong Kong population. The present article
provides an update on these recommendations.
Participants: A multidisciplinary group of clinicians
comprising the Hong Kong Cardiovascular Task
Force—10 cardiologists, an endocrinologist, and a
family physician—met in September 2014 and June
2015 in Hong Kong.
Evidence: Guidelines from the American College
of Cardiology/American Heart Association, the
European Society of Hypertension/European
Society of Cardiology, and the Eighth Joint National
Committee for the Management of High Blood
Pressure were reviewed.
Consensus Process: Group members reviewed
the 2008 Consensus Statement and relevant
international guidelines. At the meetings, each
topical recommendation of the 2008 Statement was
assessed against the pooled recommendations on
that topic from the international guidelines. A final
recommendation on each topic was generated by
consensus after discussion.
Conclusions: It is recommended that a formal risk
scoring system should be used for risk assessment
of all adults aged 40 years or older who have at least
one cardiovascular risk factor. Individuals can be
classified as having a low, moderate, or high risk of
developing atherosclerotic cardiovascular disease,
and appropriate interventions selected accordingly.
Recommended lifestyle modifications include
adopting a healthy eating pattern; maintaining a low
body mass index; quitting smoking; and undertaking
regular, moderate-intensity physical activity.
Pharmacological interventions should be selected as
appropriate after lifestyle modification.
Introduction
Atherosclerotic cardiovascular disease (ASCVD),
which includes coronary heart disease (CHD),
peripheral vascular disease and stroke, is currently
one of the most common causes of morbidity and
mortality worldwide.1 Unfortunately the prevalence
of ASCVD is expected to increase further over
the next few decades due to a number of factors
including an ageing population and increasing
industrialisation. The latter is associated with
increased exposure to known ASCVD risk factors
such as smoking, low levels of physical activity, and
poor dietary habits such as reduced consumption
of fruit and vegetables and increased fat and salt
intake.2
In Hong Kong, the prevalence of ASCVD risk
factors has increased markedly over the past few
decades. For example, the 2005-2008 Hong Kong
Cardiovascular Risk Factor Prevalence Study-3
(CRISPS-3) reported an 8.6% increase in the
prevalence of abdominal obesity (waist circumference
≥90 cm in men and ≥80 cm in women) and a 21.5%
increase in the prevalence of hypertension among
a cohort of 1803 subjects recruited from CRISPS-1, the first such survey conducted between 1995
and 1996.3 Of the 551 participants of the Hong
Kong Cardiovascular Task Force Risk Management
Programme, 65.4% had hypertension, 63.7%
dyslipidaemia, and 33.3% diabetes at baseline (BMY
Cheung, unpublished data).
Global efforts are underway to promote
ASCVD prevention and reduce the risk of major
ASCVD events. These efforts have yielded benefits—between 1990 and 2013, a substantial reduction in
cardiovascular mortality was seen in central Europe
(5.2%) and western Europe (12.8%), attributed
primarily to birth cohorts’ decreased exposure to
tobacco smoking, improvements in diet, improved
treatment of cardiometabolic risk factors, and
improved treatment of CVD.4
Methods
A multidisciplinary group of clinicians comprising
the Hong Kong Cardiovascular Task Force—10
cardiologists, an endocrinologist, and a family
physician—met in September 2014 and June 2015
in Hong Kong with the aim of updating the first
Consensus Statement on Preventing Cardiovascular
Disease in the Hong Kong Population published
in 2008.5 Prior to the consensus meetings, group
members reviewed the 2008 Consensus Statement
and relevant guidelines from the American College
of Cardiology/American Heart Association, the
European Society of Hypertension/European
Society of Cardiology, and the Eighth Joint National
Committee for the Management of High Blood
Pressure, among others.5 6 7 8 9 At the meetings, each topical recommendation of the 2008 Statement
was assessed against the pooled recommendations
on that topic from the international guidelines
reviewed. A final recommendation on each topic
was generated by consensus after discussion.
The recommendations included in this
consensus statement constitute the consensus
opinion of the members of the Hong Kong
Cardiovascular Task Force regarding the most
appropriate interventions for the Hong Kong
population.
Recommendations
Risk assessment
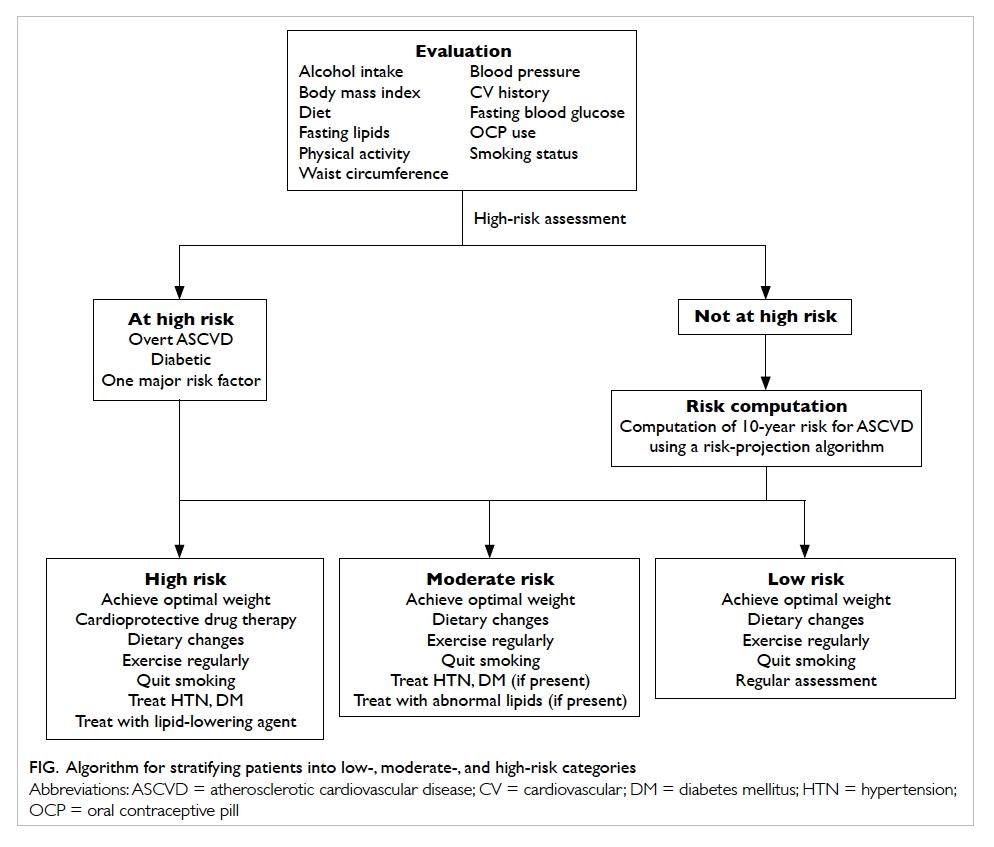
Total cardiovascular risk
Total ASCVD risk is based on the complex
interactions of a number of different risk factors
that together have a multiplicative effect. That is,
the risk of ASCVD is amplified to a greater extent
by the interaction of multiple risk factors than would
be expected due to the cumulative effect of each risk
factor alone.7 9 The present standard of practice for the primary prevention of ASCVD is to determine
a patient’s total ASCVD risk using a formal risk
scoring algorithm.1 7 9
Who to assess?
