Hong Kong Med J 2017 Feb;23(1):48–53 | Epub 6 Jan 2017
DOI: 10.12809/hkmj166046
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Out-of-hospital cardiac arrest in Hong Kong: a territory-wide study
KL Fan, FHKAM (Emergency Medicine)1;
LP Leung, FHKAM (Emergency Medicine)2;
YC Siu, FHKAM (Emergency Medicine)3
1 Accident and Emergency Department, The University of Hong Kong–Shenzhen Hospital, Shenzhen, China
2 Emergency Medicine Unit, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Pokfulam, Hong Kong
3 Accident and Emergency Department, North District Hospital, Sheung Shui, Hong Kong
Corresponding author: Dr LP Leung (leunglp@hku.hk)
Abstract
Introduction: Out-of-hospital cardiac arrest is a global health care problem. Like other cities in the world, Hong Kong faces the impact of such events. This study is the first territory-wide investigation of the epidemiology and outcomes of out-of-hospital cardiac arrest in Hong Kong. It is hoped that the findings can improve survival of patients with cardiac arrest.
Methods: This study was a retrospective analysis of
the prospectively collected data on out-of-hospital
cardiac arrest managed by the emergency medical
service from 1 August 2012 to 31 July 2013. The
characteristics of patients and cardiac arrests,
timeliness of emergency medical service attendance,
and survival rates were reported with descriptive
statistics. Predictors of 30-day survival were
evaluated with logistic regression.
Results: A total of 5154 cases of out-of-hospital cardiac arrest were analysed. The median age of patients was 80 years. Most arrests occurred at the patient’s home. Ventricular fibrillation or ventricular tachycardia was identified in 8.7% of patients. The median time taken for the emergency services to reach the patient was 9 minutes. The median time to first defibrillation was 12 minutes. Of note, 2.3% of patients were alive at 30 days or survived to hospital discharge; 1.5% had a good neurological outcome. Location of arrest, initial electrocardiogram rhythm, and time to first defibrillation were independent predictors of survival at 30 days.
Conclusion: The survival rate of out-of-hospital cardiac arrest patients in Hong Kong is low. Territory-wide public access defibrillation programme and cardiopulmonary resuscitation training may help improve survival.
New knowledge added by this study
- The prognosis of out-of-hospital cardiac arrest in Hong Kong remains poor. Location of arrest, a shockable electrocardiogram rhythm on presentation, and short time to first defibrillation predict survival at 30 days.
- Hong Kong is in need of a territory-wide public access defibrillation programme and enhanced cardiopulmonary resuscitation training of the public.
Introduction
Out-of-hospital cardiac arrest (OHCA) is an important health care issue. In a systematic review of over 60 studies, the incidence and outcome of OHCA varied greatly. The mean incidence of adult OHCA globally was estimated to be 55 per 100 000 person-years and the survival-to-discharge rate ranged from 2% to 11%.1 Lack of uniform reporting practices is believed to be one of the reasons for this variability. In Hong Kong (HK), there have been at least four studies since 1995 reporting the outcome of OHCA.2 3 4 5 All were either a single-centre study or recruited cases from a particular district of HK. The survival-to-discharge rate was between 0.5% and 3%.2 3 4 5 There was no estimate of the incidence of OHCA and the reporting style also varied. This study is the first local territory-wide investigation of OHCA. The objective was to evaluate the epidemiology and outcomes of OHCA in HK. It is hoped that lessons can be drawn from the findings to improve OHCA survival locally.
Methods
Hong Kong covers approximately 1100 km2 with a population of about 7.3 million. In 2014, it attracted nearly 61 million overseas visitors.6 The emergency medical service (EMS) is provided by the Hong Kong Fire Services Department (FSD) and is a one-tier system. The EMS dispatchers do not give advice about cardiopulmonary resuscitation (CPR) even when OHCA is reported. Transport is primarily by ground vehicles. The level of training of the ambulance crew is similar to that of an Emergency Medical Technician–intermediate level. In cases of OHCA, in addition to basic life support and defibrillation, emergency crews can provide intravenous fluids and airway management via a laryngeal mask airway. No mechanical CPR device is used. There is no protocol for pre-hospital targeted temperature management. The ambulance crews are not allowed to withhold CPR for OHCA patients prior to arrival at hospital unless it is clearly inappropriate, eg with decapitation or decomposition. Such patients are directly transferred from the scene to the public mortuary. Advance directives or do-not-resuscitate orders are uncommon in HK. Emergent coronary reperfusion and therapeutic hypothermia for OHCA patients who survive to hospital admission is performed in selected hospitals only.
