Hong Kong Med J 2017 Apr;23(2):150–7 | Epub 24 Feb 2017
DOI: 10.12809/hkmj164993
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Mothers’ attitude to the use of a combined
oral contraceptive pill by their daughters for
menstrual disorders or contraception
KW Yiu, MRCOG, FHKAM (Obstetrics and Gynaecology);
Symphorosa SC Chan, FRCOG, FHKAM (Obstetrics and Gynaecology);
Tony KH Chung, FRANZCOG, FRCOG
Department of Obstetrics and Gynaecology, The Chinese University of
Hong Kong, Prince of Wales Hospital, Shatin, Hong Kong
Corresponding author: Dr Symphorosa SC Chan (symphorosa@cuhk.edu.hk)
Abstract
Introduction: Mothers’ attitude may affect use of
combined oral contraceptive pills by their daughters.
We explored Chinese mothers’ knowledge of
and attitudes towards the use of combined oral
contraceptive pills by their daughters for menstrual
disorders or contraception, and evaluate the factors
affecting their attitude.
Methods: This survey was conducted from October
2012 to March 2013, and recruited Chinese women
who attended a gynaecology clinic or accompanied
their daughter to a gynaecology clinic, and who
had one or more daughters aged 10 to 18 years.
They completed a 41-item questionnaire to assess
their knowledge of and attitude towards use of the
combined oral contraceptive pills by their daughters.
The demographic data of the mothers and their
personal experience in using the pills were also
collected.
Results: A total of 300 women with a mean age
of 45.2 (standard deviation, 5.0) years completed
the questionnaire. Only 58.3% of women reported
that they had knowledge about the combined oral
contraceptive pills; among them, a majority (63.3%)
reported that their source of knowledge came from
medical professionals. Of a total possible score of
22, their mean knowledge score for risk, side-effects,
benefits, and contra-indications to use of combined
oral contraceptive pills was only 5.0 (standard
deviation, 4.7). If the medical recommendation
to use an oral contraceptive was to manage their
daughter’s dysmenorrhoea, menorrhagia, acne,
or contraception needs, 32.0%, 39.3%, 21.0% and
29.7%, respectively would accept this advice.
Women who were an ever-user of combined oral
contraceptive pills or who were more knowledgeable
about combined oral contraceptives had a higher
acceptance rate.
Conclusions: Chinese women had a low acceptance
level of using combined oral contraceptive pills as a
legitimate treatment for their daughters. This was
associated with lack of knowledge or a high degree
of uncertainty about their risks and benefits. It is
important that health caregivers provide up-to-date
information about combined oral contraceptive pills
to women and their daughters.
New knowledge added by this study
- Chinese women had a low acceptance level of combined oral contraceptive (COC) pills as a legitimate treatment for their daughters. This was associated with lack of knowledge or a high degree of uncertainty about the risks and benefits of COC use.
- Health caregivers should provide up-to-date information to potential COC users.
Introduction
The combined oral contraceptive (COC) pill is an
effective contraception. It has a very low-risk profile
documented over several decades and its protective
effect on endometrial and ovarian carcinoma has
been well established.1 It is also an effective treatment
for menstrual problems and polycystic ovarian
syndrome,2 3 which are common in adolescents.4 5 6 7
The prevalences of menorrhagia, dysmenorrhoea,
and menstrual symptoms in adolescent girls have
been reported to be 17.9%, 68.7%, and 37.7%,
respectively.4 The prevalence of polycystic ovarian
syndrome in adolescent girls has been reported to
be 16% in those who attended a local paediatric and
adolescent gynaecology clinic.5 Nonetheless, the
use of COC pills in Chinese women has remained
low; only 1% of women of reproductive age (20-49
years) in China used the pills in 2010.8 There are
some obstacles to access although family planning is
a relatively well-funded area of health care in China
and has been implemented for decades. In Hong
Kong, the situation is slightly less unusual. From an
online survey conducted in Hong Kong, 12.6% of
women had used an oral contraceptive in the year
prior to the survey, but many of them had stopped
using it.9 According to the annual report of the
Family Planning Association of Hong Kong in 2014-2015, 22% of the 48 363 clients who practised birth
control, including women who were both married
and unmarried, used an oral contraceptive.10 Only
6% of teenage girls who attended the youth health
care centres used COC pills for contraception.11
Although sex education has been integrated
into the primary and secondary educational
curriculum for many years, efforts to provide
quality sex education have been limited.12 According
to a survey conducted by the Hong Kong SAR
Government, sex education at the junior secondary
school level is limited to an average of 3 to 4 school
hours only.13 Sometimes concepts emphasised
included protection of self and avoidance of sex,
especially prior to marriage.14 The median age of
marriage in Hong Kong is now close to 30 years. It is
notable that Hong Kong has a high rate of therapeutic
abortion that is underestimated by official statistics
because an indeterminate proportion is performed
in mainland China due to cost considerations. In
women attending for their antenatal visit, a high
proportion of 36.5% reported a previous therapeutic
abortion (unpublished data from our institute). This
suggests that women of reproductive age may not
have been educated about contraception. There is
little published information on the use of COC pills
for the management of menstrual problems in Hong
Kong but it is likely to be low. Misconceptions and
myths about COC pills are likely to be the main
obstacles to use. Although extensive high-quality
information about use of COC is currently available
from various sources, many women remain unaware
of the non-contraceptive benefits of COC. They
also have little awareness of the risks of COC.15 For
female adolescents, their decision about whether to
use COC is likely to be influenced by their parents,
especially their mothers, who may be giving advice
to their daughters based on little or erroneous
knowledge. This may lead mothers to make decisions
that are not in their daughter’s best interests.
