Hong Kong Med J 2017 Feb;23(1):28–34 | Epub 14 Dec 2016
DOI: 10.12809/hkmj164887
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
The pattern of cervical smear abnormalities in marginalised women in Hong Kong
YH Ting, FRCOG, FHKAM (Obstetrics and Gynaecology)1;
HY Tse, FRCOG, FHKAM (Obstetrics and Gynaecology)2;
WC Lam, MPH (CUHK), FHKAM (Obstetrics and Gynaecology)3;
KS Chan, FRCOG, FHKAM (Obstetrics and Gynaecology)4;
TY Leung, LMCHK; DCOGHK5
1 Department of Obstetrics and Gynaecology, The Chinese University of Hong Kong, Prince of Wales Hospital, Shatin, Hong Kong
2 Magnus MRI and Ultrasound Diagnostic Center, Hermes Commercial
Centre, Tsimshatsui, Hong Kong
3 Department of Obstetrics and Gynaecology, Tseung Kwan O Hospital,
Tseung Kwan O, Hong Kong
4 Department of Obstetrics and Gynaecology, Kwong Wah Hospital,
Yaumatei, Hong Kong
5 Well Women Clinic, Tung Wah Group of Hospitals, Yaumatei, Hong Kong
An earlier version of this paper was presented at the 29th International Congress of the Medical Women’s International Association held in Ewha Woman’s University, Seoul, Korea on 31 July to 3 August 2013.
Corresponding author: Dr YH Ting (tingyh@cuhk.edu.hk)
Abstract
Introduction: “Ripple Action” and “WE Stand” are
projects co-organised by the Hong Kong Women
Doctors Association. The two projects organise
free cervical screening for low-income women,
new immigrants from Mainland China, and ethnic
minority women. The objective of this study was to
analyse the pattern of cervical smear abnormalities
in these marginalised women.
Methods: The study group consisted of 1189
marginalised women who participated in a free
cervical screening campaign, including 324 low-income
local Chinese, 540 new immigrants from
Mainland China, and 325 ethnic minority women.
The comparison group consisted of 1141 local
Chinese who attended a well women clinic. The
prevalence of cervical smear abnormalities was
compared using Chi squared test.
Results: In the study group, 42.6% of women had
never had a cervical smear. Compared with the
comparison group, they had a significantly higher
prevalence of cervical smear abnormalities (13.7%
vs 1.4%; P<0.001), including atypical smear (10.8%
vs 0.5%; P<0.001), low-grade lesion (1.8% vs 0.8%;
P=0.036), and high-grade lesion (1.1% vs 0.1%;
P=0.002). Logistic regression analysis showed that
the strongest predictors for abnormal cervical
smear were being South Asian (odds ratio=11.859;
95% confidence interval, 4.635-30.341), South-East
Asian (6.484; 3.192-13.171), or new immigrant from
Mainland China (6.253; 2.463-15.877).
Conclusions: Marginalised women had a
significantly higher prevalence of cervical smear
abnormality than the general population and almost
half had never had a cervical smear before. Outreach
strategies are needed to enrol this population into
screening programmes.
New knowledge added by this study
- Of the marginalised women studied, 42.6% have never had a cervical smear.
- Marginalised women have a significantly higher prevalence of cervical smear abnormality than the general population.
- South Asian, South-East Asian, and new immigrants from Mainland China have a 6- to 11-fold increased risk of cervical smear abnormalities compared with the local Chinese population.
- The Government should be proactive in developing a more comprehensive cervical cancer screening programme in Hong Kong.
- The Government should ensure adequate cervical cancer screening coverage for marginalised women in Hong Kong by developing community outreach programmes through collaboration with non-governmental organisations in the community.
