Hong Kong Med J 2017 Feb;23(1):63–6 | Epub 14 Dec 2016
DOI: 10.12809/hkmj164823
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Operative outcome of Hong Kong centenarians with hip fracture
MY Cheung, MB, ChB;
Angela WH Ho, FHKCOS, FHKAM (Orthopaedic Surgery);
SH Wong, FHKCOS, FHKAM (Orthopaedic Surgery)
Department of Orthopaedics and Traumatology, Caritas Medical Centre,
Shamshuipo, Hong Kong
Corresponding author: Dr MY Cheung (jessicacheungmy@gmail.com)
An earlier version of this paper was presented as Free Paper Oral
Presentation at the 34th Annual Congress of the Hong Kong Orthopaedic
Association held in Hong Kong on 16 November 2014.
Abstract
Introduction: International clinical guidelines
recommend early surgical treatment for geriatric
patients with hip fracture. There are, however,
few data concerning the operative outcome of
centenarians. This study aimed to report the
epidemiology of hip fracture and postoperative
mortality rate, and to discuss whether operation is
justified in centenarians in Hong Kong.
Methods: This observational study was carried out
in all public hospitals of Hong Kong. All patients
aged 100 years or above who underwent hip fracture
surgery in any public hospital between 1 January
2010 and 31 December 2013 were included. Their
postoperative mean and median survival time was
recorded.
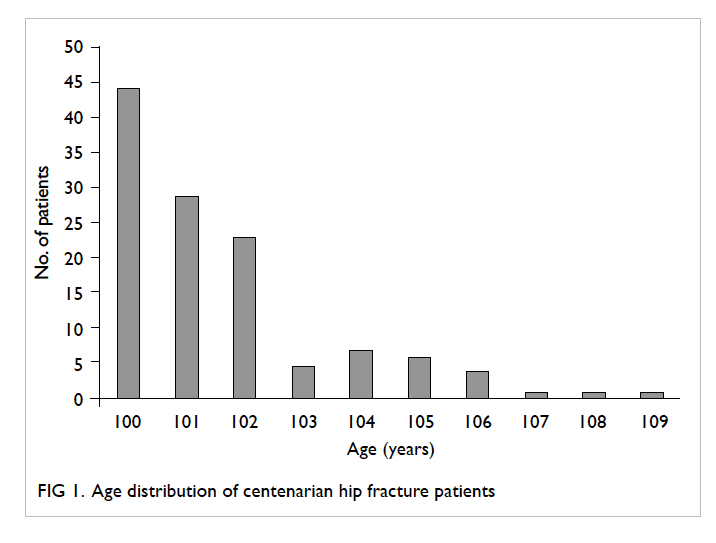
Results: Of 114 centenarians, 96 (84%) were female.
The age of patients ranged from 100 to 109 years,
with the largest number (44%) aged 100 years.
The follow-up interval ranged from 5 to 1619 days
(median, 412 days; interquartile range, 683 days).
The 1-month, 6-month, and 1-year mortalities were
8%, 25%, and 37%, respectively. By Kaplan-Meier
analysis, the postoperative mean survival was 2
years 2 months (95% confidence interval, 680-936
days) and the median survival time was 2 years
(interquartile range, 1234 days).
Conclusion: The 1-year mortality among Hong
Kong centenarians with hip fracture was 37%, which
is lower than the 41.1% in the general centenarian
population in Japan. The median survival time after
hip fracture surgery was 2 years, suggesting that
surgery even at an extreme age is worthwhile to
maintain quality of life. Extreme age should not be a
barrier to operative treatment.
New knowledge added by this study
- The postoperative 1-year mortality among Hong Kong centenarians with hip fracture was comparable to that of the general centenarian population in Japan.
- The median postoperative survival time of the centenarians in this study was 2 years.
- Operative treatment should be offered to centenarians with hip fracture to maintain their quality of life. Extreme age should not be a barrier to hip fracture surgery.