Focused education about COC may lead to
a more balanced view, both in adolescents and
their mothers. In a study of Korean and Japanese
university students, significant correlation between
knowledge of and positive attitude towards COC
pills was reported.16 Mothers in Asia are also often
involved in their teenage daughters’ decision to
begin sexual relationships, the use of contraceptives, and
even vaccination.17 18 Since the mothers’ attitude may affect use of COC by their daughters, we explored
Chinese mothers’ knowledge of and attitudes
towards such use. Mothers’ knowledge about the
COC pills and factors affecting their attitude were
also evaluated.
Methods
The study was conducted from October 2012 to
March 2013 in the gynaecology clinic of a tertiary
teaching hospital in Hong Kong. Women who
attended the clinic or accompanied a daughter
to the clinic, and who had one or more daughters
aged 10 to 18 years were recruited. Women who
did not speak or read Chinese were excluded. The
participants completed a 41-item questionnaire
to assess their knowledge of and attitude towards
use of COC pills by their daughters. Firstly, they
were asked to self-assess their own knowledge of
the COC pill. The knowledge domain consisted
of 19 items testing their knowledge of the non-contraceptive
health benefits and side-effects of
COC pills, and three items on contra-indications to
use of COC pills. For each item, participants were
asked to respond “yes”, “no”, or “don’t know”. They
were then asked about their attitudes to the use of
COC pills by their daughters aged 10 to 18 years for the
management of dysmenorrhoea, menorrhagia, acne,
or as a contraceptive. They were asked to respond
from “strongly agree”, “agree”, “disagree”, to “strongly
disagree”. Reasons for agreeing or disagreeing with
the use of COC pills and the appropriate age or
life-events for using COC pills by their daughters
were also asked. Finally, demographic data and
their personal experience in using COC pills were
collected. Knowledge score and uncertainty score
were calculated for the participants based on their
response15 16—knowledge score was defined as the score of correct answers with 1 score given for
each correct answer (ie range from 0-22); a “don’t
know” reply would create the uncertainty score. The
participants provided written informed consent,
and approval was obtained from the local ethics
committee (CRE-2012.186).
Statistical analyses
Descriptive statistics were used to summarise
participants’ demographic information. Association
between participant characteristics and overall
attitude was explored using Chi squared and
independent-samples t test. A P value of <0.05 was
considered statistically significant. All statistical
analyses were conducted using the SPSS (Windows
version 18.0; SPSS Inc, Chicago [IL], United States). Assuming
that 50% of the women accepted the use of COC pills
by their daughters with an accepted error of 0.05%,
278 women were required. An additional 10% was
recruited to prepare for an incomplete questionnaire.
Results
Apart from 150 women who were excluded because
they did not have a daughter aged 10 to 18 years, a
total of 317 women were invited to participate; 302
agreed and 300 (94.6%) completed the questionnaire.