Introduction
Cervical cancer is an important global health problem
in women. It is the fourth most common cancer in
women worldwide with an age-standardised rate
(ASR) of 14.2 per 100 000.1 Cervical screening and
treatment of precancerous lesions have been shown
to reduce the incidence and mortality of cervical
cancer in many developed countries. This remarkable
success has been achieved through organised
screening programmes. Such programmes, however,
are not routinely available in most developing
countries.2 3
Cervical cancer screening in Hong Kong
An organised cervical cancer screening programme
was launched in Hong Kong in 2004 for 25- to
64-year-old women who were currently or previously
had been sexually active.4 The programme does
not proactively recruit eligible women who have
never had a cervical smear. These women must
seek cervical smear services by themselves from
family health service clinics, well women clinics,
general practitioners, or private gynaecologists
for their first smear before they can be registered
under the programme and become eligible for
recall for subsequent smears. Of eligible women in
Hong Kong, 30% have yet to have a cervical smear,
despite the availability of the scheme for 11 years.5
The most common reasons cited were cost, lack of
time, ignorance about cervical cancer and screening,
lack of knowledge about how to access the screening
service, and embarrassment.6 7 8 9 These reasons were
particularly common for marginalised women.
‘Ripple Action’ and ‘WE Stand’
‘Ripple Action’ is a collaborative project launched
by several women professional bodies to serve the
marginalised women in Hong Kong. Collaborating
parties include doctors, nurses, lawyers, accountants,
social workers, and various local women
organisations. ‘WE Stand’ is a project launched
by RainLily in collaboration with the Hong Kong
Women Doctors Association to raise the awareness
about sexual violence against foreign female workers
and ethnic minority women. These two projects
organise free cervical screening events for low-income
women, new immigrants from Mainland
China, and ethnic minority women. The objective
of this study was to analyse the pattern of cervical
smear abnormalities in these marginalised women.
Methods
The study group consisted of women who had a
cervical smear taken in one of the 16 free cervical
screening events held between March 2008 and
November 2014. These women were recruited by
various charitable non-governmental organisations
(NGOs) and included low-income local Chinese
women in receipt of assistance from NGOs, new
immigrants from Mainland China who had lived
in Hong Kong for less than 7 years, and ethnic
minority women mainly from South Asia and South-East Asia. Demographic data, including age, self-reported
ethnicity, date of last menstrual period, and
history of cervical smear were recorded.
Menstruating women and those with a hysterectomy
or no sexual history were excluded from screening.
Informed consent for cervical smear taking was
obtained. Cervical smears were processed using
the ThinPrep Pap Test liquid-based system in an
accredited cytology laboratory and examined by
accredited cytopathologists at a private hospital. All
cervical smear reports were reviewed by specialist
gynaecologists. Women with a normal cervical
smear were called to collect the report in person
from the referring NGO. Women with a cervical
smear abnormality were individually counselled
by a specialist gynaecologist. Women with atypical
smears were referred to a family health service clinic
for a follow-up smear. Women with epithelial lesions
were referred to the gynaecology department in a
public hospital.
The prevalence of cervical smear abnormalities
in the study group was compared with a comparison
group that comprised cervical smear reports selected
from the database of a well women clinic in Hong
Kong. The first 200 of every 1000 sequential smear
reports taken in the four Februarys of the years 2011
to 2014 were selected. To ensure that these reports
were from local Chinese population, reports bearing
foreign names and those with the first alphabet of
the identity card number being R (holders arrived
Hong Kong from 2000 to 2011), M (holders arrived
after 2011), or W (foreign workers) were excluded.
Unsatisfactory smears and vault smears were also
excluded. Statistical analysis of the difference in the
prevalence of cervical smear abnormalities between
the study and the comparison groups was performed
with Chi squared test using the Statistical Package for
the Social Sciences (Windows version 22.0; SPSS
Inc, Chicago [IL], US). A P value of <0.05 was
regarded as statistically significant. Binary logistic
regression analysis was performed to predict the
odds of having a cervical smear abnormality using
the following variables: (1) age; (2) resident in Hong
Kong for less than 7 years; (3) never had a cervical
smear before; (4) ethnicity including local Chinese
(reference group), new immigrant from Mainland
China, South-East Asian (Indonesian, Filipino, and
Thai) or South Asian (Indian, Pakistani, Sri Lankan,
Nepalese, and Bangladeshi). The study was approved
by the Joint Chinese University of Hong Kong–New
Territories East Cluster Clinical Research Ethics
Committee (CREC Ref. No.: 2015.426).