Introduction
Fragility fracture is one of the common chronic
diseases in geriatrics. The prevalence of femoral
neck osteoporosis based on a hip T-score of < –2.5 was 47.8% in males and 59.1% in females in our
previous study of 239 hip fractures.1 The incidence
of hip fracture increases with age, and the incidence
is high in the elderly (1639 per 100 000 in men and
3012 per 100 000 in women for the age-group of
≥85 years).2 3 A 2015 study of geriatric hip fracture showed that there was a steady increase in the
incidence of geriatric hip fracture in Hong Kong.4
The overall 30-day and 1-year mortalities were 3.01%
and 18.56%, respectively. Advancing age and male
sex were associated with an increased mortality and
a higher excess mortality rate following surgery.4
With the advances in medical technology, the
population of centenarians is increasing both locally
and internationally. In Hong Kong, the number of
centenarians has increased 6.5-fold over the last
30 years, from 289 in 1981 to 1890 in 2011 (about
3/10 000).5 Hong Kong women have overtaken
Japanese women for longevity, with an average life
expectancy reaching 87.32 years in 2015 compared
with 87.02 years in Japan, according to statistics from
Japan’s Ministry of Health, Labour and Welfare.6
Advanced medical service and easy access to
emergency services may contribute to this longevity.
International clinical guidelines recommend early
surgical treatment for geriatric patients with hip
fracture once their medical condition has been
optimised with the help of a geriatrician.7 There
are, however, few data concerning the operative
outcome of this group of oldest elderly. Although
centenarians represent only a small subset of the
elderly population, their number is expected to
further increase.5 Therefore it is important for us to
understand the surgical outcome for this particular
group of patients to enable provision of the best care
and effective use of limited health care resources. The
aims of our study were to report the epidemiology of
hip fracture and postoperative mortality rate, and to
discuss whether surgery is justified in this group of
patients.
Methods
This was an observational study of all patients aged
100 years or above who underwent hip fracture
surgery in any public hospital in Hong Kong between
1 January 2010 and 31 December 2013. This study was done in accordance with the principles outlined in the Declaration of Helsinki. Data were retrieved from the Hospital Authority clinical
database that included 99% of geriatric patients
with hip fracture in Hong Kong.8 9 Patients with hip fracture aged 100 years or above were extracted from
the Clinical Data Analysis and Reporting System using
International Classification of Diseases code 820
under subdivision Operation Theatre Management
System–linked diagnosis. Complications of initial hip
surgery or periprosthetic fractures were excluded.
Demographics, type of operation, and dates of
admission, discharge, and death were retrieved.
Mortality of the general population was retrieved
using census data and the death registry of Hong
Kong Special Administrative Region.
Data are shown as mean and 95% confidence
interval, or median and interquartile range.
Mortality and survival were calculated using Kaplan-Meier survival analysis. Analyses were performed
using the Statistical Package for the Social Sciences
(Windows version 16.0; SPSS Inc, Chicago [IL], US).
Comparative tests between different groups were
performed using Chi squared test. A P value of <0.05
was considered statistically significant.
Results
During the 4-year study period, 114 centenarians
underwent surgery in Hong Kong for primary hip
fracture, of whom 96 (84%) were female. The age
of patients ranged from 100 to 109 years, with the
largest number (44%) aged 100 years (Fig 1). The largest number of patients were admitted to hospitals
in Kowloon West Cluster, and this accounted for
25%. Most were residents in the Eastern district
(12%) and Sham Shui Po (11%) before admission.
Overall, 62 (54%) patients were admitted from elderly
care homes. Hip fracture surgery was performed as
an emergency in 76 (67%) patients. Closed reduction
and internal fixation of the femur was performed
in 80 (70%) patients, partial hip replacement in 28
(25%), and other hip surgery in six (5%). Postoperative
admission to an intensive care unit (ICU) or high
dependency unit (HDU) was necessary in two
patients. The mean length of stay in an acute ward
was 13.3 days, with a median of 10.5 days.
Postoperative follow-up ranged from 5 to 1619
days (median, 412 days; interquartile range, 683
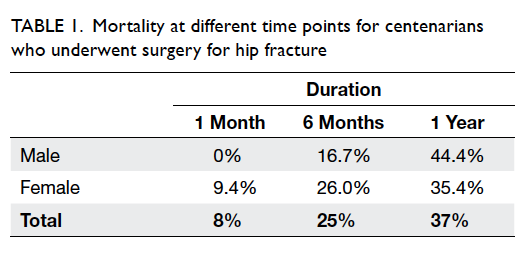
days). The 1-month, 6-month, and 1-year mortality
rates were 8%, 25%, and 37%, respectively (Table 1).