In Hong Kong, it is recommended that ASCVD
prevention efforts should be focused on adults aged
40 years or older who have at least one ASCVD risk
factor.1 9 The total ASCVD risk should be formally calculated for such individuals, and they should
receive ASCVD prevention advice and/or treatment
according to their determined level of risk (high,
moderate, or low).1 9 High-risk patients will benefit most from treatment and include:
- patients with overt ASCVD (CHD, previous myocardial infarction, previous stroke, or peripheral vascular disease) or those who are symptomatic (eg have experience with angina)
- patients with diabetes mellitus
- patients with one major ASCVD risk factor (eg moderate-to-severe hypertension, severely elevated lipid levels)9
These patients automatically meet the
threshold for intensive risk factor treatment and
need not undergo formal risk scoring.1 9
How to assess?
It is important to note that the current
recommendations do not espouse a preference
for any particular method of risk projection, but
recommend that formal ASCVD risk scoring should
be performed for all potentially at-risk patients.
A patient’s 10-year (total) risk for ASCVD may
be calculated using a variety of methods. The most
recently published algorithm uses the American
Pooled Cohort Risk Assessment Equations that are
sex- and race-specific estimates for African-American
and White men and women aged 40 to 79 years.
They utilise age, total and high-density lipoprotein
(HDL) cholesterol, systolic blood pressure (BP),
diabetes, and current smoking status to calculate
the total ASCVD risk.1 The European Systematic
Coronary Risk Evaluation (SCORE) system is another
well-validated system that uses sex, age, systolic
BP, total cholesterol, and current smoking status
to predict the risk of fatal cardiovascular events.7
Another risk assessment system, QRISK2, includes
the risk factor of ‘self-assigned ethnicity’ (including
Chinese) in the computation10 11; however, the model was validated for Chinese immigrants to the United Kingdom and,
thus, its applicability to the local Chinese population
is unknown.
The calculated risk score is used to stratify
patients into low-, moderate-, and high-risk
categories (Fig). When interpreting these scores,
the clinician should bear in mind that they were
developed and validated for western populations. In
addition, it must be remembered that any calculated
ASCVD score is simply an indicator of total
cardiovascular risk.9 Although it can guide patient
treatment, it cannot be a substitute for individualised
patient evaluation and management. The clinician is
advised to take all factors into account and to treat
the patient individually rather than treat the risk
score.
Risk interventions
There is robust scientific evidence that the
development of ASCVD in at-risk patients
may be slowed and/or prevented by lifestyle
modification, reduction of metabolic risk factors,
and pharmacological treatment.7 9 10 11 12 13 14 15 16 17 18 19 Listed below are
the major modifiable risk factors for ASCVD. The
treatment goal is stated for each risk factor, along with
general recommendations on how this goal may be
achieved. Existing hypertension,7 8 dyslipidaemia,1 6 and diabetes20 21 22 treatment guidelines incorporate
the latest evidence on how to treat these conditions
and to what appropriate targets. The clinician is
referred to these guidelines for further guidance.
Diet
Treatment goal: an overall healthy eating pattern
All patients at increased risk of ASCVD should be
given advice and specific recommendations for
eating a healthy diet. Advice should include9:
- matching energy intake with energy needs;
- eating a variety of fruits, vegetables, grains, low- or non-fat dairy products, legumes, fish, poultry, and lean meats;
- reducing saturated and trans fats to <10% of total daily caloric intake, through replacement with polyunsaturated fats (vegetables, nuts, seeds, and seafood);
- reducing cholesterol intake;
- reducing salt intake; and
- limiting alcohol intake to no more than two drinks per day for men and one drink per day for women.
Physical activity
Treatment goal: a minimum of 30 minutes of
moderate-intensity physical activity at least 5 times
a week, or a minimum of 15 minutes of vigorous-intensity
physical activity at least 5 times a week9
- ‘Moderate intensity’ is defined as exercising at 64% to 76% of maximum heart rate (ie 220 minus age); activities include brisk walking, slow cycling, vacuuming, gardening, golf, tennis (doubles), ballroom dancing, and water aerobics.9 ‘Vigorous intensity’ is defined as exercising at 77% to 93% of maximum heart rate; activities include race walking, jogging or running, bicycling, heavy gardening, swimming laps, and tennis (singles).9
- The practice of the popular Chinese soft martial art tai chi may also be beneficial for individuals at risk of ASCVD. A systematic review has shown that tai chi has physiological and psychosocial benefits, and it also appears to be safe and effective in promoting flexibility, balance control, and cardiovascular fitness in older patients with chronic conditions.23
- All patients should consult their doctor prior to initiating graded exercise programmes.