Results
There were 1194 participants across the 16 free
cervical screening events. Five women were excluded
from cervical smear screening because of previous
hysterectomy or current menstruation. Thus, the
study group consisted of 1189 marginalised women,
including 324 low-income local Chinese women
who were receiving assistance from NGOs, 540
new immigrants from Mainland China who were
residents in Hong Kong for less than 7 years, and
325 ethnic minority women mainly from South Asia
and South-East Asia. The characteristics of the study
group, including the self-reported ethnicity, history
of cervical smear, and prevalence of cervical
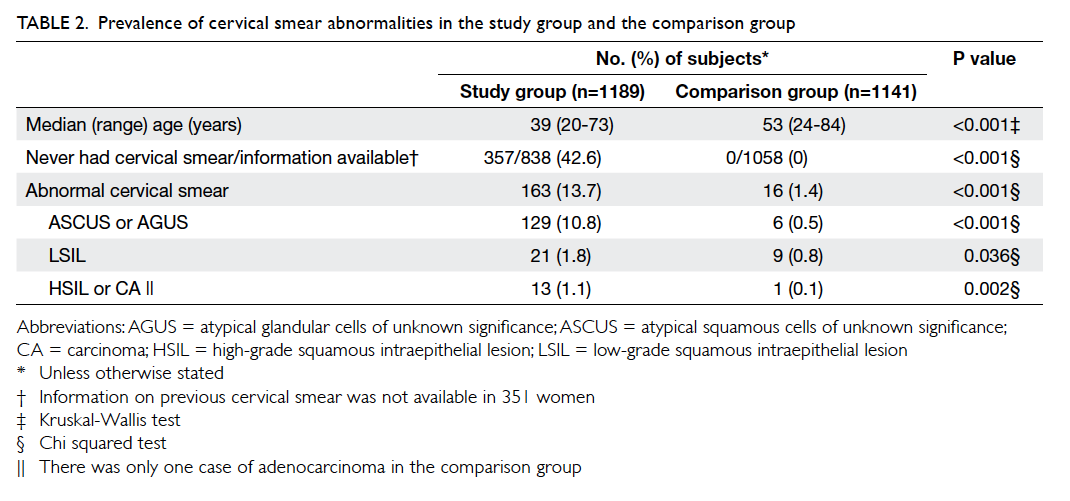
smear abnormalities are shown in Table 1. Among
the 838 women with information available about a history of cervical smear, 357 (42.6%) had
never had a cervical smear. Compared with the local
Chinese in the study group, there were significantly
more ethnic minority women and new immigrants
from Mainland China who had never had a cervical
smear (61.2% vs 45.4% vs 25.0%; P<0.001), and their
prevalence of cervical smear abnormalities was also
significantly higher (20.0% vs 12.8% vs 9.0%; P<0.001)
[Table 1].
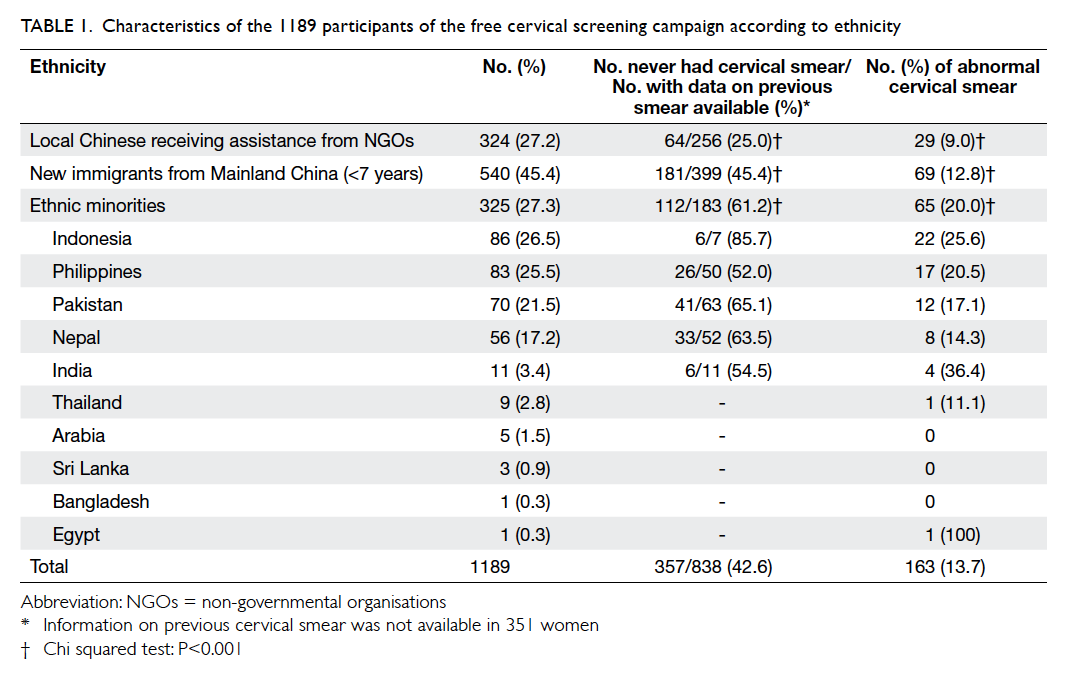
Table 1. Characteristics of the 1189 participants of the free cervical screening campaign according to ethnicity
There were 163 women with cervical smear
abnormalities in the study group, including
129 (79%) atypical cells of unknown significance (ACUS), 21 (13%) low-grade squamous
intraepithelial lesion (LSIL), and 13 (8%) high-grade