This study was a retrospective analysis of the OHCA database compiled prospectively by EMS personnel from 1 August 2012 to 31 July 2013. Data included characteristics of the patient (age and gender), the cardiac arrest (location, whether the event was witnessed, whether there was bystander CPR or defibrillation with an automated external defibrillator [AED], and initial electrocardiogram [ECG] rhythm detected by the EMS), and the EMS response time (time of recognition, call receipt, arrival at patient’s side, arrival at the emergency department [ED], delivery of bystander CPR, delivery of CPR by EMS, and first defibrillation). Outcome data (whether there was return of spontaneous circulation before arrival at the ED; whether resuscitation was conducted in the ED; whether the patient survived to hospital admission, at 30 days, or to hospital discharge; and neurological status on hospital discharge) were collected by the Medical Director of the FSD from hospital records on the electronic database of the Hospital Authority. Patients of all ages were included in this study. Exclusion criteria were OHCAs caused by trauma or those victims directly transferred to the public mortuary from scene by EMS personnel, and patients not using a ground ambulance. Data were reported according to the Utstein style.7 Descriptive statistics were used to describe the patients, OHCA, and timeliness of the EMS. Patients who survived at 30 days were compared with non-survivors in terms of patient characteristics, OHCA characteristics, and the EMS response time. Significance testing by Chi squared test and Mann-Whitney U test was done for categorical and continuous variables, respectively. A P value of <0.05 was considered statistically significant. To identify predictors of 30-day survival, multivariate logistic regression with backward stepwise selection was performed. Covariates used in the
analysis were age, gender, arrest location, witnessed arrest, bystander CPR, bystander AED, initial shockable rhythm, recognition to activation interval, time taken to reach the patient, time to first defibrillation, and time to ED arrival. Findings are reported as odds ratios with 95% confidence intervals. Model calibration was performed by the Hosmer-Lemeshow goodness-of-fit test. Statistical analysis was performed by the Statistical Package for the Social Sciences (Windows version 23.0; SPSS Inc, Chicago [IL], US). This study was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (Reference number: UW 15-599), with the requirement of patient informed consent waived because of its retrospective nature.
Results
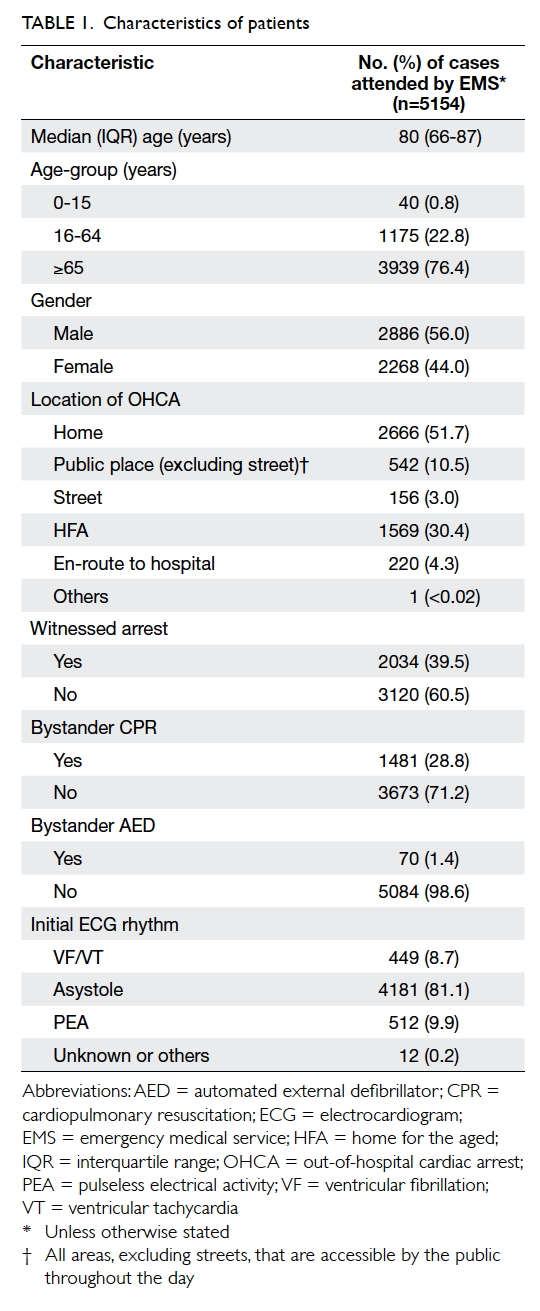
The EMS attended 5154 OHCAs during the study period. This corresponded to 72 arrests per 100 000 persons (based on the Hong Kong Monthly Digest of Statistics published by the Government).8 The median age of patients was 80 years. Males outnumbered females by 12% and approximately 60% of OHCAs were unwitnessed. The arrests most commonly occurred at the patient’s home. Bystander CPR and AED were performed in 28.8% and 1.4% of cases, respectively. Asystole was the initial ECG rhythm on site in approximately 80% of patients. Ventricular fibrillation (VF) or ventricular tachycardia (VT) was evident in only 8.7% of patients (Table 1).
