Hong Kong Med J 2016 Dec;22(6):576–81 | Epub 24 Oct 2016
DOI: 10.12809/hkmj164970
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Sexual violence cases in a hospital setting
in Hong Kong: victims’ demographic, event
characteristics, and management
WK Chiu, MB, ChB, MRCOG1;
WC Lam, MRCOG, FHKAM (Obstetrics and Gynaecology)1;
NH Chu, MRCP (UK), FHKAM (Emergency Medicine)2;
Charles KM Mok, FRCOG, FHKAM (Obstetrics and Gynaecology)1;
WK Tung, FRCSEd, FHKAM (Emergency Medicine)2;
Frances YL Leung, FHKAM (Emergency Medicine)3;
SM Ting, FRCSEd, FHKAM (Emergency Medicine)3
1 Department of Obstetrics and Gynaecology, United Christian Hospital, Kwun Tong, Hong Kong
2 Department of Accident and Emergency, Kwong Wah Hospital, Yaumatei,
Hong Kong
3 Department of Accident and Emergency, United Christian Hospital, Kwun Tong, Hong Kong
This paper was presented at the 2015 Western Pacific Regional
Conference of Medical Women’s International Association, 24-26 April
2015, Taipei, Taiwan.
Corresponding author: Dr WC Lam (lam_mona@hotmail.com)
Abstract
Introduction: Rainlily, the first one-stop crisis
centre in Hong Kong, was set up in 2000 to protect
female victims of sexual violence. This study aimed
to analyse the characteristics of sexual assault cases and victims
who presented to two hospitals
in Hong Kong. The data are invaluable for health care
professionals and policymakers to improve service
provision to these victims.
Methods: This retrospective analysis of hospital
records was conducted in two acute hospitals under
the Hospital Authority in Hong Kong. Sexual assault
victims who attended the two hospitals between May
2010 and April 2013 were included. Characteristics
of the cases and the victims, the use of alcohol and
drugs, involvement of violence, and the outcome of
the victims were studied.
Results: During the study period, 154 sexual assault
victims attended either one of the two hospitals.
Their age ranged from 13 to 64 years. The time from
assault to presentation ranged from 1 hour to more
than 5 months. Approximately 50% of the assailants
were strangers. Approximately 50% of victims
presented with symptoms; the most common were
pelvic and genitourinary symptoms. Those with
symptoms (except pregnancy) presented earlier than
those without. The use of alcohol and drugs was
involved in 36.4% and 11.7% of cases, respectively.
Approximately 10% of the screened victims were
positive for Chlamydia trachomatis. There were
11 pregnancies with gestational age ranged from
6 weeks to 5 months at presentation. Less than half
of the victims completed follow-up care.
Conclusions: Involvement of alcohol and drugs is
not uncommon in sexual assault cases. Efforts should
be made to promote public education, enhance coordination
between medical and social services, and
improve the accessibility and availability of clinical
care. Earlier management and better compliance with
follow-up can minimise the health consequences
and impact on victims.
New knowledge added by this study
- A significant proportion of sexual assault cases involved the use of alcohol (36.4%) or drugs (11.7%). This number may be underreported. Physical violence with or without verbal threat was reported in approximately 30% of cases. Half of the victims attended hospital more than 3 days after the incident when emergency contraception would be less effective.
- Blood and urine samples for toxicology screening should be obtained in selected sexual assault cases. Public education should focus on primary prevention, the means of seeking help, and the importance of early medical care. A territory-wide case review may offer a better evaluation of the problem in Hong Kong.