squamous intraepithelial lesion (HSIL). Compared
with the 1141 local Chinese women in the comparison group, the
study group had a significantly higher proportion of
women who had never had a cervical smear (42.6%
vs 0%; P<0.001), and a significantly higher prevalence
of cervical smear abnormalities (13.7% vs 1.4%;
P<0.001), including ACUS (10.8% vs 0.5%; P<0.001),
LSIL (1.8% vs 0.8%; P=0.036), and HSIL (1.1% vs
0.1%; P=0.002) [Table 2]. Binary logistic regression
analysis showed that the strongest predictors for
abnormal cervical smear were being South Asian
(odds ratio [OR]=11.859; 95% confidence interval
[CI], 4.635-30.341), South-East Asian (OR=6.484;
95% CI, 3.192-13.171), or a new immigrant from
Mainland China (OR=6.253; 95% CI, 2.463-15.877)
[Table 3].
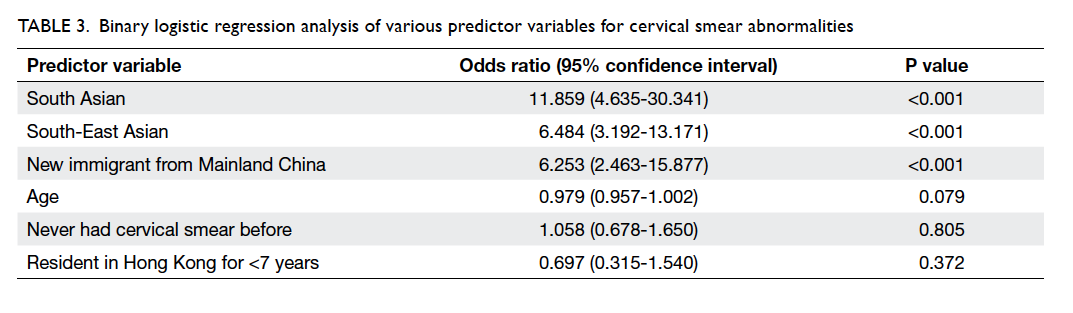
Table 3. Binary logistic regression analysis of various predictor variables for cervical smear abnormalities
We also compared the prevalence of cervical
smear abnormalities in the study group with another
data set that consisted of 509 439 cervical cytology
tests first recorded among registered women in
the Cervical Screening Information System (CSIS)
from the Cervical Screening Programme of the
Department of Health from 2004 to 2014.10 Similar
to the previous findings, the study group once again
had a significantly higher prevalence of cervical
smear abnormalities (13.7% vs 6.3%; P<0.001),
including ACUS (10.8% vs 4.0%; P<0.001) and HSIL
(1.1% vs 0.4%; P=0.005) although the prevalence of
LSIL was not significantly different (1.8% vs 1.9%;
P=0.833) [Table 4].