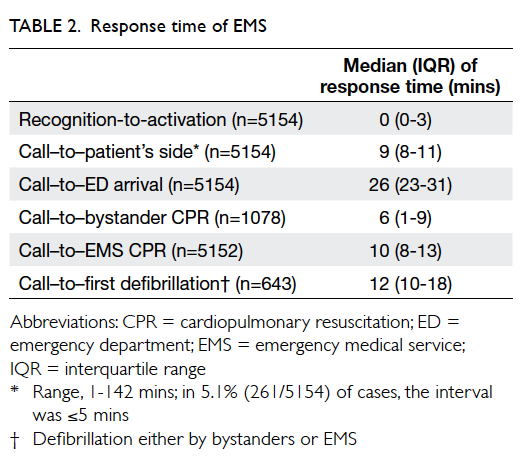
The median response time of the EMS was 9 minutes. The median time to administration of first defibrillation was 12 minutes (Table 2). The time to coronary reperfusion was not available from the database.
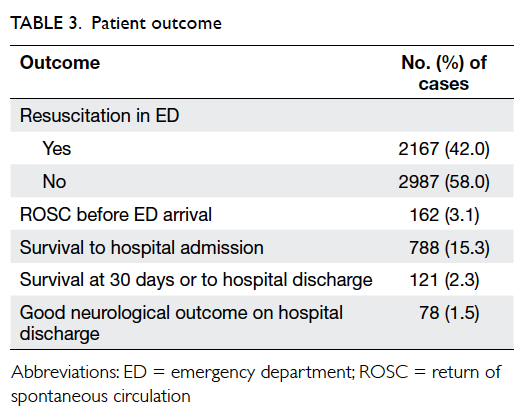
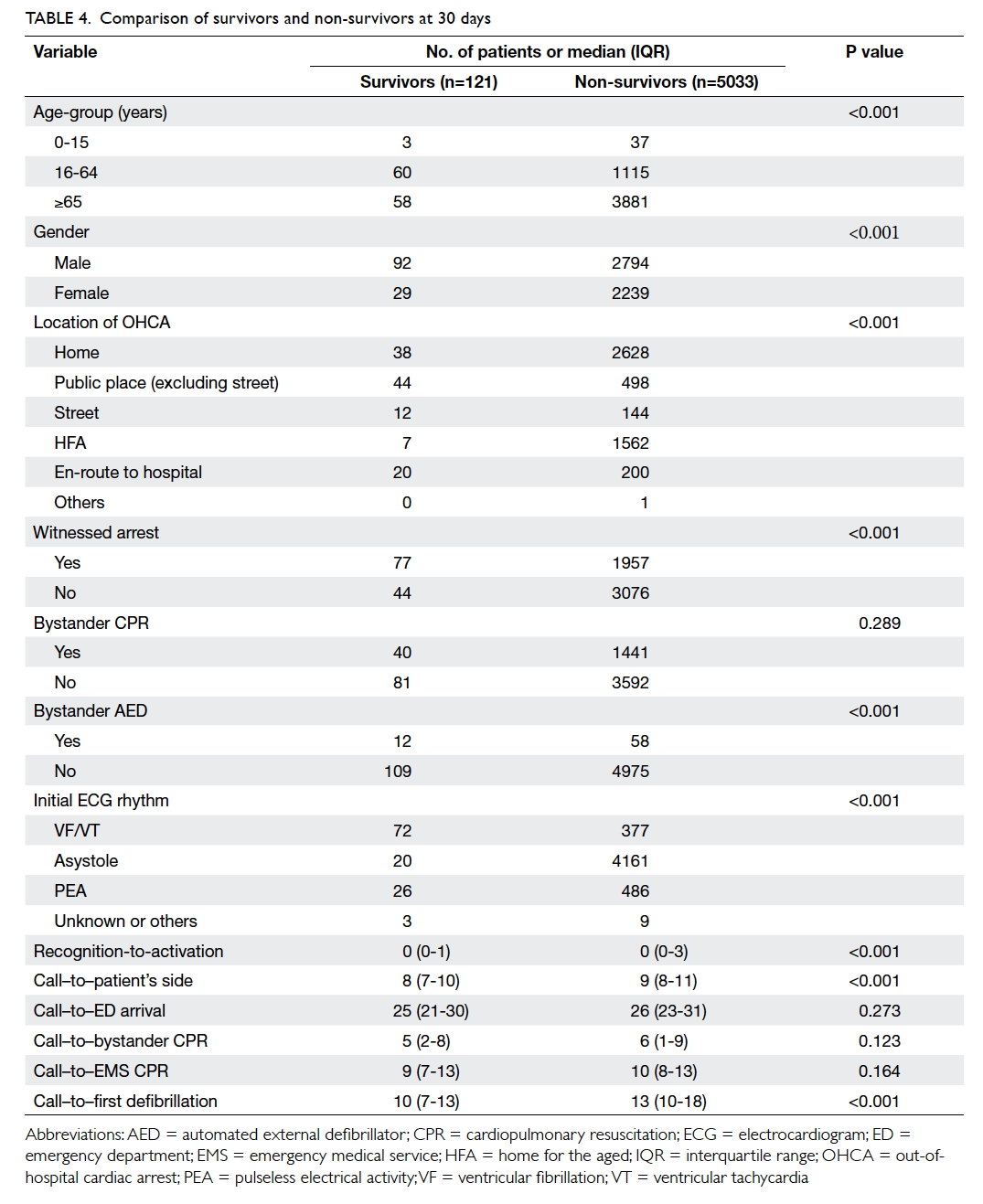
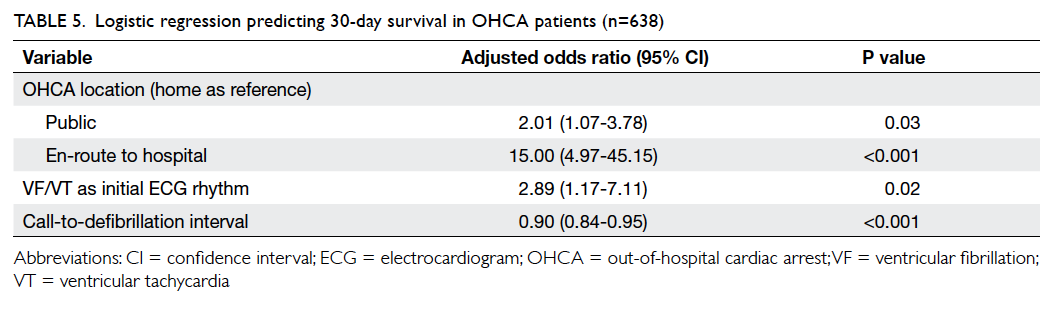
Of the 5154 cases, 162 (3.1%) had return of spontaneous circulation (spontaneous circulation with a palpable pulse) on hospital arrival; 788 (15.3%) patients survived to hospital admission; and 121 (2.3%) were still alive at 30 days or survived to hospital discharge and 78 (1.5%) had a good neurological outcome (defined as cerebral performance category score ≤2) [Table 3]. Survivors and non-survivors were compared, and statistically significant differences were found regarding age, gender, location of arrest, witness status, bystander defibrillation, initial ECG rhythm, recognition-activation interval, time from call receipt to patient’s side, and time to first defibrillation (Table 4). Further analysis with multivariate regression analysis identified location of arrest, initial ECG rhythm, and time from call to first defibrillation as independent predictors of survival at 30 days (Table 5). The Hosmer-Lemeshow test yielded a P value of 0.82.