Overweight/obesity
Treatment goal: maintenance of normal body mass
index and waist circumference
- Normal body mass index is 18.5-22.9 kg/m2 for Asians,24 and normal waist circumference is <90 cm (35.4 inches) for men and <80 cm (31.5 inches) for women.25
- Patients who are overweight or obese should strive to achieve normal body weight by restricting caloric intake and increasing physical activity.
- Drug therapy or surgical interventions may be a helpful adjunct for the treatment of severe obesity in some patients.
Smoking
Treatment goal: complete smoking cessation
- Assess the patient’s tobacco use and strongly urge the patient to stop smoking.
- Determine the patient’s degree of nicotine addiction and his/her readiness to quit smoking. For patients identified as willing to quit, a plan should be developed that may involve pharmacotherapy, counselling, cessation support mechanisms (eg follow-up calls and visits), and referral to specialised programmes, if available.20 26
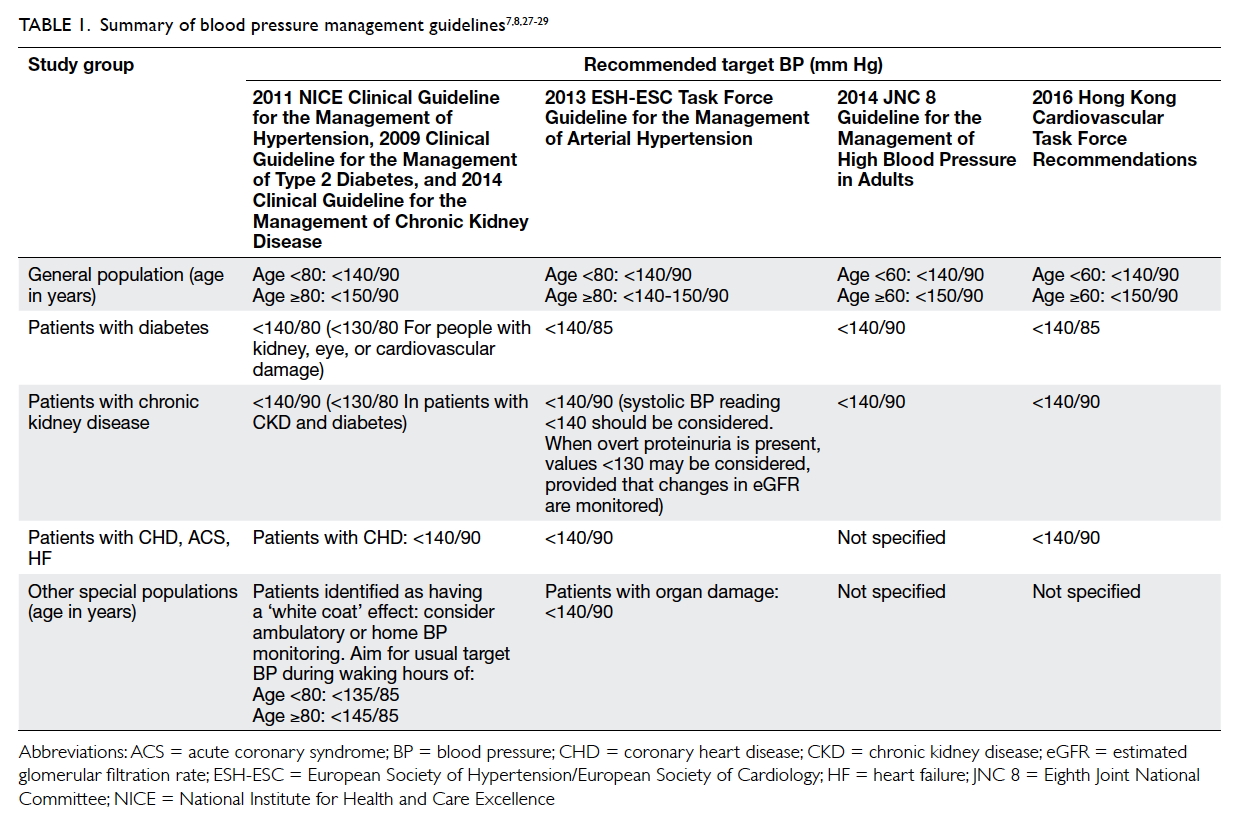
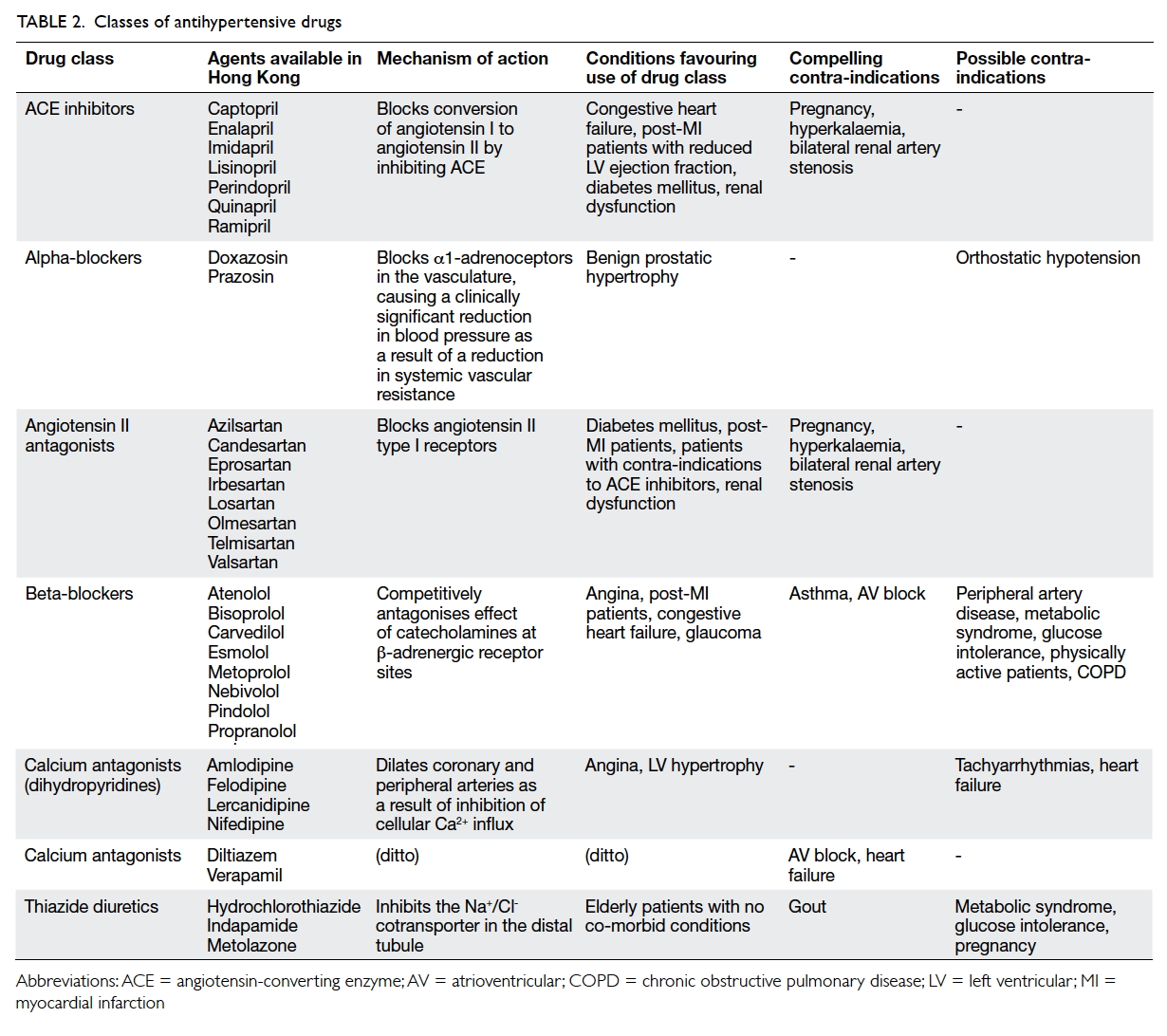
Hypertension
Risk factor reduction goal: blood pressure of <140/90
mm Hg for the general population aged <60 years,
including patients with previous stroke or transient
ischaemic attack; patients with coronary heart disease; and patients with chronic kidney disease.
For patients with diabetes, a target blood pressure
of <140/85 mm Hg is recommended. For the general
population aged ≥60 years, a target blood pressure
of <150/90 mm Hg is recommended7 8 9
- Patients with a systolic BP of ≥130 mm Hg or diastolic BP of ≥80 mm Hg should be given advice and specific recommendations on reducing lifestyle risk factors.
- Patients who do not meet their primary goals as defined above should be given drug therapy tailored to their circumstances.