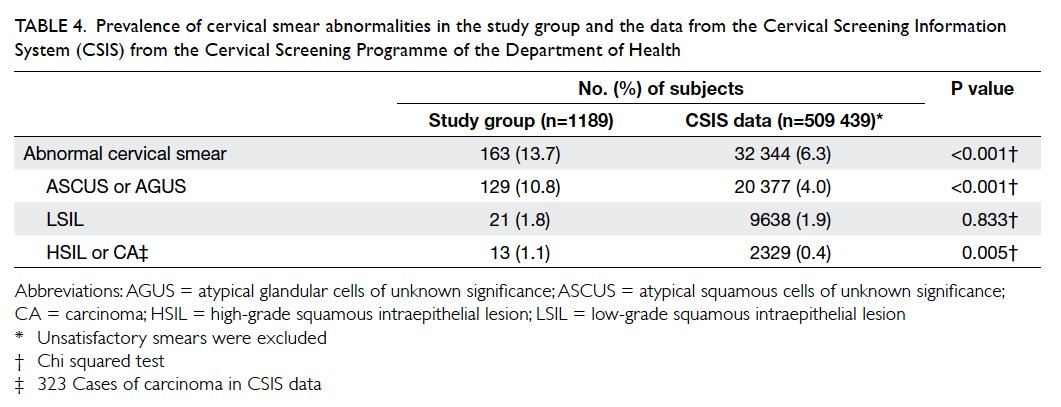
Table 4. Prevalence of cervical smear abnormalities in the study group and the data from the Cervical Screening Information System (CSIS) from the Cervical Screening Programme of the Department of Health
We attempted to contact those women with
an abnormal cervical smear to ensure compliance
with subsequent gynaecological assessment and
treatment after the events and were successful in 58
(36%) instances. Among the 47 women with ACUS,
30 (64%) attended for subsequent assessment, three
underwent colposcopy and one had loop excision. Of
the six women with LSIL, five attended subsequent
assessment of whom four underwent colposcopy and
none required loop excision. All five women with
HSIL attended subsequent colposcopic assessment
and four had loop excision.
Discussion
Cervical cancer is an important health issue for
women in Hong Kong. It is the eighth most common
cancer in the local female population.11 Over the
past three decades, the ASR of cervical cancer has
declined from 25 per 100 000 in 1983 to 8.7 per
100 000 in 2013.11 The figure remains higher than
that of other high-income countries such as Finland
(ASR=4.3 per 100 000).1 After the organised cervical
screening programme was launched, the ever-screened
rate increased from 37% in 2003 to 64%
2008,12 and remained approximately 70% until 2014.5 As this programme does not proactively recruit
eligible women, 30% remain never-screened.5 Studies
show that these women tend to be immigrants or
have a lower socio-economic status with lower
family income.6 7 8 9 13 In Hong Kong, 20% of women
belonged to these groups. In 2012, there were 1.02
million people living below the poverty line in Hong
Kong; 250 000 were adult women and comprised
7.3% of our female population.14 15 In 2011, there were 171 322 mainlanders who had been resident
in Hong Kong for less than 7 years; 80 237 were
women aged 25 to 54 years, comprising 2.3% of our
female population.15 16 Immigrants from other ethnic groups constituted 10.2% of our female population
in 2011; 7% were South-East Asian domestic helpers
from Philippines, Indonesia, and Thailand, and
the remaining 3% were South Asians from India,
Pakistan, and Nepal.15 Studies show that immigrants
often develop cervical cancer at rates more akin to
their country of origin.13 Since these countries have a
high prevalence of cervical cancer with ASR ranging
from 16 to 22 per 100 000,1 it is not surprising that
our study group had a significantly higher prevalence
of cervical smear abnormalities than the comparison
group (13.7% vs 1.4%). This also explains the 6- to
11-fold higher risk of cervical smear abnormalities in
South Asian, South-East Asian, and new immigrants
from Mainland China. More importantly, almost
half (42.6%) of these women had never had a cervical
smear. This was particularly true for ethnic minority
women (61.2%) and new immigrants from Mainland
China (45.4%). This shows that there are inequalities
in our community in the access to cervical screening,
similar to most metropolitan cities worldwide.17 18 The resultant under-screening of high-risk women
and over-screening of low-risk women are clearly
demonstrated by the significant difference in
prevalence of cervical smear abnormalities between
our study group and comparison group. To ensure
that cervical screening services reach these
marginalised women, it is imperative to understand
the barriers to screening.