Discussion
This is the first territory-wide study that reports the epidemiology and outcomes of OHCA in HK. The incidence of 72 arrests per 100 000 persons is higher than the global average of 55 per 100 000 person-years. An ageing population, of whom nearly 15% are older than 65 years, probably contributes to this difference.9 The significance of an ageing population in HK is also reflected by the high median age of 80 years. The OHCA patients in HK are older than those in Japan and are probably the oldest in Asia.10 Nearly 30% of OHCAs occurred in a home for the aged (HFA) or nursing home for the elderly. Whether this is a contributing factor to the relatively low survival rate revealed by this study is unclear. In the 1990s, it was suggested that the prognosis of OHCA in nursing home residents was dismal.11 More recent studies, however, have revealed contradictory results. A Danish study published in 2014 found similar survival rates between nursing home and non–nursing home victims of OHCA.12 On the contrary, a study in Melbourne showed that survival following OHCA that occurred in residential aged care facilities was poorer than that occurred elsewhere.13 In HK where 30% of OHCAs occur in a HFA, the prognosis of local HFA residents with cardiac arrest warrants further investigation. The bystander CPR rate of 28.8% revealed by this study has almost doubled from 15.6% in 1999.3 There is still room for improvement, however. Community-based CPR education programmes are ideal as public knowledge and attitudes towards CPR are poor.14 The rate of defibrillation by bystanders was very low. This is due to the absence of a comprehensive programme of public access to defibrillation in HK. This study also revealed a drop in the percentage of VF/VT as the initial rhythm from 14% in 1999 to 8.7% in this study.15 This decline is compatible with the findings reported elsewhere.16 It remains to be determined whether this is due to the drugs used in treating coronary artery disease.
The local EMS response time (time between call receipt and reaching the patient) of 9 minutes is in the mid-range compared with major Asian cities.10 The call–to–first defibrillation interval of 12 minutes is long. This is probably related to the AED protocol at that time. In cases of unwitnessed arrest, the ambulance crews were required to perform 2 minutes of CPR before rhythm detection. With a time lag of 12 minutes, the chance of successful defibrillation by the EMS would be low. Of note, HK is a highly urbanised and densely populated metropolis. Improving the timeliness of the EMS may be difficult because of traffic congestion. Promotion of public access to defibrillation with a consequent reduced time between OHCA and delivery of the first defibrillation in appropriate patients may improve the success of resuscitation for OHCA victims. Moreover, since 2015, the AED protocol used by the EMS has been amended to immediate rhythm detection even for unwitnessed arrests.
The survival rate of 2.3% in HK is low compared with western countries.1 It is also at the lower range of survival rate among the major Asian cities.10 A high median age of OHCA patients in HK may be a factor, but it is not the only cause. A US study of over 100 000 patients found that age alone was not a good predictor of outcome.17 In another Swedish study, it was found that in the presence of favourable resuscitation factors—eg witnessed arrest, cardiac aetiology with VF as the initial rhythm—a survival rate of 10% could be achieved even in those aged 90 years or above.18 Another explanation for the low survival rate in HK is the low percentage of VF/VT as the initial rhythm. Patients with OHCA with a rhythm other than VF have been shown to have a worse prognosis.15 The low rate of VF/VT may in turn be influenced by the low bystander CPR rate and a large proportion of OHCAs being unwitnessed. Another factor contributing to the low survival rate is that HK EMS personnel have to treat almost every patient with OHCA, even when it is clear they are deceased or have been dead for some time. If a protocol permitted EMS personnel to withhold CPR from the obviously dead, the calculated survival rate would have been higher than 2.3%. Although there was a significant difference between survivors and non-survivors at 30 days or on hospital discharge in terms of age, gender, location of arrest, witness status, bystander defibrillation, initial ECG rhythm, recognition-activation interval, time from call receipt to patient’s side, and call–to–first defibrillation interval, only three were independent predictors of 30-day survival. Arrest occurring en-route to hospital is the most powerful one. This is not unexpected as immediate life support measures can be instituted by the EMS. Collapse in public areas also favours survival as the arrest is more likely to be witnessed and resuscitative measures implemented sooner. The finding that the presence of a shockable initial rhythm and prompt defibrillation favours survival concurs with multiple studies of the relationship between VF/VT in OHCA and survival.19 Bystander CPR was not a significant predictor of survival in this study, contrary to the common belief that bystander CPR improves survival. This raises the concern that in those 28.8% of OHCA victims who received bystander CPR, the quality of CPR was suboptimal. This warrants a separate investigation.
Limitation
The primary limitation of this study was that the analysis was based on data collected for 12 months only and cases not attended by the EMS in the first instance were not included. The latter included an unknown number of patients with advance directives or do-not-resuscitate orders. Data from a longer period of time and the inclusion of cases taken to hospital by means other than ground ambulances or agencies like St John Ambulance should give more accurate results. The analysis of survival was also limited by the lack of data on post-resuscitation care that could have produced a more accurate estimation of the predictors of survival. Furthermore, because of the methodological limitation in the logistic model for 30-day survival predictors, only 638 cases were included for the calculation. Caution is recommended when interpreting survival predictors.