- The choice of first-line therapy is the prerogative of the attending physician. Suitable antihypertensive drugs include calcium channel blockers, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin receptor blockers (ARBs), either alone or in combination (Tables 1 and 2).7 9 Diuretics (chlorthalidone and indapamide) and β-blockers may also be used, but their long-term use is associated with increased risk of new-onset diabetes30 31; of note, there is no evidence that hydrochlorothiazide—one of the most commonly prescribed antihypertensives—in its usual dose of 12.5 to 25 mg daily reduces myocardial infarction, stroke, or death.32
- When target BP cannot be achieved with monotherapy or with a two-drug combination, doses can be increased; if target BP cannot be achieved by a two-drug combination at full doses, switching to another two-drug combination, or adding a third drug, may be considered.7 8 9 In patients with uncontrolled BP despite treatment with maximally tolerated doses of three antihypertensive medications, addition of the aldosterone antagonist spironolactone has achieved larger reductions in systolic BP than addition of the β-blocker bisoprolol, the alpha-adrenergic blocker doxazosin, or placebo.33
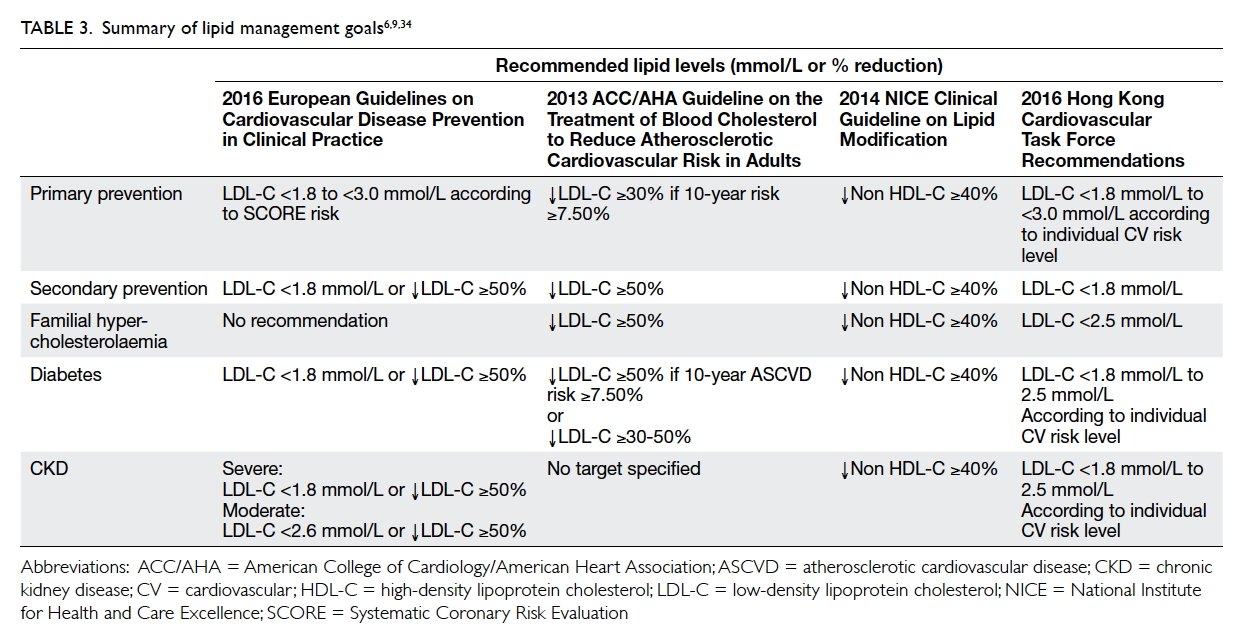
Dyslipidaemia
Risk factor reduction goal: low-density lipoprotein
cholesterol level of <3 mmol/L. For patients with
overt atherosclerotic cardiovascular disease, the
target level should be <1.8 mmol/L9
- Low-density lipoprotein cholesterol (LDL-C) reduction decreases cardiovascular events.9
- Recommended target LDL-C level for patients stratified by ASCVD risk is as follows:
- Very high ASCVD risk: LDL-C <1.8 mmol/L, or a ≥50% reduction if the baseline is between 1.8 and 3.5 mmol/L (Table 3)
- High ASCVD risk: LDL-C <2.6 mmol/L, or a ≥50% reduction if the baseline is between 2.6 and 5.1 mmol/L
- Low-to-moderate ASCVD risk: LDL-C <3.0 mmol/L9
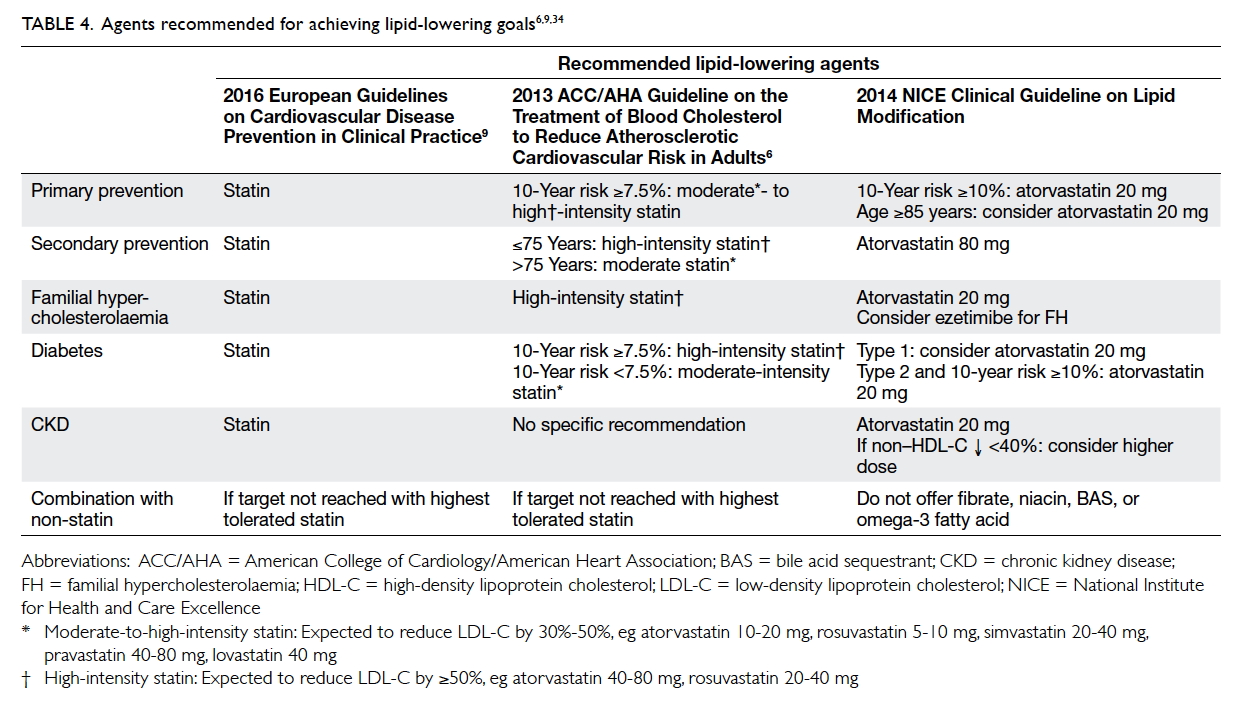
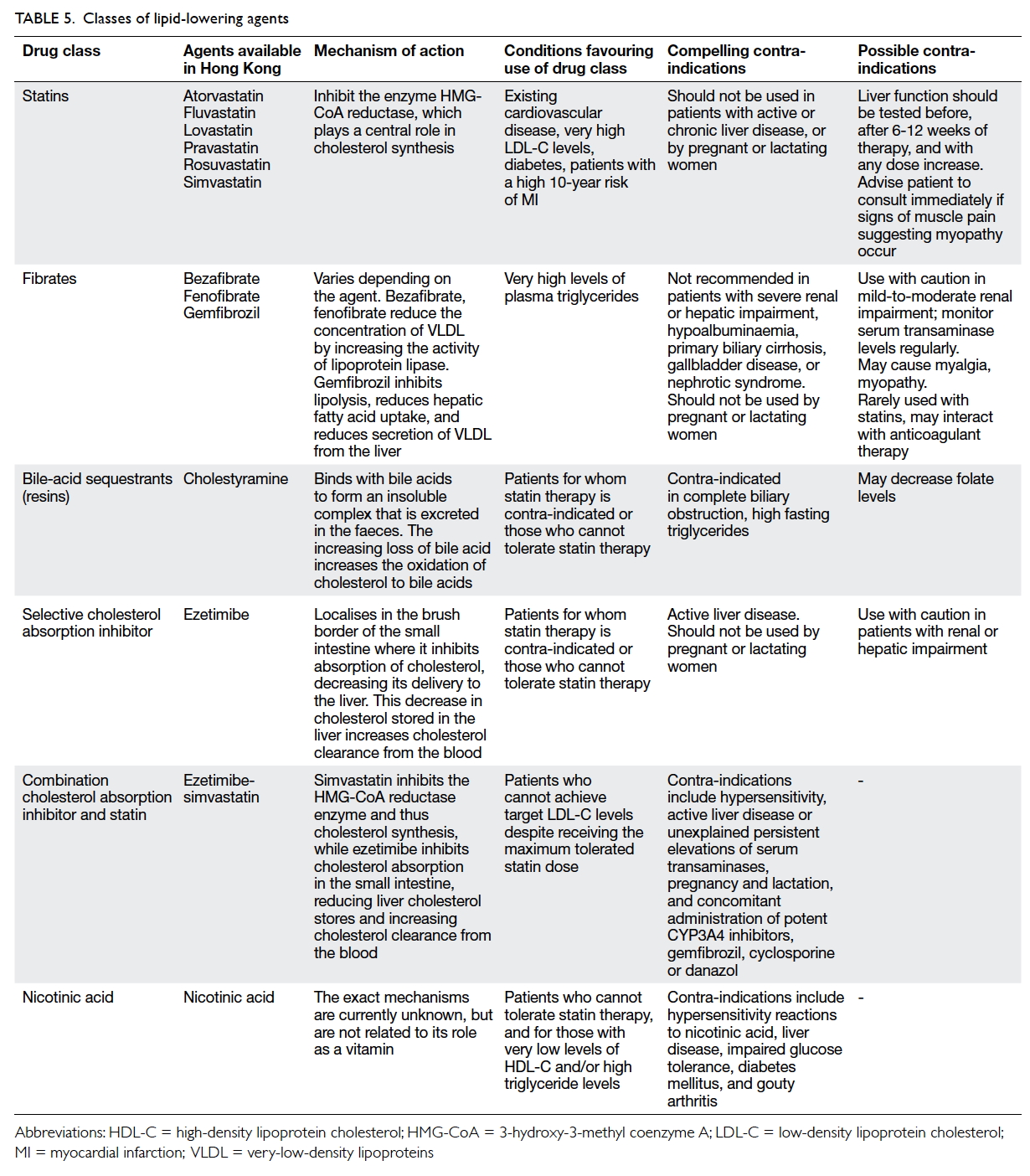
- Patients at low and moderate risk should be given advice and specific recommendations on lowering LDL-C through dietary adjustments, increased physical activity, and weight reduction. If the target is not met after 6 months, they should be given a lipid-lowering agent (Tables 4 and 5).35