Cost is a common barrier for low-income
women and immigrants with economic hardship.6 7 8 13
Of the female mainlanders who had been resident in
Hong Kong for less than 7 years, 7.6% were in receipt
of social assistance.16 Foreign domestic helpers earn
only HK$4210 a month. The charge for a cervical
smear provided by the public health sector is HK$100
and may be unaffordable by some women. Even
if the screening service is free, other costs related
to attending screening, such as transportation
and taking time-off work, are deterrents.13 These
barriers can be surmounted by community
outreach that refers to the efforts made beyond
the walls of the health care facility to reach target
populations.19 The first step of outreach is to identify
the target populations and this can be facilitated
by collaboration with NGOs.13 19 Provision of a free service in mobile screening units outside working
hours is also effective.19 Studies also show that the
availability of female service providers helps reduce
embarrassment about cervical cancer screening, and
thus reluctance to attend, among Chinese and other
ethnic groups.6 7 8 13 19 Utilising these strategies, we
organised free screening events during weekends by
women doctors, and we have successfully attracted
almost 1200 marginalised women to participate.
Another important barrier to screening is
ignorance about cervical cancer prevention and
lack of awareness of screening service access,6 7 8 9 13 19 consequent to low health literacy.13 20 Health literacy
refers to how easy it is for an individual to obtain,
process, and understand health information and
services to make appropriate health decisions.13
Low health literacy means that a person is unable to
understand the health information available, access
health services effectively, and make informed
health decisions.20 In other words, health literacy
is dependent not only on the education level and
literacy of the individual, but also on how well health
information is delivered and how accessible the
health service is to the individual. Efforts to improve
health literacy will help reduce health inequalities.20
For women with a low education level or low literacy,
rewriting pamphlets in simple language or employing
non-written forms of communication such as radio
and television programmes are recommended.13 19
In Hong Kong, television programmes designed
to promote cervical cancer screening are available,
but they are broadcast in the local Cantonese
dialect.21 As 68.3% of ethnic minority adults do
not understand Chinese language and 36% of the
new female immigrants from Mainland China do
not speak Cantonese,22 23 they will not benefit from
these programmes. It is worthwhile to translate
these educational materials into different languages.
In our recent free cervical cancer screening events,
health talks on cervical cancer prevention were given
with simultaneous translation into languages spoken
by the participants, aiming to empower them to
become peer health educators in their families and
circle of friends, so that the health literacy in their
community could be improved.
It is now known that cervical cancer is caused
by human papillomavirus (HPV). Vaccination
against HPV for 9- to 13-year-old girls combined
with regular screening for precancerous lesions in
women aged over 30 years followed by adequate
treatment are now the key preventive approaches
against cervical cancer.24 We have launched a free
HPV vaccination programme for 9- to 18-year-old
girls in this marginalised population. Since 2013,
176 girls from low-income families and 24 girls from
ethnic minority groups have been vaccinated. It is
hoped that our free cervical smear programme and
free HPV vaccination programme will help reduce
the incidence of cervical cancer in these marginalised
women.
Limitations
Our study was a retrospective analysis of data
obtained from our free cervical cancer screening
campaign. Limited by the nature of the campaign,
important information such as occupation,
education level, household income, and reasons for
not attending screening was not obtained. Some
data on the history of cervical smear were
missed due to a language barrier. Moreover, self-reported
smear history may not be reliable in this
group of women with low health literacy.
The comparison group may not be ideal as
it may represent an ultra-low-risk population,
as reflected by the low prevalence of cervical
smear abnormalities in these women who had
regular cervical smears. Nonetheless, this is the
only accessible data set from which to obtain the
necessary raw data for analysis. Moreover, limited by
the scarcity of data available on the smear reports
from the Well Women Clinic, the only means to
avoid including women with a similar background to
those in the study group was by excluding reports
bearing foreign names and those with the first
alphabet of the identity card number being R, M, or
W. When we compared the prevalence of cervical
smear abnormalities in the study group with the
CSIS data,10 which may be more representative of the
general population, the findings remained similar
and the prevalence of cervical smear abnormalities
remained 2-fold higher (Table 4).