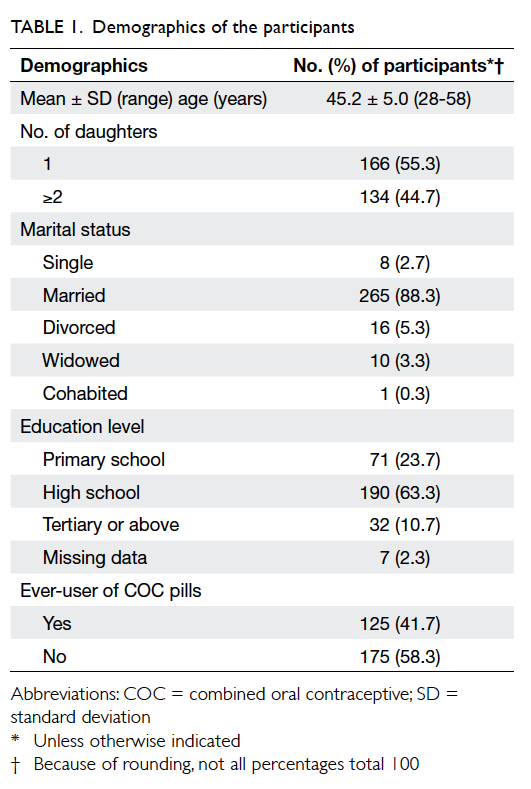
Demographic characteristics of the participants are
shown in Table 1. Their mean age was 45.2 years (range, 28-58 years). The median number of daughters
was one and most participants (88.3%) were married.
Most (>70%) had high school education. In all, 125
(41.7%) were ever-users of COC pills, including both
current and ex-users. Overall, 175 (58.3%) reported
that they had knowledge about the COC pills, while
125 (41.7%) reported no knowledge.
The rates of giving correct answers about the
COC pill and the comparison between ever- and
never-users of COC pills are shown in Table 2. Of
a total possible score of 22, the mean (± standard
deviation) knowledge score of all the participants was
5.0 ± 4.7. Of all the participants, only approximately
20% of the mothers correctly answered that COC
pills would not cause carcinoma of ovary and
corpus; 26.0%, 29.7%, and 30.3% respectively
correctly answered that COC pills did not have
proven teratogenicity, cause pelvic inflammatory
disease and infertility; 10.3% knew that COC pills
would not cause weight gain and 25.7% answered
that COC pills would not lead to a depressive mood.
In all, 43.3%, 33.0%, and 25.3% knew that COC pills
had the benefits of regulating the menstrual cycle,
decreasing menstrual flow, and helping to relieve
dysmenorrhoea, respectively. Moreover only 20%
knew that the COC pills are not contra-indicated
in people with a family history of breast cancer
but is contra-indicated in thromboembolism. The
knowledge score of the 175 women who responded
to have knowledge of the COC pills was significantly
higher than those who reported lack of knowledge
(8.0 ± 4.4 vs 3.0 ± 3.7; P<0.001). Among those who
declared they had knowledge about the use of COC