- Patients at high risk should immediately be started on lipid-lowering therapy with a high-intensity statin (Tables 4 and 5).35 Importantly, however, pharmacokinetic studies have shown that Chinese patients achieve a higher plasma concentration of statin compared with Caucasians, and this may be associated with an increased risk of adverse effects.36 Consequently, the maximum approved doses of the statins available in Asia are around half the maximum approved doses in the United States.37 The clinician should, therefore, exercise caution when prescribing high-intensity statin therapy.
- Inhibitors of proprotein convertase subtilisin/kexin type 9 have recently been approved for use in the United Kingdom and the United States as an adjunct to diet and maximally tolerated statin therapy for the treatment of individuals with primary hypercholesterolaemia or mixed dyslipidaemia, or those with clinical ASCVD who require additional lowering of LDL-C.38 39 Clinical trials have demonstrated decreases in LDL-C by up to 60% in subjects receiving these agents38; definitive evidence of reduced cardiovascular event rates associated with their use may be provided by ongoing trials.
Diabetes
- All diabetic patients are considered high risk for the development of ASCVD9 21 and should receive appropriate management upon diagnosis. This includes guidance on diet modification and increased physical activity in conjunction with pharmacotherapy.20 21 22 Early initiation of medication is recommended to avoid any delay in treatment. Insulin is administered if treatment goals are not achieved with oral therapy.20 21 22 Treatment goal for glycaemia should be tailored according to the patient profile in order to avoid hypoglycaemia in those with co-morbidities or in elderly patients.22 40
- In diabetic patients, treat other ASCVD risk factors more aggressively,22 including hypertension. Nevertheless, present evidence suggests that a BP target of <140/85 mm Hg is appropriate in patients with diabetes, with a lower BP (systolic BP of <130 mm Hg) as an option in patients with hypertension and nephropathy. It should be noted that lower BP may be associated with increased risk of adverse events, especially in older patients or those with a long duration of diabetes, and the risk and benefit of intensive BP lowering needs to be considered individually according to the patient profile.22