By Kaplan-Meier analysis, the postoperative mean
survival was 2 years 2 months (95% confidence
interval, 680-936 days) and the median survival time
was 2 years (interquartile range, 1234 days) [Fig 2].
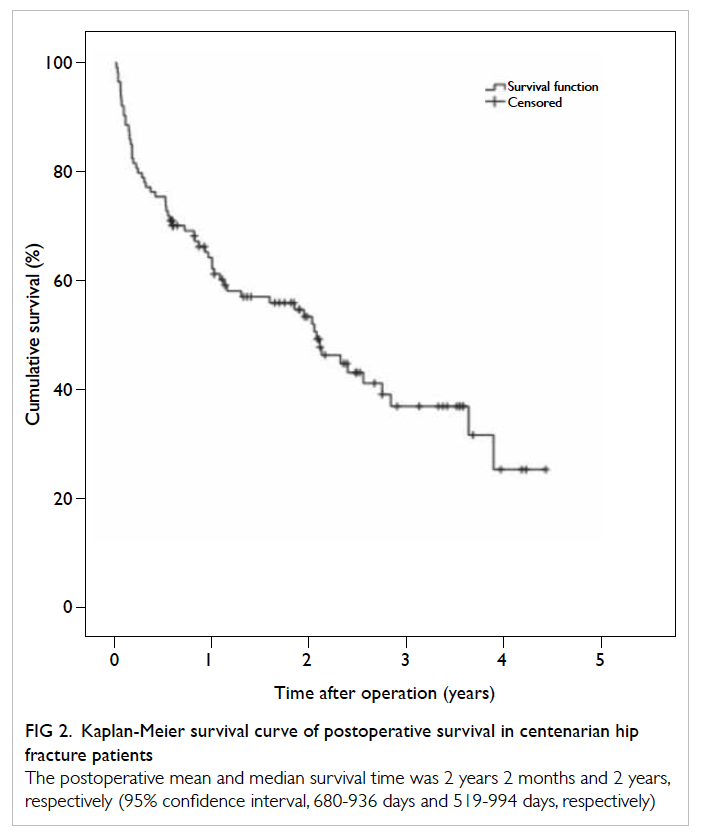
Figure 2. Kaplan-Meier survival curve of postoperative survival in centenarian hip fracture patients
The postoperative mean and median survival time was 2 years 2 months and 2 years, respectively (95% confidence interval, 680-936 days and 519-994 days, respectively)
Discussion
With an increase in life expectancy, the health
care authority is likely to encounter more elderly
patients with hip fracture. The cost of providing
clinical care for centenarians imposes a substantial
financial burden on our health care system. There
are only a few publications that specifically examine
the surgical outcome of centenarians following hip
fracture surgery. Due to their limited sample size,
these studies have failed to justify the need to operate
on centenarians with hip fracture. A previous report
by Tarity et al10 on 23 centenarians reported a 1-year
mortality of 60% and concluded that operating on
patients >100 years carried an acceptable
mortality rate. Patil et al11 reported a high mobility
rate of 77% and a low mortality rate of 8.3% in 13
centenarians, and concluded that hip fracture surgery
yielded a good return on money spent and quality of
life. Shabat et al12 reported a mortality rate of 48% in
23 centenarians and concluded that operated cases
had shorter hospitalisation and patients with two
or more co-morbid diseases had a higher mortality
rate. Only one prospective review has reported the
surgical outcome of patients aged ≥95 years
with the largest sample size of 50 patients.13 They
reported a mortality rate of 36% that was higher than
that of a younger age-group. Predictors of mortality
included the American Society of Anesthesiologists
physical status classification system, number of co-morbidities,
and active medical problems. Despite
numerous studies in different parts of the world,
there are no data for Asian patients.