pills, their sources of knowledge were from medical
professional (63.3%), media (30.3%), friends (24.6%),
family members (6.9%), school (2.9%), and others
(1%).
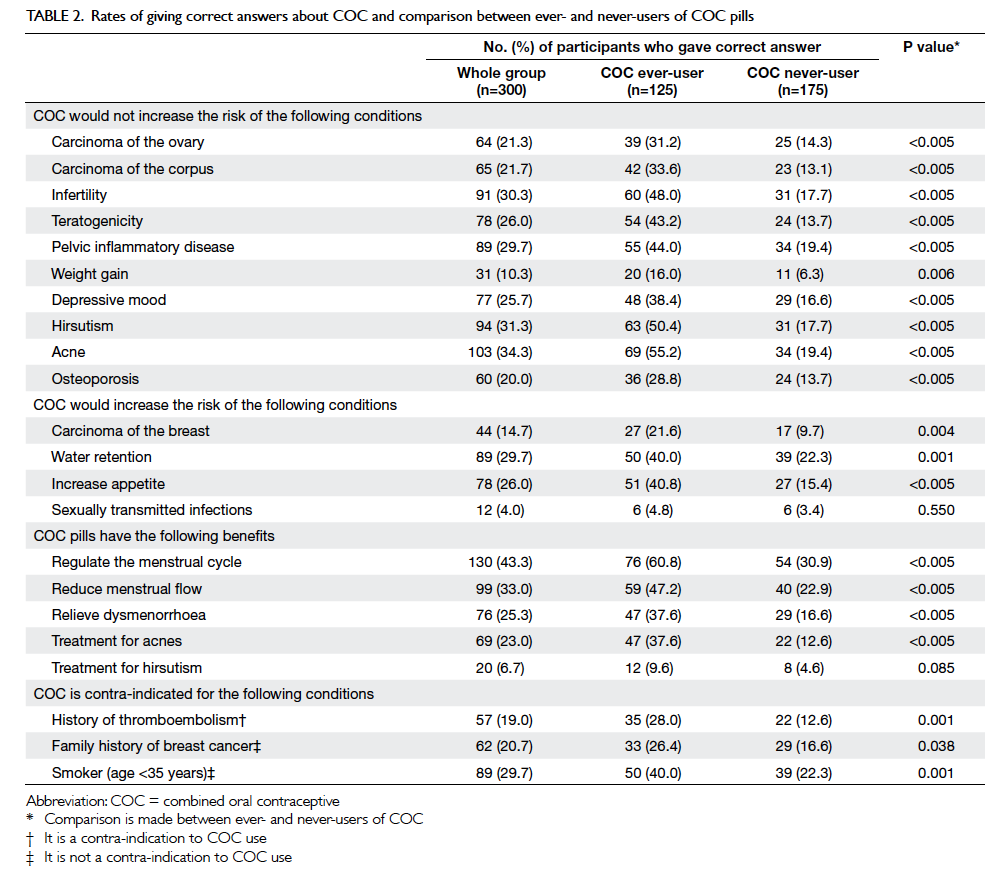
Table 2. Rates of giving correct answers about COC and comparison between ever- and never-users of COC pills
The rate of responding “uncertain” to the health
benefit, side-effects, or contra-indications of COC
use ranged from 43.7% to 71.0% for each item. The
mean uncertainty score among all participants was
13.0 ± 7.6. The uncertainty score was significantly
higher in participants who reported to have lack of
knowledge when compared with those reported to
have knowledge about COC pills (15.6 ± 7.1 vs 9.1 ±
6.7; P<0.001).
Among the ever-users, 43 (34%), five (4%), and
96 (77%) women reported that COC pills had been
used to manage their own menstrual problems, acne
problems, and as contraception, respectively. Table 3 lists the participants’ acceptance rate of COC use by their daughters in different gynaecological
conditions and the comparison between ever- and
never-users of COC pills. More ever-users than
never-users accepted the use of COC for their
daughter’s gynaecological indications. Participants
who accepted their daughter’s use of COC also had a
higher knowledge score and lower uncertainty score
(Table 4). Table 5 shows the participants’ reasons for accepting use of COC pills by their daughters.
Recommendation by medical professionals was the
major reason, followed by the knowledge that COC
pills provided effective contraception.
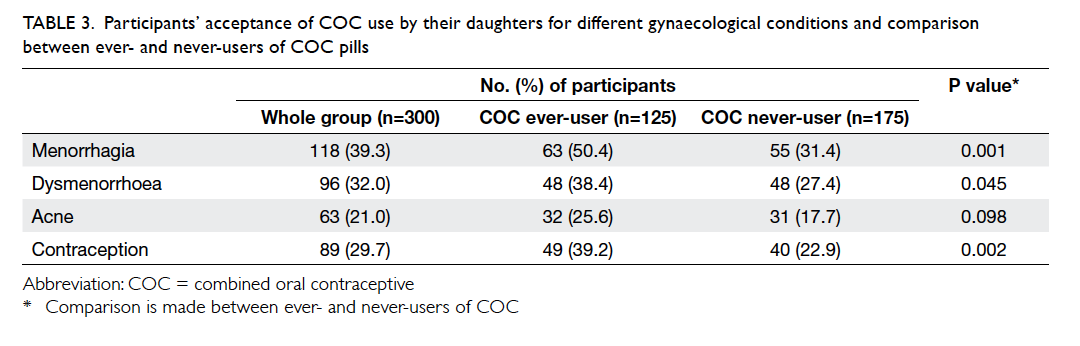
Table 3. Participants’ acceptance of COC use by their daughters for different gynaecological conditions and comparison between ever- and never-users of COC pills