Introduction
Sexual violence refers to sexual activity where
consent is not obtained or freely given.1 The World
Health Organization defines sexual violence as “any
sexual act, attempt to obtain a sexual act, or other act
directed against a person’s sexuality using coercion,
by any person regardless of their relationship to the
victim, in any setting”.2 This includes rape, indecent
assault, sexual harassment and threats. According
to the statistics of ‘Child abuse, spouse/cohabitant
battering and sexual violence cases’ from the
Social Welfare Department, the majority (88.4%) of
newly reported sexual violence cases in Hong Kong
are indecent assault and 8.8% are rape or unlawful
sexual intercourse. More than 96% of the victims are
females. Approximately 70% of the perpetrators are
strangers, and the rest are usually someone known to
the victim, such as a family member, friend, lover or
ex-lover, co-worker, caregiver, neighbour, or teacher.3
Sexual violence is usually underreported because
of fear: fear of physical examination, disclosure of
sexual history, repeating the traumatic experience
in full detail over and over again, complicated legal
procedures, not being believed by others, and being
harmed by the perpetrator(s).2
Sexual violence may lead to health consequences
such as unwanted pregnancy, sexually transmitted
disease (STD) infections, physical trauma,
depression, and post-traumatic stress disorder.4
Not all victims will seek medical care, however,
because the experience of sexual violence is seen as
stigmatising and shameful, with possible extreme
social consequences.5 Stigmatisation not only from
society but also from health care providers, family,
and even the intimate partner is common. This leads
to minimal support for the victims who may distance
themselves by withdrawing from social activities.6
In November 2000, the Association Concerning
Sexual Violence Against Women set up the first one-stop
crisis centre in Hong Kong, Rainlily, for the
protection of female victims of sexual violence. All
the social workers at Rainlily are female and trained
to provide counselling and care for victims of sexual
assault. They will accompany the victim for medical
care, police interviews, legal proceedings, and most
importantly, the possibly long and difficult recovery
period from the incident.
For many years, Rainlily has worked with the
accident and emergency department of Kwong Wah
Hospital to provide one-stop service to victims
of sexual violence including pregnancy prevention,
screening and prevention of STDs, forensic medical
examination, psychological support, and reporting
to the police if desired by the victim. This avoids
recalling and repeating the unpleasant experience
for different professionals and hence minimises
the need for the victim to psychologically re-live
the trauma. Since May 2010, Rainlily has also
collaborated with the United Christian Hospital and
set up an additional rape crisis centre.
We conducted a retrospective analysis of
female victims of sexual assault who were seen at
either hospital to evaluate the characteristics of
the cases and the victims, the use of alcohol and
drugs, involvement of violence, and the outcome
of the victims. The data are invaluable for health care
professionals and policymakers for improving
service provision for victims.
Methods
All female sexual assault victims who attended the
Kwong Wah Hospital or United Christian Hospital
from May 2010 to April 2013 were included in this
retrospective study. The sexual assault cases were
identified from the special case list of the accident
and emergency department of each hospital and
the designated gynaecology clinic booking list of
the United Christian Hospital. The clinical records
were reviewed and the demographics of the victims,
time lapse from assault to presentation at hospital,
characteristics of the assault, investigations and
results, treatment and outcome of the victims were
analysed.
At Kwong Wah Hospital, the sexual assault
cases were managed and followed up in the accident
and emergency department, with referral to
gynaecologists if clinically indicated, for example,
for unwanted pregnancy. At the United Christian
Hospital, cases were initially managed in the accident
and emergency department with subsequent follow-up
in the gynaecology clinic. At initial presentation,
victims were screened for the presence of any
infection, including STDs. Emergency contraception
was prescribed if necessary. Subsequent follow-up
was after 2 weeks, 6 weeks, 3 months, and 6 months
to exclude pregnancy, to review investigation results
and treat any infection.
The study protocol complied with the
good clinical practice of ICH (The International
Conference on Harmonisation of Technical
Requirements for Registration of Pharmaceuticals
for Human Use). Ethical approval was obtained from
Clinical Research Ethics Committee of Hospital Authority.
All statistical analysis of data was performed
by PASW Statistics 18, Release Version 18.0.0 (SPSS,
Inc, 2009, Chicago [IL], US). For continuous data
with a highly skewed distribution such as time from
the incident of assault to presentation at the hospital,
Mann-Whitney U test was used. The critical level of
statistical significance was set at 0.05.