In our study, the postoperative 1-year mortality
rate for centenarians with hip fracture was 37%. The
postoperative mortality rate of centenarians was
higher than that of hip fracture patients aged >65
years.4 The mortality rate in this study was similar
to that of the abovementioned studies. Nonetheless,
Hong Kong is one of the countries/regions with the longest
life expectancy, and we had the largest sample size of
114 patients compared with previous studies (Table 210 11 12 13).
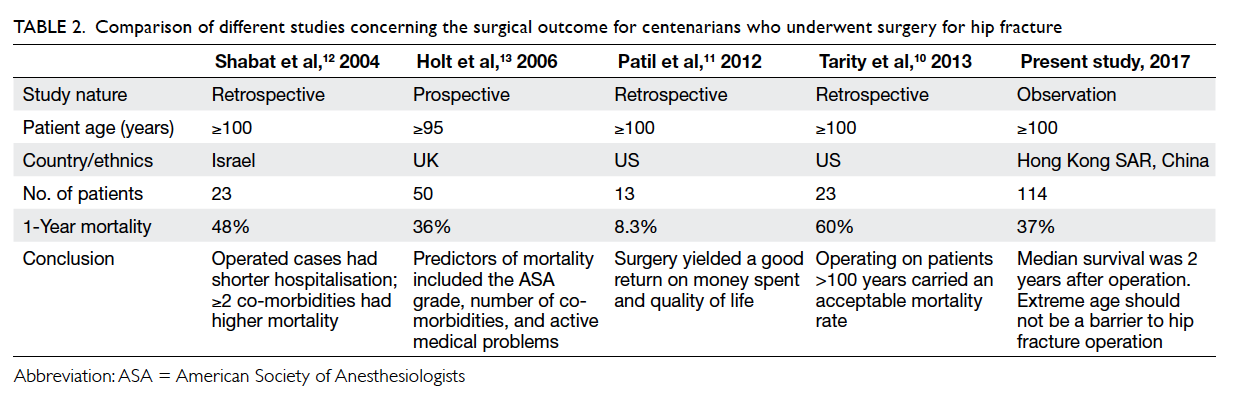
Table 2. Comparison of different studies concerning the surgical outcome for centenarians who underwent surgery for hip fracture
Although two centenarians required ICU
or HDU admission during their hospital stay, the
postoperative 1-year mortality of 37% in our study
is lower than the 41.1% for a general centenarian
population in Japan (P<0.05).14 Those patients in our
study also had a reasonable median postoperative
survival of 2 years.
Previous studies have shown that the benefits
of surgery are not confined to improving mobility, it
also reduces other related complications, improves
patient care, and is more cost-effective than other
non-surgical treatments.15 16 17 Early multidisciplinary
geriatric care also reduces in-hospital mortality
and medical complications.18 Patients who have
undergone hip fracture surgery can be transferred
from an acute unit to rehabilitation as soon as they
are medically stable. In this study, the mean length of
stay on an acute ward was 13.3 days. Weight-bearing
walking exercises can be initiated immediately
after surgery so minimising complications related
to being bedbound. This will also lower the
inevitable costs of acute hospital care. Some of
the centenarians in our study were able to walk
independently with aid following rehabilitation. One
of the most encouraging cases was a 104-year-old
woman who underwent dynamic hip screw fixation
surgery with subsequent cut-out and converted to
cemented unipolar hemiarthroplasty 1 month after
the initial operation. She was able to walk well with a
frame after 2 weeks of rehabilitation and was finally
discharged home.
A limitation of our study was its observational
nature rather than being a prospective randomised
controlled trial. It would be unethical, however, to
randomise patients to have surgery or not and the
sample size would be too small to provide enough
statistical power to demonstrate any significant
difference for this extreme of age. To the best of
our knowledge, our sample size of 114 makes it
the largest study to date of the surgical outcome of
centenarians undergoing hip fracture surgery (Table 2). The present study undoubtedly provides insight into the treatment of centenarians with hip fracture
and should prompt further research on this topic.