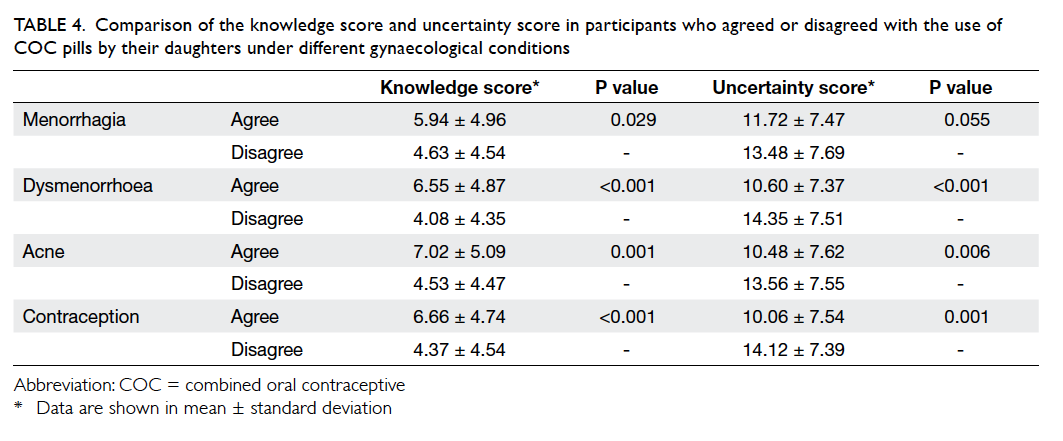
Table 4. Comparison of the knowledge score and uncertainty score in participants who agreed or disagreed with the use of COC pills by their daughters under different gynaecological conditions
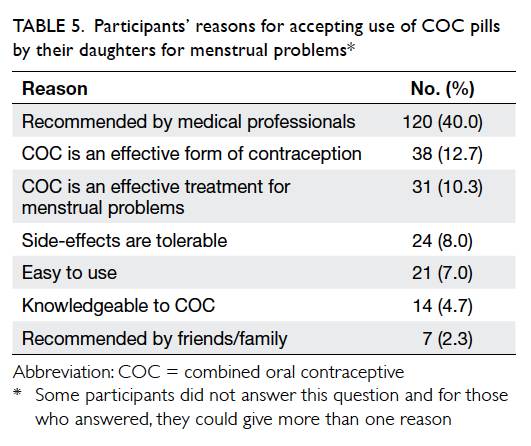
Table 5. Participants’ reasons for accepting use of COC pills by their daughters for menstrual problems
Age, education level, and whether they had
previous experience of side-effects of COC pills were
not associated with participants’ acceptance of COC
use by their daughters. Among the 125 ever-users of
COC pills, 65 (52.0%) reported they had experienced
side-effects, including weight gain (n=45), fluid
retention (n=25), headache (n=12), increase in
appetite (n=8), mode disturbance (n=8), and acne
(n=4). Table 6 lists the reasons for disagreement with the use of COC pills by their daughters for menstrual
problems. Finally, only 71 (23.6%) participants
thought that the use of COC pills was appropriate in
girls aged 12 to 18 years.
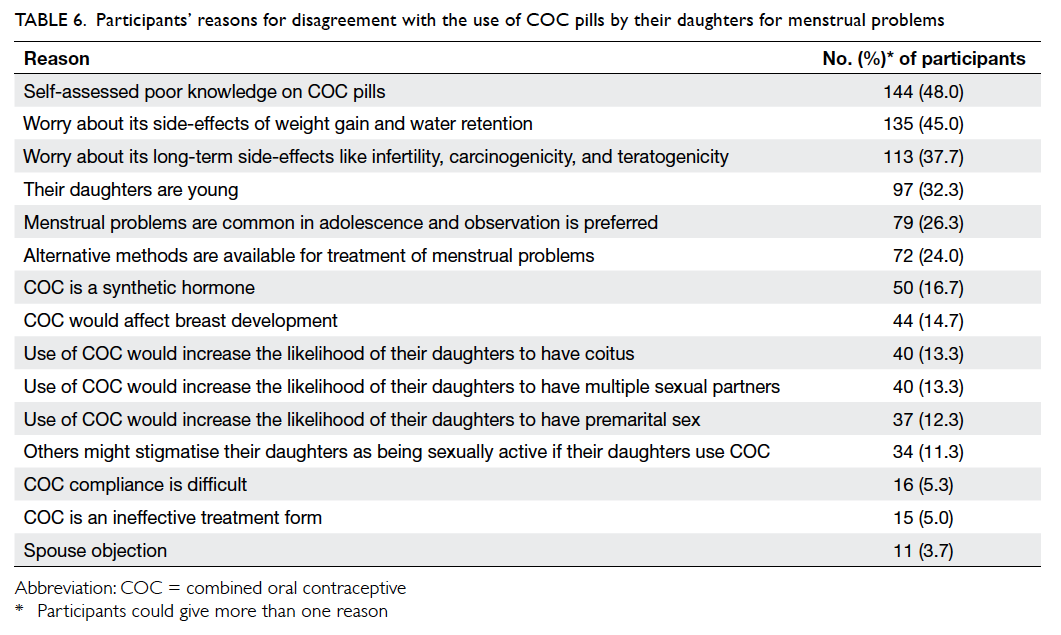
Table 6. Participants’ reasons for disagreement with the use of COC pills by their daughters for menstrual problems
Discussion
Our study highlights a notable lack of knowledge
about the use of COC pills in many Hong Kong
Chinese mothers. Many were uncertain or had
erroneous beliefs about the use of COC pills. They
believed that such usage would lead to cancers,
fetal deformity, and cause infertility and pelvic
inflammatory disease. These misconceptions and
uncertainties may further reinforce their non-acceptance
of the COC pills as an appropriate
medication for their daughters. This inevitably often
leads to suboptimal treatment for their daughters.