It would be more informative to have data
about HPV DNA testing on all abnormal smears,
but unfortunately the test was not covered by the
charitable fund. The picture would also be more
complete if the colposcopic or histological diagnosis
of those women with abnormal cervical smears was
available. Such information could not be obtained
without the individual’s consent. We did attempt
to contact these women to ensure compliance with
subsequent gynaecological assessment and treatment
after the event, but were successful in only 36% of
cases as they came from a very mobile population.
It is encouraging that most contactable women with
LSIL or HSIL did attend subsequent assessment,
and almost all with HSIL received treatment. It is
hoped that by identifying and treating precancerous
lesions, our campaign may help reduce the incidence
of cervical cancer in these marginalised women.
Conclusions
The prevalence of cervical smear abnormality in
marginalised women is at least double that of the
general population and almost half had never had
a cervical smear. South Asian, South-East Asian,
and new immigrants from Mainland China had
a 6- to 11-fold increased risk of cervical smear
abnormalities compared with local Chinese
population. The Government should play a proactive
role in developing a more comprehensive cervical
cancer screening programme in Hong Kong and
ensuring adequate coverage for marginalised women
by developing community outreach programmes
through collaboration with community NGOs.
Acknowledgements
We thank the following organisations for
collaboration in the ‘Ripple Action’ and ‘WE Stand’
projects (in alphabetical order): Association of
Women Accountants (Hong Kong) Ltd, GoodNews
Communication International, Hepatitis Free
Generation, Hong Kong Ap Lei Chau Women’s
Association, Hong Kong Employment Development
Service, Hong Kong Federation of Women, Hong
Kong Federation of Women Lawyers, Hong Kong
Island Women’s Association, Hong Kong Nurses
General Union, Hong Kong Outlying Islands
Women’s Association, Hong Kong Playground
Association, Hong Kong Sheng Kung Hui Lady
MacLehose Centre, Hong Kong Sheng Kung Hui
Welfare Council Limited, Hong Kong Women
Doctors Association, International Social
Service Hong Kong Branch, Kowloon Women’s
Organisations Federation, Narcotics Division of
Security Bureau, Po Tat Women’s Association,
RainLily Association Concerning Sexual Violence
Against Women, Social Welfare Department, The
Neighbourhood Advice-Action Council, Village
Volunteers of Hong Kong Sanatorium and Hospital,
Yang Memorial Methodist Social Service Family
Education and Support Centre, and Yuen Long Town
Hall Support Service Centre for Ethnic Minorities.
We thank Dr Ellen Li Charitable Foundation for
funding all the cervical smears in the ‘Ripple Action’
and ‘WE Stand’ projects. We thank Zonta Club of
Kowloon for sponsoring all the HPV vaccines. We
thank Dr KL Mak for retrieving cervical smear
data for the comparison group; Prof DS Sahota for
statistical support; Prof TKH Chung, Prof SSC Ho,
and Prof TC Li for editorial assistance; and Prof HYS
Ngan, the advisor of the ‘Ripple Action’ and ‘WE
Stand’ free cervical screening projects.
Declaration
All the cervical smears taken in the “Ripple Action”
and “WE Stand” projects were funded by Dr Ellen Li
Charitable Foundation. All the HPV vaccines were
sponsored by Zonta Club of Kowloon. All authors
have disclosed no conflicts of interest.
References
1. Ferlay J, Soerjomataram I, Ervik M, et al. GLOBOCAN
2012 v1.0. Cancer incidence and mortality worldwide:
IARC CancerBase No. 11. Lyon, France: International
Agency for Research on Cancer; 2013. Available from:
http://globocan.iarc.fr. Accessed 17 Feb 2016.
2. Denny L, Quinn M, Sankaranarayanan R. Chapter 8:
Screening for cervical cancer in developing countries.
Vaccine 2006;24 Suppl 3:S3/71-7.
3. Gakidou E, Nordhagen S, Obermeyer Z. Coverage of
cervical cancer screening in 57 countries: low average
levels and large inequalities. PLoS Med 2008;5:e132. Crossref
4. Surveillance and Epidemiology Branch, Centre for Health
Protection, Department of Health, Hong Kong SAR
Government. Topical health report No. 4: Prevention and
screening of cervical cancer. Available from: http://www.chp.gov.hk/files/pdf/grp-THR-report4-en-20041209.pdf.
Accessed 17 Feb 2016.