Results
Demographics of victims
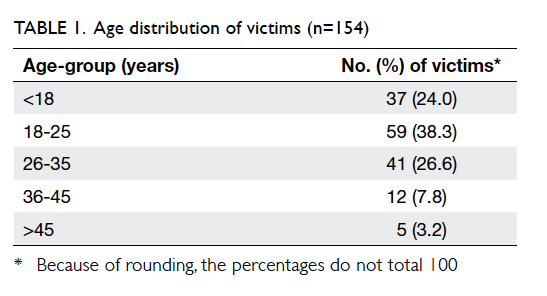
From May 2010 to April 2013, a total of 154 sexual
assault victims had attended either hospital; 102 at
Kwong Wah Hospital and 52 at United Christian
Hospital. The age of victims ranged from 13 to 64
years (mean 24.5 years, median 22 years; Table 1). Most (150 cases; 97.4%) victims were Chinese and four were domestic helpers from other Asian
countries. Five (3.2%) victims were mentally disabled
and 19 (12.3%) had a history of psychiatric disorder.
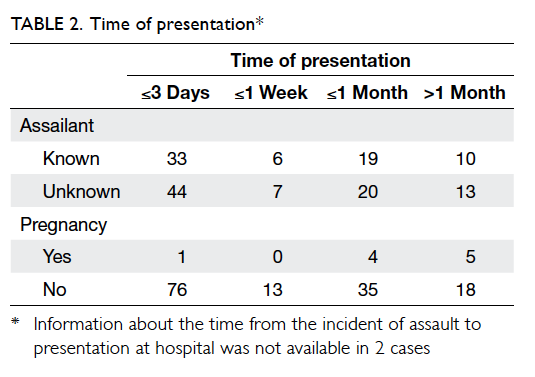
Time between assault and presentation
The time from the incident of assault to presentation
at the hospital ranged from 1 hour to more than 5
months (mean 16 days, median 3 days). Half of the
victims (n=77) attended hospital within 3 days of
the incident. Approximately half (n=84, 54.5%) of
the assailants were strangers (Table 2); the others
included friend, internet friend, family member,
classmate, colleague, employer, boyfriend, ex-boyfriend,
and ex-husband.
The median time from the incident to
presentation was 48 hours (interquartile range
[IQR], 24-240 hours) for victims with symptoms
(except pregnancy), compared with 288 hours for
those without (IQR, 48-696 hours) [P<0.001]. Those
who were pregnant (median time, 756 hours; IQR,
510-1386 hours) presented later than those who
were not (median time, 72 hours; IQR, 24-432 hours)
[P<0.001].
Characteristics of the incident
In 56 (36.4%) cases, alcohol was involved in the
incident. There were 18 (11.7%) cases where drugs
were involved, including ketamine, amphetamine,
methamphetamine, cocaine, and midazolam. In one
victim, multiple drugs were involved. Some victims
could not identify which drug they had been given. It
had either been added to the victim’s drink, or been
given as ‘flu medication’ or an ‘anti-drunk pill’.
There were 133 (86.4%) victims with
documented vaginal penetration, of whom 25
had also been exposed to oral penetration, five
to anal penetration, and four to all three forms of
sexual assault. There were three victims in whom
penetration was oral only. The remaining 18 victims
had no clear documentation. In only three (1.9%)
cases did the assailant use a condom. Verbal threats
were reported by six (3.9%) victims, and physical
violence with or without verbal threat by 45 (29.2%).
Reported physical violence included restraint,
strangling, beating, grasping, and biting.
Presenting symptoms
Apart from the incident, 75 (48.7%) victims presented
with other associated problems, most (n=44, 28.6%)
with pelvic or genitourinary symptoms such as
lower abdominal pain, vaginal discharge, or urinary
symptoms. There were 17 (11.0%) victims who
complained of laceration, contusions, bruises, and
pain due to physical violence during the incident.
Another 12 (7.8%) victims presented with psychiatric
or mood problems: two attempted suicide, one had
auditory hallucinations, and the others had mood
problems or post-traumatic stress disorder with
nightmares and flashbacks. One victim presented
with per rectal bleeding due to anal penetration and
another presented with recurrent oral ulcers in which
oral penetration was involved during the incident.