Discussion
The gap between evidence and practice
Although clear, evidence-based guidelines and
recommendations for ASCVD prevention have
been available for a number of years and are
regularly updated, there is evidence that they are
not routinely implemented in clinical practice.9 41 42
For example, Yusuf et al43 reported worldwide poor
use of medications for the secondary prevention of
ASCVD. Their study included 153 996 adults aged
35 to 70 years from rural and urban communities
in high-, upper-middle–, lower-middle–, and
low-income countries, 5650 of whom had had a
self-reported CHD event and 2292 a stroke. Few
individuals with ASCVD took antiplatelet drugs
(25.3%), β-blockers (17.4%), ACE inhibitors or ARBs
(19.5%), or statins (14.6%). As expected, drug use
was higher in high-income countries, with 11.2% of
patients in these countries not receiving any drugs
compared with 45.1% of patients in upper-middle–income
countries, 69.3% in lower-middle–income
countries, and 80.2% in low-income countries.
Notably, despite the relative accessibility of drugs
for secondary prevention of ASCVD in high- and
upper-middle–income countries, many patients
remained untreated.
Of the patients who do receive treatment for
ASCVD risk factors, only a few attain their treatment
goals. Findings from the Hong Kong Cardiovascular
Task Force Risk Management Programme indicate
that 84% of enrolled hypertensive patients were
treated with one or two antihypertensive drugs,
most commonly ARBs (63.5%) and calcium channel
blockers (47.2%; BMY Cheung, unpublished data).
Similarly 64% of the diabetic patients were treated
with metformin (68.8%) and/or gliptins (36%), while
78.1% of patients with dyslipidaemia were treated
with a statin. Notably, however, treatment goals for
hypertension (<130/80 mm Hg for diabetic patients,
<140/90 mm Hg for non-diabetics) and diabetes
(glycated haemoglobin <7%) were met by just over
50% of hypertensive patients and approximately 60%
of diabetics.