Fear of increased risk of cancer is an important
reason for low acceptance of COC pills and only
22% of our participants thought it did not increase
the risk for carcinoma of ovary or uterus. More
than 60% of the participants were uncertain about
the risk of cancer with the use of COC pills (results
not shown). Research has shown that contraceptives
have a significantly protective effect on carcinoma
of ovary and corpus uteri.19 20 In fact, a collaborative re-analysis of individual data from 53 297 women with
breast cancer and 100 239 women without breast
cancer from 54 epidemiological studies revealed
that while women were taking COC pills and in the
10 years after stopping, there was a small increase
in the relative risk of breast cancer.21 There was,
however, no significant excess risk of having breast
cancer diagnosed ≥10 years after stopping
use of COC pills. The breast cancer incidence rises
steeply with age. The estimated excess number of
cancers diagnosed in the period between starting
use and 10 years after stopping increases with age
at last use. The estimated excess number of breast
cancers diagnosed up to 10 years after stopping
use from the age of 16 to 19 years among 10 000
women has been reported to be 0.5 (95% confidence
interval, 0.3-0.7) only.21 The Nurses’ Health Study
with 121 701 participants followed up for 36 years
revealed that longer duration of COC use was
strongly associated with premature mortality due
to breast cancer.22 Another highlight was that only
20.7% of our participants knew that a family history
of breast cancer was not a contra-indication to use of
COC pills.
Another common misconception is that the
use of COC pills can lead to future subfertility.
The COC pill preserves fertility by diminishing the
risk of ectopic pregnancy.23 According to a review,
1-year pregnancy rates after discontinuation of COC
ranged from 79% to 96%, similar to those reported
following discontinuation of barrier methods or no
contraception.24 Moreover, the progestogen effect of
COC pills results in production of thick, tenacious
cervical mucus that resists penetration by bacteria
and spermatozoa and reduces the risk of upper
genital tract infection. Use of COC pills was also
quoted to be protective against symptomatic pelvic
inflammatory disease, with a 50% reduction in rate
of hospitalisation for the disease, with itself being a
risk factor for subfertility.25 The COC pill does not
protect against sexually transmitted infections. On
the other hand, there is no evidence to support the
notion that the use of COC pills is associated with
high-risk sexual behaviour in adolescents, which is a
very common fear among Hong Kong mothers.
Primary dysmenorrhoea is prevalent during
adolescence. Approximately 6.4% of adolescents or
29% of those reporting severe dysmenorrhoea seek
help from a physician.4 A review and meta-analysis
of five trials of the use of COC pills concluded that
it was more effective than placebo in managing
dysmenorrhoea.2 One of the most common problems
reported by adolescents is irregular and/or profuse
menstruation. The COC pill is also effective in
treating and preventing heavy menstrual bleeding. In
our study, only 25% to 43% of the participants knew
that it is an appropriate treatment for menstrual
problems and 50% were uncertain.
The fear of side-effects often leads to reluctance
to using new treatments.18 In many cases, such fears
are often unfounded. In our study, participants
believed that weight gain and depressive mood were
side-effects of COC pills, although pooled analysis
of a placebo-controlled trial showed no difference
in weight gain.26 Furthermore, depressive symptoms
are common in adolescence.27 In a randomised
controlled study, there was no difference in mood
changes throughout the menstrual cycle between
COC users and non-users.28 In a prospective study
of 43 adolescents, subjects anticipated more side-effects
than they actually experienced after 6 months
of taking COC pills.29
It is important to provide correct information
to women and their teenage daughters if they are
contemplating the use of COC pills. In our study,
40% of participants indicated that recommendation
from a medical professional was a critical factor in
their acceptance of the use of COC pills by their
daughters.
Only 19% of participants were aware that
thromboembolism is a contra-indication to COC
use. Venous thromboembolism in Asians has been
reported to be low.30 A recent case-control study
confirmed that current exposure to any COC poses
a 3-times higher risk of venous thromboembolism
compared with no exposure in the previous year.31
The risk is higher with COC pills containing
desogestrel (odds ratio, 4.3), gestodene (3.6),
drospirenone (4.1), and cyproterone (4.3) than the
second-generation COC pills with levonorgestrel
(2.4) and norgestimate (2.5).31 The risk of venous
thromboembolism is also increased for COC users
with a family history of venous thromboembolism.32
Clinicians should assess the woman’s personal and
family history of thromboembolism, and provide
information about the warning symptoms of
venous thromboembolism before prescribing a
new generation pill. As recommended by the World
Health Organization, the COC pill is not contra-indicated
in smokers <35 years old33;
approximately 30% of our participants answered this
correctly.