Seven victims had found themselves pregnant before
attending the hospital.
Sexually transmitted diseases
Blood testing for hepatitis B surface antigen was
performed in 146 victims of whom six (4.1%) were
positive. All positive results were obtained within
6 weeks of the sexual assault. Hepatitis B surface
antibodies were not present in 85 of 134 victims
tested. Hepatitis B immunoglobulin was given to 43
victims and a first dose of hepatitis B vaccination to
52. Only 29 victims completed the course of hepatitis
B vaccination, however, and the remainder defaulted
from follow-up.
Blood test for syphilis by rapid plasma reagin
was positive in one victim and was performed
around 4 days after the sexual assault. Treponema
pallidum haemagglutination assay was also positive.
There was no other positive case in the subsequent
screening at 6 weeks and 6 months. A similar result
was obtained when testing for anti–hepatitis C
virus antibody that was positive in one victim and
the test was performed within 1 day of the sexual
assault. There was no other positive case identified
at subsequent follow-up. Blood tests for anti–human
immunodeficiency virus antibody were all negative
and a total of 71 victims had negative serology 6
months after the alleged assault.
High vaginal and endocervical swabs were
taken for culture and revealed one victim with
Trichomonas vaginalis. Urethral, rectal, and throat
swabs were taken in selected cases and no infection
other than with Candida species was detected.
Chlamydia trachomatis was tested by polymerase
chain reaction test on a urine sample or endocervical
swab in 110 victims, and 12 (10.9%) were positive.
Among those with chlamydial infection, four
presented with genitourinary symptoms such as
perineal pain, vaginal discharge, urinary frequency,
and dysuria.
Pregnancy
Emergency contraception was provided to 63 of the
77 victims who presented within 3 days of the alleged
rape. There were 10 victims who had been prescribed
emergency contraception, either by other doctors, or
self-prescribed from a pharmacy. Other reasons for
not prescribing emergency contraception included a
victim with only oral penetration, one victim with
a previous hysterectomy, two victims taking reliable
regular contraception, and one victim who refused
the prescription.
There were a total of 11 pregnancies as a result
of the incident, among them one victim had received
emergency contraception within the day of assault.
The gestational age ranged from 6 weeks to 5 months
at presentation. Eight cases underwent termination
of pregnancy, one underwent medical evacuation for
silent miscarriage, one continued the pregnancy
to term, and one defaulted from follow-up with
unknown outcome.
Attendance at follow-up
Attendance at follow-up was 57.8%, 63.6%, 59.1% and
46.8% at 2 weeks, 6 weeks, 3 months, and 6 months,
respectively after the incident. Overall, less than half
of the victims completed follow-up care.
Discussion
Every 2 to 3 minutes, one woman is sexually assaulted
somewhere in the world.7 The prevalence of sexual
violence differs across populations, but studies have
consistently shown there to be underreporting
in both developed and developing countries.5 It is
believed that Hong Kong is no different. The reported
cases may only be the tip of the iceberg. This makes
prevention, detection, and proper care difficult.
Comparison with a similar study conducted
in Hong Kong from 2001 to 2004 by Chu and Tung8
shows that the age of victims, time between assault
and presentation, and the percentage of those lost
to follow-up are similar; thus the characteristics
appear unchanged over the past decade. This raises
the question of whether we are doing enough to
promote awareness, prevention, and education in
society.
A considerable proportion of victims have a
history of psychiatric disorder, and there is emerging
evidence of the association.9 Although the causal
relationship is not well understood, it might be due
to the higher prevalence of alcohol or substance
abuse among this population. Nonetheless, a history of
alcohol or substance abuse was not always documented
in the case notes. Patients having a certain type of
psychiatric disorder—such as schizophrenia, bipolar
disorder, and heroin addiction—are more likely to
adopt risky behaviour,10 and hence are at higher risk
of being sexually abused.