Conclusion
The postoperative 1-year mortality rate among Hong
Kong centenarians with hip fracture was 37%, lower
than the 41.1% in the general centenarian population
of Japan. Centenarians also had a reasonable median
survival of 2 years after hip fracture surgery. The
mean length of stay in an acute ward was only 13.3
days. Therefore, surgery for hip fracture, even at
extreme age, is worthwhile to maintain quality of life
for affected patients. Extreme age should not be a
barrier to operative treatment.
Declaration
All authors have disclosed no conflicts of interest.
References
1. Ho AW, Lee MM, Chan EW, et al. Prevalence of pre-sarcopenia
and sarcopenia in Hong Kong Chinese geriatric
patients with hip fracture and its correlation with different
factors. Hong Kong Med J 2016;22:23-9. Crossref
2. Gullberg B, Johnell O, Kanis JA. World-wide projections
for hip fracture. Osteoporos Int 1997;7:407-13. Crossref
3. Lau EM, Lee JK, Suriwongpaisal P, et al. The incidence of
hip fracture in four Asian countries: the Asian Osteoporosis
Study (AOS). Osteoporos Int 2001;12:239-43. Crossref
4. Man LP, Ho AW, Wong SH. Excess mortality for operated
geriatric hip fracture in Hong Kong. Hong Kong Med J
2016;22:6-10.
5. Census and Statistics Department of the Hong Kong SAR
Government. Hong Kong Population Projections 2012-2041. Available from: http://www.statistics.gov.hk/pub/B1120015052012XXXXB0100.pdf. Accessed Dec 2014.
6. Ministry of Health, Labour and Welfare, Government of
Japan. Abridged life tables for Japan 2015. Available from:
http://www.mhlw.go.jp/english/database/db-hw/lifetb15/index.html. Accessed Dec 2014.
7. British Orthopaedic Association. The care of patients with fragility fracture. September 2007. Available from: http://www.fractures.com/pdf/BOA-BGS-Blue-Book.pdf. Accessed
Jun 2016.
8. Lau EM, Cooper C, Wickham C, Donnan S, Barker DJ.
Hip fracture in Hong Kong and Britain. Int J Epidemiol
1990;19:1119-21. Crossref
9. Lau EM, Cooper C, Fung H, Lam D, Tsang KK. Hip fracture
in Hong Kong over the last decade—a comparison with the
UK. J Public Health Med 1999;21:249-50. Crossref
10. Tarity TD, Smith EB, Dolan K, Rasouli MR, Maltenfort MG.
Mortality in centenarians with hip fractures. Orthopedics
2013;36:e282-7. Crossref
11. Patil S, Parcells B, Balsted A, Chamberlain RS. Surgical
outcome following hip fracture in patients >100 years old:
will they ever walk again? Surg Sci 2012;3:554-9. Crossref
12. Shabat S, Mann G, Gepstein R, Fredman B, Folman Y,
Nyska M. Operative treatment for hip fractures in patients
100 years of age and older: is it justified? J Orthop Trauma
2004;18:431-5. Crossref
13. Holt G, Macdonald D, Fraser M, Reece AT. Outcome after
surgery for fracture of the hip in patients aged over 95
years. J Bone Joint Surg Br 2006;88:1060-4. Crossref
14. Statistics Bureau, Ministry of Internal Affairs and
Communications, the Government of Japan. Statistical
Handbook of Japan 2013. Available from: http://www.stat.go.jp/english/data/handbook/pdf/2013all.pdf. Accessed Dec 2014.
15. Lyons AR. Clinical outcomes and treatment of hip
fractures. Am J Med 1997;103:51S-64S. Crossref
16. Simunovic N, Devereaux PJ, Sprague S, et al. Effect of early
surgery after hip fracture on mortality and complications:
systematic review and meta-analysis. CMAJ 2010;182:1609-16. Crossref
17. Parker MJ, Myles JW, Anand JK, Drewett R. Cost-benefit
analysis of hip fracture treatment. J Bone Joint Surg Br
1992;74:261-4.
18. Vidán M, Serra JA, Moreno C, Riquelme G, Ortiz J. Efficacy
of a comprehensive geriatric intervention in older patients
hospitalized for hip fracture: a randomized, controlled
trial. J Am Geriatr Soc 2005;53:1476-82. Crossref