Ensuring physician compliance with
evidence-based guidelines and improving clinician
understanding of factors affecting patient compliance
with treatment may be the key to decreasing ASCVD
risk in the Hong Kong population.
Differences between the 2008 and 2016
consensus statements
The present update of the 2008 Consensus
Statement introduces the use of the new American
Pooled Cohort Risk Assessment Equations that
have superseded the Framingham Risk Evaluation;
ASCVD risk can be assessed using either these
equations or the European SCORE system to
stratify patients into low-, moderate-, or high-risk
categories to aid targeting of therapies as well as
the establishment of suitable treatment goals. The
risk factor reduction goals for hypertension and
dyslipidaemia have been updated to reflect the
most current recommendations from the Eighth
Joint National Committee, the European guidelines
on the management of arterial hypertension, and
the European guidelines on cardiovascular disease
prevention in clinical practice. The HDL-C target
included in the 2008 Consensus Statement has
been omitted from the current update as increased
HDL-C has not been proven to reduce ASCVD risk.
Conclusions
The development of ASCVD in at-risk patients
may be slowed and/or prevented by lifestyle
modification, reduction of metabolic risk factors,
and pharmacological treatment. The clinician plays
a central role in ASCVD prevention—identifying
at-risk patients, calculating the total ASVCD risk
score, encouraging lifestyle changes, and providing
targeted interventions to achieve specific treatment
goals. Nonetheless, it is vital that the clinician is not
overly focused on the treatment of isolated ASCVD
risk factors but should instead adopt a ‘whole-person’
approach to diagnosis and therapy. Many
patients present with multiple risk factors and,
therefore, individualised, nuanced patient evaluation
and management is essential to achieve optimum
outcomes. Finally, none of these interventions will
result in ASVCD prevention without the cooperation
of the patient. Clinicians are encouraged to build
strong partnerships with their patients, with the
aim of establishing individual ownership of their
treatment plans and, thus, improved treatment
compliance.
Acknowledgements
The authors would like to acknowledge Ms Lianne
Cowie and Dr Jose Miguel (Awi) Curameng of
MIMS (Hong Kong) Limited for providing editorial
and writing support, which was funded by Pfizer
Corporation Hong Kong Limited. The meetings
during which these consensus points were formulated
and discussed were supported by an unrestricted
educational grant from Pfizer Corporation Hong
Kong Limited.
Declaration
Source of support: Editorial and writing services, and
the meetings during which these consensus points
were formulated and discussed, were supported
by an unrestricted educational grant from Pfizer
Corporation Hong Kong Limited.
References
1. Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American
Heart Association Task Force on Practice Guidelines.
Circulation 2014;129(25 Suppl 2):S49-73. Crossref
2. Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of
cardiovascular diseases. Part I: general considerations,
the epidemiologic transition, risk factors, and impact of
urbanization. Circulation 2001;104:2746-53. Crossref
3. Cheung MY, Ong KL, Tso WK, Lam TH, Lam SL. Increasing
prevalence of hypertension in Hong Kong Cardiovascular
Risk Factor Prevalence Study: role of general and central
obesity. Proceedings of the 16th Medical Research
Conference; 2011 Jan 22; Department of Medicine, The
University of Hong Kong, Hong Kong. Hong Kong Med J
2011;17(Suppl 1):16S.
4. Roth GA, Huffman MD, Moran AE, et al. Global and
regional patterns in cardiovascular mortality from 1990 to
2013. Circulation 2015;132:1667-78. Crossref
5. Cheung MY, Chow CC, Chu DW, et al. The Hong Kong
Cardiovascular Task Force. Towards cardiovascular
disease protection. Consensus statement on preventing
cardiovascular disease in the Hong Kong population. Med
Prog 2008;35:473-9.
6. Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to
reduce atherosclerotic cardiovascular risk in adults: a
report of the American College of Cardiology/American
Heart Association Task Force on Practice Guidelines. J Am
Coll Cardiol 2014;63(25 Pt B):2889-934. Crossref
7. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC
guidelines for the management of arterial hypertension: the
Task Force for the Management of Arterial Hypertension
of the European Society of Hypertension (ESH) and of
the European Society of Cardiology (ESC). Eur Heart J
2013;34:2159-219. Crossref
8. James PA, Oparil S, Carter BL, et al. 2014 Evidence-based
guideline for the management of high blood pressure
in adults: report from the panel members appointed to
the Eighth Joint National Committee (JNC 8). JAMA
2014;311:507-20. Crossref
9. Piepoli MF, Hoes AW, Agewall S, et al. 2016 European
guidelines on cardiovascular disease prevention in
clinical practice: The Sixth Joint Task Force of the
European Society of Cardiology and Other Societies on
Cardiovascular Disease Prevention in Clinical Practice
(constituted by representatives of 10 societies and by
invited experts) developed with the special contribution of
the European Association for Cardiovascular Prevention &
Rehabilitation (EACPR). Eur Heart J 2016;37:2315-81. Crossref
10. Collins GS, Altman DG. Predicting the 10 year risk of
cardiovascular disease in the United Kingdom: independent
and external validation of an updated version of QRISK2.
BMJ 2012;344:e4181. Crossref
11. QRISK2. Available from: https://www.qrisk.org/2016/.
Accessed 9 Jan 2017.
12. Scandinavian Simvastatin Survival Group. Randomized
trial of cholesterol lowering in 4,444 patients with coronary
heart disease: the Scandinavian Simvastatin Survival Study
(4S). Lancet 1994;344:1383-9.
13. Shepherd J, Cobbe SM, Ford I, et al. Prevention of
coronary heart disease with pravastatin in men with
hypercholesterolemia. West of Scotland Coronary
Prevention Study Group. N Engl J Med 1995;333:1301-7. Crossref
14. Intensive blood-glucose control with sulphonylureas or
insulin compared with conventional treatment and risk of
complications in patients with type 2 diabetes (UKPDS 33).