This study has several limitations. First,
there may be selection bias as subjects were
women who presented to the gynaecology clinic or
accompanied their daughter to a gynaecology clinic
for a gynaecological problem. The results may not be
generalised to the whole population of Hong Kong.
Second, the questionnaire was not validated and the
questions did not include all aspects of the use of
COC pills. Third, we relied on women’s self-reported
use of COC pills and could not verify the information.
Despite these, the questionnaire included the most
widely studied aspects of non-contraceptive benefits
and risks of the COC pill and knowledge score
or uncertainty score have been used in previous
literature.15 16 Although this study was conducted in only one centre and in Chinese women only, it helps
clinicians to understand the low levels of acceptance
of and compliance with prescribed COC pills.
The degree of misconception among Hong
Kong mothers about COC use is of concern. Hong
Kong has a well-developed education system with
many highly regarded universities. The reported
limited sex education in schools may be responsible
for this knowledge gap of Hong Kong mothers.13 This
may in turn have an impact on the advice they give
their daughters, who are usually compliant with their
mother’s wishes. Specific training in communication
and counselling skills should be provided to health
care professionals when promoting sexual health to
women and adolescents.34
Conclusions
Our study found that the Hong Kong Chinese women
who attended a gynaecology clinic of a tertiary centre
had a low acceptance rate of the use of COC pills by
their daughters. This low acceptance was associated
with a lack of knowledge and misconception of the
risks and benefits of the COC pills. Such ignorance
will exert an adverse influence on the choice of
treatment for many gynaecological problems in
teenage daughters.
Declaration
All authors have disclosed no conflicts of interest.
References
1. Vessey M, Painter R. Oral contraceptive use and cancer.
Findings in a large cohort study, 1968-2004. Br J Cancer
2006;95:385-9. Crossref
2. Proctor ML, Roberts H, Farquhar CM. Combined
oral contraceptive pill (OCP) as treatment for
primary dysmenorrhoea. Cochrane Database Syst Rev
2001;(4):CD002120.
3. Nader S, Diamanti-Kandarakis E. Polycystic ovary
syndrome, oral contraceptives and metabolic issues: new
perspectives and a unifying hypothesis. Hum Reprod
2007;22:317-22. Crossref
4. Chan SS, Yiu KW, Yuen PM, Sahota DS, Chung TK.
Menstrual problems and health-seeking behaviour in
Hong Kong Chinese girls. Hong Kong Med J 2009;15:18-23.
5. Chung PW, Chan SS, Yiu KW, Lao TT, Chung TK.
Menstrual disorders in a Paediatric and Adolescent
Gynaecology Clinic: patient presentations and longitudinal
outcomes. Hong Kong Med J 2011;17:391-7.
6. Esmaelizadeh S, Delavar MA, Amiri M, Khafri S, Pasha
NG. Polycystic ovary syndrome in Iranian adolescents. Int
J Adolesc Med Health 2014;26:559-65. Crossref
7. Christensen SB, Black MH, Smith N, et al. Prevalence of
polycystic ovary syndrome in adolescents. Fertil Steril
2013;100:470-7. Crossref
8. Wang C. Trends in contraceptive use and determinants of
choice in China: 1980-2010. Contraception 2012;85:570-9. Crossref
9. Lo SS, Fan SY. Acceptability of the combined oral
contraceptive pill among Hong Kong women. Hong Kong
Med J 2016;22:231-6.
10. The Family Planning Association of Hong Kong. 2014-2015 Annual report. Available from: http://www.famplan.org.hk/fpahk/en/template1.asp?style=template1.asp&content=about/annualreport.asp. Accessed 28 Apr 2016.
11. The Family Planning Association of Hong Kong. Youth
sexuality in Hong Kong secondary school survey. Available
from: http://www.famplan.org.hk/fpahk/en/template1.asp?content=info/research.asp. Accessed 28 Apr 2016.
12. Che FS. A study of the implementation of sex education in
Hong Kong secondary schools. Sex Educ 2005;5:281-94. Crossref
13. Survey of life skills-based education on HIV/AIDS at
junior level of secondary schools in Hong Kong. Red
Ribbon Centre, Department of Health, Hong Kong SAR
Government; 2014.