Conclusion
In the presence of an ageing population, OHCA is becoming a significant health care problem in HK. The survival rate of OHCA patients is low. Targeted measures such as implementation of a territory-wide public access defibrillation programme and community-based CPR education and training are needed to improve the chance of survival following OHCA.
Acknowledgments
The authors would like to thank the Hong Kong
Fire Services Department for assistance in data
collection. The authors thank Mr Reynold Leung for
providing technical support to the project, including
data cleaning, statistical analysis, and drawing
figures and tables for manuscript improvement.
Declaration
All authors have disclosed no conflicts of interest.
References
1. Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation 2010;81:1479-87. Crossref
2. Wong TW, Yeung KC. Out-of-hospital cardiac arrest: two and a half years experience of an accident and emergency department in Hong Kong. J Accid Emerg Med 1995;12:34-9. Crossref
3. Leung LP, Wong TW, Tong HK, Lo CB, Kan PG. Out-of-hospital cardiac arrest in Hong Kong. Prehosp Emerg Care 2001;5:308-11. Crossref
4. Wai AK, Cameron P, Cheung CK, Mak P, Rainer TM. Out-of-hospital cardiac arrest in a teaching hospital in Hong Kong: descriptive study using the Utstein style. Hong Kong J Emerg Med 2005;12:148-55.
5. Lau CL, Lai JC, Hung CY, Kam CW. Outcome of out-of-hospital cardiac arrest in a regional hospital in Hong Kong. Hong Kong J Emerg Med 2005;12:224-7.
6. Hong Kong—the facts. Government of Hong Kong Special Administrative Region. Available from: http://www.gov.hk/en/about/abouthk/facts.htm. Accessed Jan 2016.
7. Perkins GD, Jacobs IG, Nadkarni VM, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein Resuscitation Registry Templates for Out-of-Hospital Cardiac Arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation 2015;131:1286-300. Crossref
8. Hong Kong Monthly Digest of Statistics. Government of Hong Kong Special Administrative Region. Available from: http://www.statistics.gov.hk/pub/B10100022013MM12B0100.pdf. Accessed Jan 2016.
9. Census and Statistics Department. Government of Hong Kong Special Administrative Region. Available from: http://www.censtatd.gov.hk/home/. Accessed Jan 2016.
10. Ong ME, Shin SD, De Souza NN, et al. Outcomes for out-of-hospital cardiac arrests across 7 countries in Asia: The Pan Asian Resuscitation Outcomes Study (PAROS). Resuscitation 2015;96:100-8. Crossref
11. Benkendorf R, Swor RA, Jackson R, Rivera-Rivera EJ, Demrick A. Outcomes of cardiac arrest in the nursing home: destiny or futility? Prehosp Emerg Care 1997;1:68-72. Crossref
12. Søholm H, Bro-Jeppesen J, Lippert FK, et al. Resuscitation of patients suffering from sudden cardiac arrests in nursing homes is not futile. Resuscitation 2014;85:369-75. Crossref
13. Deasy C, Bray JE, Smith K, et al. Resuscitation of out-of-hospital cardiac arrests in residential aged care facilities in Melbourne, Australia. Resuscitation 2012;83:58-62. Crossref
14. Chair SY, Hung MS, Lui JC, Lee DT, Shiu IY, Choi KC. Public knowledge and attitudes towards cardiopulmonary resuscitation in Hong Kong: telephone survey. Hong Kong Med J 2014;20:126-33.
15. Fan KL, Leung LP. Prognosis of patients with ventricular fibrillation in out-of-hospital cardiac arrest in Hong Kong: prospective study. Hong Kong Med J 2002;8:318-21.
16. Cobb LA, Fahrenbruch CE, Olsufka M, Copass MK. Changing incidence of out-of-hospital ventricular fibrillation, 1980-2000. JAMA 2002;288:3008-13. Crossref
17. Andersen LW, Bivens MJ, Giberson T, et al. The relationship between age and outcome in out-of-hospital cardiac arrest patients. Resuscitation 2015;94:49-54. Crossref
18. Libungan B, Lindqvist J, Strömsöe A, et al. Out-of-hospital cardiac arrest in the elderly: A large-scale population-based study. Resuscitation 2015;94:28-32. Crossref
19. Sasson C, Rogers MM, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 2010;3:63-81. Crossref