The delayed presentation among victims of
assault by a known assailant may be due to the fear of
being discovered by the assailant and being further
harmed. Furthermore, sexual violence is associated
with stigma in some communities, even in cases
with an unknown assailant; the victims may be
afraid of being blamed, and there is also a perceived
lack of support from families and friends.11 Delayed
presentation may result in loss of forensic evidence,
delay in prescription of STD prophylaxis, and a
missed chance for emergency contraception.12 This
explains why those who were pregnant presented
later than those who were not, and those without
symptoms may not have sought help until they found
themselves pregnant. Public education definitely
has a role and must emphasise the importance of
seeking medical care early and promote community
awareness of prevention, instead of blaming the victims.
The prevalence of sexual assault involving
alcohol or drug use in this study was similar to a
previous study by Hurley et al.13 Females are more
vulnerable to the effects of alcohol because of their
smaller body mass and higher proportion of body
fat. Compared with drugs, there is a higher rate of
alcohol involvement in sexual assault cases because
it is easily available, cheap, and legally and socially
acceptable. Alcohol can cause disinhibition and
impair judgement; most of the victims consumed
alcohol voluntarily and therefore there is a strong
feeling of self-blame after the incident. Recreational
drugs consumed by victims themselves or ‘date rape
drug’–spiked drinks given to victims can cause
sedation, anterograde amnesia, and incapacitation.
The actual prevalence is likely to be more than
reported, as the victims may not be aware of the
assault or only have patchy recall of events. Some
of these victims have an intense fear of internet
exposure of their body or the incident, and feel a loss
of control and sense of insecurity. If a drug abuser
is assaulted, they may worry about being charged
and are reluctant to report the incident to the police.
Delay in reporting or seeking help results in loss
of forensic evidence and delay in prescription of
emergency contraception. The current protocol of
the two studied units did not include toxicological
analysis. Therefore the drug used was based on the
victim’s report and recall error is highly likely. In
order to improve service provision and to help in
crime recollection, blood, urine, and nasal swabs for
toxicology screening should be obtained in selected
sexual assault cases. Public education should
emphasise the harmful effects of excessive alcohol
consumption and the effects of combining alcohol
and recreational drugs. Ways to avoid spiked drinks
include keeping an eye on one’s drink, not leaving a
drink unattended or obtaining a new one if it is, and
not accepting a drink from strangers.
The most common presenting symptoms
were pelvic and genitourinary symptoms or
injuries as a result of violence during the incident.
Psychiatric symptoms were usually underreported.
Common symptoms include low mood, fear, guilt,
nervousness, sleeping difficulties, poor appetite, and
feelings of shame and anger. Emotional numbness
and avoidance are common reasons for not seeking
help.14 Moreover, some medical providers do not
actively ask about psychiatric symptoms. Even if
symptoms are reported, they may be considered a
‘normal reaction’ to rape and then ignored. About half
of victims recover from acute psychological effects
by 12 weeks, but in others the symptoms persist
for years.14 Sexual assault survivors are at increased
lifetime risk of post-traumatic stress disorder, major
depression, suicidal ideas and attempts.15 Mental
state and risk of self-harm should be assessed to
identify those who are at risk. Psychosocial support
and opportunities to talk about the incident are
important. For those who do not recover with time,
referral to a psychotherapist or even a psychiatrist is
essential.
Some experts discourage testing for STD
infections in the acute setting unless clinically
indicated by symptoms.15 The positive rate of STD in
this study was low with the exception of chlamydial
infection. Nucleic acid amplification testing can be
carried out on urine samples instead of endocervical
samples, minimising the need for invasive vaginal
examination using a speculum.14 One may consider
omitting the screening test and instead offering
prophylactic antibiotics against bacterial STDs.