5. Cervical screening programme: statistics and reports.
Available from: http://www.cervicalscreening.gov.hk/english/sr/sr_statistics_ccsc.html. Accessed 17 Feb 2016.
6. Wang LD, Lam WW, Fielding R. Cervical cancer
prevention practices through screening and vaccination: A
cross-sectional study among Hong Kong Chinese women.
Gynecol Oncol 2015;138:311-6. Crossref
7. Wang LD, Lam WW, Wu J, Fielding R. Hong Kong Chinese
women’s lay beliefs about cervical cancer causation and
prevention. Asian Pac J Cancer Prev 2014;15:7679-86. Crossref
8. Holroyd E, Twinn S, Adab P. Socio-cultural influences on
Chinese women’s attendance for cervical screening. J Adv
Nurs 2004;46:42-52. Crossref
9. Adab P, McGhee SM, Yanova J, Wong LC, Wong CM,
Hedley AJ. The pattern of cervical cancer screening in
Hong Kong. Hong Kong Med J 2006;12(Suppl 2):S15-8.
10. Cervical Screening Programme annual statistics report
2014. Available from: http://www.cervicalscreening.gov.hk/english/sr/files/2014_Eng.pdf. Accessed 17 Feb 2016.
11. Department of Health, Hong Kong SAR Government.
Cervical cancer. Available from: http://www.chp.gov.hk/en/content/9/25/56.html. Accessed 14 Sep 2016.
12. Wu J. Cervical cancer prevention through cytologic and
human papillomavirus DNA screening in Hong Kong
Chinese women. Hong Kong Med J 2011;17(3 Suppl 3):S20-4.
13. Schleicher E. Immigrant women and cervical cancer
prevention in the United States. Available from: http://www.jhsph.edu/research/centers-and-institutes/womens-and-childrens-health-policy-center/publications/ImmigrantWomenCerCancerPrevUS.pdf. Accessed 17 Feb
2016.
14. Lam C. Hong Kong’s first official poverty line—purpose
and value. Available from: http://www.povertyrelief.gov.hk/eng/pdf/20130930_article.pdf. Accessed 17 Feb 2016.
15. 2011 Hong Kong Population Census. Population by
ethnicity, sex and economic activity status, 2011 (C110).
Available from: http://www.census2011.gov.hk/en/maintable/C110.html. Accessed 17 Feb 2016.
16. 2011 Hong Kong Population Census. Thematic report:
Persons from the Mainland having resided in Hong Kong
for less than 7 Years. Available from: http://www.statistics.gov.hk/pub/B11200612012XXXXB0100.pdf. Accessed 17
Feb 2016.
17. Grillo F, Vallée J, Chauvin P. Inequalities in cervical cancer
screening for women with or without a regular consulting
in primary care for gynaecological health, in Paris, France.
Prev Med 2012;54:259-65. Crossref
18. Moser K, Patnick J, Beral V. Inequalities in reported use of
breast and cervical screening in Great Britain: analysis of
cross sectional survey data. BMJ 2009;338:b2025. Crossref
19. Comprehensive cervical cancer control: a guide to essential
practice. 2nd ed. Geneva: World Health Organization;
2014.
20. Kanj M, Mitic W. Promoting health and development:
closing the implementation gap. Available from: http://www.who.int/healthpromotion/conferences/7gchp/Track1_Inner.pdf. Accessed 17 Feb 2016.
21. Twinn SF, Holroyd E, Fabrizio C, Moore A, Dickinson JA.
Increasing knowledge about and uptake of cervical cancer
screening in Hong Kong Chinese women over 40 years.
Hong Kong Med J 2007;13(Suppl 2):S16-20.
22. 2011 Hong Kong Population Census. Thematic report:
Ethnic minorities. Available from: http://www.statistics.gov.hk/pub/B11200622012XXXXB0100.pdf. Accessed 17
Feb 2016.
23. Central Policy Unit, Hong Kong SAR Government. A
study of new arrivals from Mainland China; 25 Jan 2013.
Available from: http://www.cpu.gov.hk/doc/en/research_reports/A_study_on_new_arrivals_from_Mainland_China.pdf. Accessed 17 Feb 2016.
24. Comprehensive cervical cancer prevention and control—a
healthier future for girls and women: WHO guidance note.
World Health Organization; 2013.