UK Prospective Diabetes Study (UKPDS) Group. Lancet
1998;352:837-53. Crossref
15. Retinopathy and nephropathy in patients with type 1
diabetes four years after a trial of intensive therapy. The
Diabetes Control and Complications Trial/Epidemiology
of Diabetes Interventions and Complications Research
Group. N Engl J Med 2000;342:381-9. Crossref
16. Antithrombotic Trialists’ Collaboration. Collaborative
meta-analysis of randomised trials of antiplatelet therapy
for prevention of death, myocardial infarction, and stroke
in high risk patients. BMJ 2002;324:71-86. Crossref
17. US Department of Health and Human Services. The
health benefits of smoking cessation. Washington DC: US
Department of Health and Human Services; 1990.
18. Taylor R, Brown A, Ebrahim S, et al. Exercise-based
rehabilitation for patients with coronary heart disease:
systematic review and meta-analysis of randomized
controlled trials. Am J Med 2004;116:682-92. Crossref
19. Prevention of cardiovascular disease. Guidelines for
assessment and management of cardiovascular risk.
Geneva, World Health Organization; 2007.
20. American Diabetes Association. Standards of medical care
in diabetes—2014. Diabetes Care 2014;37(Suppl 1):S14-80. Crossref
21. The Hong Kong reference framework for diabetes care
for adults in primary care settings. Available from: http://www.pco.gov.hk/english/resource/files/RF_DM_full.pdf.
Accessed 1 Dec 2014.
22. Rydén L, Grant PJ, Anker SD, et al. ESC guidelines on
diabetes, pre-diabetes, and cardiovascular diseases
developed in collaboration with the EASD: the Task Force
on diabetes, pre-diabetes, and cardiovascular diseases of
the European Society of Cardiology (ESC) and developed
in collaboration with the European Association for the
Study of Diabetes (EASD). Eur Heart J 2013;34:3035-87. Crossref
23. Wang C, Collet JP, Lau J. The effect of Tai Chi on health
outcomes in patients with chronic conditions: a systematic
review. Arch Intern Med 2004;164:493-501. Crossref
24. WHO Expert Consultation. Appropriate body-mass index
for Asian populations and its implications for policy and
intervention strategies. Lancet 2004;363:157-63. Crossref
25. International Diabetes Federation. The IDF consensus
worldwide definition of the metabolic syndrome. Available
from: http://www.idf.org/webdata/docs/MetSyndrome_FINAL.pdf. Accessed 10 Jul 2015.
26. West R, McNeill A, Raw M. Smoking cessation guidelines
for health professionals: an update. Health Education
Authority. Thorax 2000;55:987-99. Crossref
27. National Institute for Health and Clinical Excellence. Hypertension in adults: diagnosis and management. NICE guideline (CG127). August 2011. Available from: https://www.nice.org.uk/guidance/cg127. Accessed 10 Jul 2015.
28. National Institute for Health and Clinical Excellence. Type 2 diabetes: The management of type 2 diabetes. NICE guideline (CG87). May 2009. Accessed 10 Jul 2015.
29. National Institute for Health and Care Excellence. Chronic kidney disease in adults: assessment and management. NICE guideline (CG182). July 2014. Accessed 10 Jul 2015.
30. Shen L, Shah BR, Reyes EM, et al. Role of diuretics, β
blockers, and statins in increasing the risk of diabetes in
patients with impaired glucose tolerance: reanalysis of data
from the NAVIGATOR study. BMJ 2013;347:f6745. Crossref
31. Bangalore S, Parkar S, Grossman E, Messerli FH. A meta-analysis
of 94,492 patients with hypertension treated with
beta blockers to determine the risk of new-onset diabetes
mellitus. Am J Cardiol 2007;100:1254-62. Crossref
32. Messerli FH, Bangalore S. Half a century of
hydrochlorothiazide: facts, fads, fiction, and follies. Am J
Med 2011;124:896-9. Crossref
33. Williams B, MacDonald TM, Morant S, et al. Spironolactone
versus placebo, bisoprolol, and doxazosin to determine
the optimal treatment for drug-resistant hypertension
(PATHWAY-2): a randomised, double-blind, crossover
trial. Lancet 2015;386:2059-68. Crossref
34. National Institute for Health and Care Excellence. Cardiovascular disease: risk assessment and reduction, including lipid modification. NICE guideline (CG181). July 2014. Accessed 10 Jul 2015.
35. Baigent C, Keech A, Kearney PM, et al. Efficacy and safety
of cholesterol-lowering treatment: prospective meta-analysis
of data from 90 056 participants in 14 randomised
trials of statins. Lancet 2005;366:1267-78. Crossref
36. Tomlinson B, Hu M, Zhang Y, Liu ZM, Chan P. Response to
the letter “No evidence to support high-intensity statin in
Chinese patients with coronary heart disease”. Int J Cardiol
2016;209:192-3. Crossref
37. Liao JK. Safety and efficacy of statins in Asians. Am J
Cardiol 2007;99:410-4. Crossref
38. Everett BM, Smith RJ, Hiatt WR. Reducing LDL with
PCSK9 inhibitors—the clinical benefit of lipid drugs. N
Engl J Med 2015;373:1588-91. Crossref
39. Mayor S. NICE recommends PCSK9 inhibitors for patients
not responding to statins. BMJ 2016;353:i2609. Crossref
40. Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of
hyperglycemia in type 2 diabetes, 2015: a patient-centered
approach: update to a position statement of the American
Diabetes Association and the European Association for the
Study of Diabetes. Diabetes Care 2015;38:140-9. Crossref
41. Ma J, Sehgal NL, Ayanian JZ, Stafford RS. National trends
in statin use by coronary heart disease risk category. PLoS
Med 2005;2:e123. Crossref
42. Pearson TA. The prevention of cardiovascular disease:
have we really made progress? Health Aff (Millwood)
2007;26:49-60. Crossref
43. Yusuf S, Islam S, Chow CK, et al. Use of secondary prevention
drugs for cardiovascular disease in the community in high-income,
middle-income, and low-income countries (the
PURE Study): a prospective epidemiological survey. Lancet
2011;378:1231-43. Crossref