The rate of pregnancy (7.1%) is slightly higher
than the quoted risk of 5%.16 The administration
of emergency contraception in the two studied
units comes in the form of levonorgestrel and was
limited to victims who presented within 3 days of
alleged rape. Levonorgestrel is licensed for up to 72
hours after unprotected intercourse, indeed there is
still some residual efficacy after 3 days although it
diminishes with time. To further decrease the chance
of pregnancy, other contraceptive methods can be
considered in victims who present more than 3 days
after the incident, including a copper intrauterine
device or ulipristal acetate. If it is not feasible to
insert an intrauterine device in the emergency
department, urgent referral to a gynaecology clinic
should be considered. Ulipristal acetate may not be
readily available in all public hospitals but it could be
stocked and prescribed as a patient-financed item.
Limitations of this study include the small
sample size, recall bias of alcohol or drug use, loss
of some victims to follow-up, and short follow-up
periods. A territory-wide case review may offer a
better evaluation of the problem in Hong Kong.
Conclusions
Sexual assault is usually underreported and can
lead to significant health consequences. Involvement
of alcohol and drugs is not uncommon in sexual
assault cases. Efforts should be made to enhance coordination
and cooperation between medical and
social services, and improve the accessibility and
availability of clinical care. Health care professionals
should be properly trained to understand the physical
and mental health consequences, the importance of follow-up care, and to equip the skills to manage sexual assault cases. Public education should target at primary prevention, and publicise the simple ways to access the available services.
Acknowledgement
The authors gratefully acknowledge Mr Edward Choi
for his valuable statistical advice.
Declaration
All authors have disclosed no conflicts of interest.
References
1. Understanding sexual violence. National Center for Injury
Prevention and Control, Centers for Disease Control and
Prevention; 2012.
2. Violence against women: preventing intimate partner and
sexual violence against women. Geneva: World Health
Organization; 2011.
3. Statistics on child abuse, spouse/cohabitant battering and
sexual violence cases. Social Welfare Department, the
Government of the Hong Kong Special Administrative
Region; 2014.
4. Welch J, Mason F. Rape and sexual assault. BMJ
2007;334:1154-8. Crossref
5. Dartnall E, Jewkes R. Sexual violence against women: the
scope of the problem. Best Pract Res Clin Obstet Gynaecol
2013;27:3-13. Crossref
6. Jina R, Thomas LS. Health consequences of sexual violence
against women. Best Pract Res Clin Obstet Gynaecol
2013;27:15-26. Crossref
7. Masho SW, Odor RK, Adera T. Sexual assault in Virginia:
A population-based study. Womens Health Issues
2005;15:157-66. Crossref
8. Chu LC, Tung WK. The clinical outcome of 137 rape
victims in Hong Kong. Hong Kong Med J 2005;11:391-6.
9. Goodman LA, Rosenberg SD, Mueser KT, Drake RE.
Physical and sexual assault history in women with serious
mental illness: prevalence, correlates, treatment, and
future research directions. Schizophr Bull 1997;23:685-96. Crossref
10. Hariri AG, Karadag F, Gokalp P, Essizoglu A. Risky
sexual behavior among patients in Turkey with bipolar
disorder, schizophrenia, and heroin addiction. J Sex Med
2011;9:2284-91. Crossref
11. Abrahams N, Devries K, Watts C, et al. Worldwide
prevalence of non-partner sexual violence: a systematic
review. Lancet 2014;383:1648-54. Crossref
12. McCall-Hosenfeld JS, Freund KM, Liebschutz JM. Factors
associated with sexual assault and time to presentation.
Prev Med 2009;48:593-5. Crossref
13. Hurley M, Parker H, Wells DL. The epidemiology of drug
facilitated sexual assault. J Clin Forensic Med 2006;13:181-5. Crossref
14. Cybulska B. Immediate medical care after sexual assault.
Best Pract Res Clin Obstet Gynaecol 2013;27:141-9. Crossref
15. Linden JA. Clinical practice. Care of the adult patient after
sexual assault. N Engl J Med 2011;365:834-41. Crossref
16. Holmes MM, Resnick HS, Kilpatrick DG, Best CL. Rape-related
pregnancy: estimates and descriptive characteristics
from a national sample of women. Am J Obstet Gynecol
1996;175:320-4. Crossref