14. Wong WC, Lee A, Tsang KK, Lynn H. The impact of AIDS/sex education by schools or family doctors on Hong Kong Chinese adolescents. Psychol Health Med 2006;11:108-16. Crossref
15. Voqt C, Schaefer M. Disparities in knowledge and interest
about benefits and risks of combined oral contraceptives.
Eur J Contracept Reprod Health Care 2011;16:183-93. Crossref
16. Lim HJ, Lee MS, Cho YH, Kazumi U. A comparative study
of knowledge about and attitudes toward the combined
oral contraceptives among Korean and Japanese university
students. Pharmacoepidemiol Drug Saf 2004;13:741-7. Crossref
17. Bachar R, Yogev Y, Fisher M, Geva A, Blumberg G, Kaplan
B. Attitudes of mothers toward their daughters’ use of
contraceptives in Israel. Contraception 2002;66:117-20. Crossref
18. Chan SS, Cheung TH, Lo WK, Chung TK. Women’s
attitudes on human papillomavirus vaccination to their
daughters. J Adolesc Health 2007;41:204-7. Crossref
19. Cibula D, Gompel A, Mueck AO, et al. Hormonal
contraception and risk of cancer. Hum Reprod Update
2010;16:631-50. Crossref
20. Bitzer J. Oral contraceptives in adolescent women. Best
Pract Res Clin Endocrinol Metab 2013;27:77-89. Crossref
21. Collaborative Group on Hormonal Factors in Breast Cancer.
Breast cancer and hormonal contraceptives: collaborative
reanalysis of individual data on 53 297 women with breast
cancer and 100 239 women without breast cancer from 54
epidemiological studies. Lancet 1996;347:1713-27. Crossref
22. Charlton BM, Rich-Edwards JW, Colditz GA, et al. Oral
contraceptive use and mortality after 36 years of follow-up
in the Nurses’ Health Study: prospective cohort study. BMJ
2014;349:g6356. Crossref
23. Burkman R, Schlesselman JJ, Zieman M. Safety concerns
and health benefits associated with oral contraception. Am
J Obstet Gynecol 2004;190 (4 Suppl):S5-22. Crossref
24. Mansour D, Gemzell-Dianielsson K, Inki P, Jensen
JT. Fertility after discontinuation of contraception: a
comprehensive review of the literature. Contraception
2011;84:465-77. Crossref
25. Guillebaud J, MacGregor A. Contraception: your questions
answered. 6th ed. London: Churchill Livingstone; 2013.
26. Gallo MF, Lopez LM, Grimes DA, Carayon F, Schulz KF,
Helmerhorst FM. Combination contraceptives: effects on
weight. Cochrane Database Syst Rev 2014;(1):CD003987. Crossref
27. Saluja G, Iachan R, Scheidt PC, Overpeck MD, Sun W,
Giedd JN. Prevalence of and risk factors for depressive
symptoms among young adolescents. Arch Pediatr Adolesc
Med 2004;158:760-5. Crossref
28. Walker A, Bancroft J. Relationship between premenstrual
symptoms and oral contraceptive use: a controlled study.
Psychosom Med 1990;52:86-96. Crossref
29. Rosenthal SL, Cotton S, Ready JN, Potter LS, Succop
PA. Adolescents’ attitudes and experiences regarding
levonorgestrel 100 mcg/ethinyl estradiol 20 mcg. J Pediatr
Adolesc Gynecol 2002;15:301-5. Crossref
30. Lee WS, Kim KI, Lee HJ, Kyung HS, Seo SS. The incidence
of pulmonary embolism and deep vein thrombosis after
knee arthroplasty in Asians remains low: a meta-analysis.
Clin Orthop Relat Res 2013;471:1523-32. Crossref
31. Vinogradova Y, Coupland C, Hippisley-Cox J. Use
of combined oral contraceptives and risk of venous
thromboembolism: nested case-control studies using the
QResearch and CPRD databases. BMJ 2015;350:h2135. Crossref
32. Zöller B, Ohlsson H, Sundquist J, Sundquist K. Family
history of venous thromboembolism is a risk factor for
venous thromboembolism in combined oral contraceptive
users: a nationwide case-control study. Thromb J
2015;13:34. Crossref
33. Medical eligibility criteria for contraceptive use. 5th ed.
Geneva: World Health Organization; 2015.
34. Yip BH, Sheng XT, Chan VW, Wong LH, Lee SW, Abraham
AA. ‘Let’s talk about sex’—a knowledge, attitudes and
practice study among paediatric nurses about teen sexual
health in Hong Kong. J Clin Nurs 2015;24:2591-600. Crossref