Hong Kong Med J 2016 Aug;22(4):372–81 | Epub 20 May 2016
DOI: 10.12809/hkmj154686
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
REVIEW ARTICLE
Oral health of Hong Kong children: a historical and epidemiological perspective
Gillian HM Lee, FCDSHK (Paediatric Dentistry), FHKAM (Dental Surgery);
Harry N Pang, FCDSHK (Orthodontics), FHKAM (Dental Surgery);
Colman McGrath, FFDRCS (Ire), PhD (Eng);
Cynthia KY Yiu, FHKAM (Dental Surgery), FCDSHK (Paediatric Dentistry)
Faculty of Dentistry, The University of Hong Kong, Pokfulam, Hong Kong
Corresponding author: Dr Gillian HM Lee (lee.gillian@gmail.com)
Abstract
Objective: To provide a historical and
epidemiological overview of the oral health of Hong
Kong children.
Methods: Literature published before 2014
related to the oral health of Hong Kong children,
supplemented with information accessed from
government-archived oral health reports, was
sourced using electronic databases and hand
searches. Dental caries experience, periodontal
health, enamel defects, and malocclusion of Hong
Kong children were reviewed.
Results: A decline in the prevalence and extent
of dental caries was observed among Hong Kong
schoolchildren and adolescents after the 1960s.
Among preschool children, however, dental caries
remains common and the extent appears to have
increased. The periodontal health of Hong Kong
children remains unsatisfactory. Recently, enamel
defects/dental fluorosis have considerably reduced.
Information about malocclusion in Hong Kong
children is limited.
Conclusions: Since the 1960s, following public
health policies, health promotion activities, and
the introduction of a School Dental Care Service,
improvements in the oral health of schoolchildren
are evident. Nonetheless, the oral health of preschool children
remains a concern. Policies and
practices to improve the oral health of preschool children
in Hong Kong are required.
Introduction
Over the past 50 years, a number of dental public
health measures and policies have been established
by the government in Hong Kong to help improve
the oral health of the population. Children have
been the focus for many of these dental public health
practices since the 1960s and these have included
prevention strategies, oral health education, and the
provision of the School Dental Care Service (SDCS).
Historical development of Hong Kong’s public health measures for children
Water fluoridation is one of the most successfully
implemented dental public health measures in Hong
Kong. The project was launched in 1961 and has
remarkably reduced the prevalence of dental caries
in Hong Kong.1 All areas with a centralised water
supply are fluoridated. Prior to its implementation,
the natural fluoride concentration of drinking
water in Hong Kong was less than 0.13 parts per million (ppm). Several adjustments have been made
to the water fluoride level in Hong Kong since its
implementation: from 0.7 ppm for summer months
and 0.9 ppm for winter months in 1961, to 1 ppm in
1967; then reduced to 0.7 ppm in 1978; and further to
0.5 ppm in 1988 because of concerns of an increased
prevalence of dental fluorosis in the population.
In late 1979, the SDCS was introduced to
provide prevention and dental treatment to primary
schoolchildren in Hong Kong. The SDCS also aims
to promote oral health by delivering oral health
education to schoolchildren. Preschool children
in Hong Kong are not routinely eligible for the
SDCS. They receive oral health care and treatment
largely from dentists working in the private sector.
Oral health education for preschool children was
introduced through the ‘Brighter Smiles for the New
Generation’ programme by the government in 1993.
This programme promotes oral health awareness
by educating children aged under 6 years about
good oral health–related behaviour. It also aims to
increase their teachers’ and parents’ oral health care
knowledge.
The community is served by registered
professional oral health care personnel. The Faculty
of Dentistry at the University of Hong Kong was
established in 1981 and began training dentists and
supporting dental personnel in the same year. More
than one third of local practising dentists have been
educated in Hong Kong.2 The number of practising
dentists currently serving the community has
increased to about 2310 personnel, a per capita ratio
of 1:3125.3 Before 1973, there were only about
440 practising dentists, a per capita ratio of 1:9000. In
the past, it was often only the economic affluent who
sought treatment from private dental practitioners.
For many others, teeth were considered a dispensable
commodity.2 Although this situation has improved,
access to dental care for the Hong Kong population
remains inadequate.
Oral health care products (fluoridated
toothpaste, mouth rinses, toothbrushes, and floss)
are now widely available in Hong Kong.4 These easily
accessible fluoride-containing products provide an
additional benefit to the oral health of the Hong
Kong population. Most locally available toothpastes
have a fluoride concentration of 1000 to 1500 ppm,
while those for children have 600 ppm. Mouth rinse
with 0.05% sodium fluoride is also freely available,
though its use among children is not common and
it is not recommended for the very young.
Over the years, dentistry in Hong Kong has
advanced and oral health care has greatly improved
under several government public health policies.
Although children have been the primary target
of such initiatives, information and review of the
effects of the changes and trends in the oral health
of Hong Kong children are limited. This is in part due
to the limited dissemination of findings, particularly
those of earlier government reports. Understanding
the trends and current oral health condition of
Hong Kong children is important. It can provide a
historical and epidemiological overview of dental
activity and inform the planning of future public
health measures, prevention, and services for
children. It may also help set future oral health
targets and specific goals.
This paper reviews all available oral health
epidemiological data and information of Hong
Kong children from published literature before 2014
through electronic database searches, supplemented
with information accessed from government-archived
oral health reports. Reference lists of
articles retrieved from the electronic databases were
hand-searched for any other articles that might
provide information relevant to the objectives of
this paper. Major oral health problems of Hong
Kong children—including dental caries experience,
periodontal health, enamel defects, malocclusion,
and orthodontic treatment need—are described.
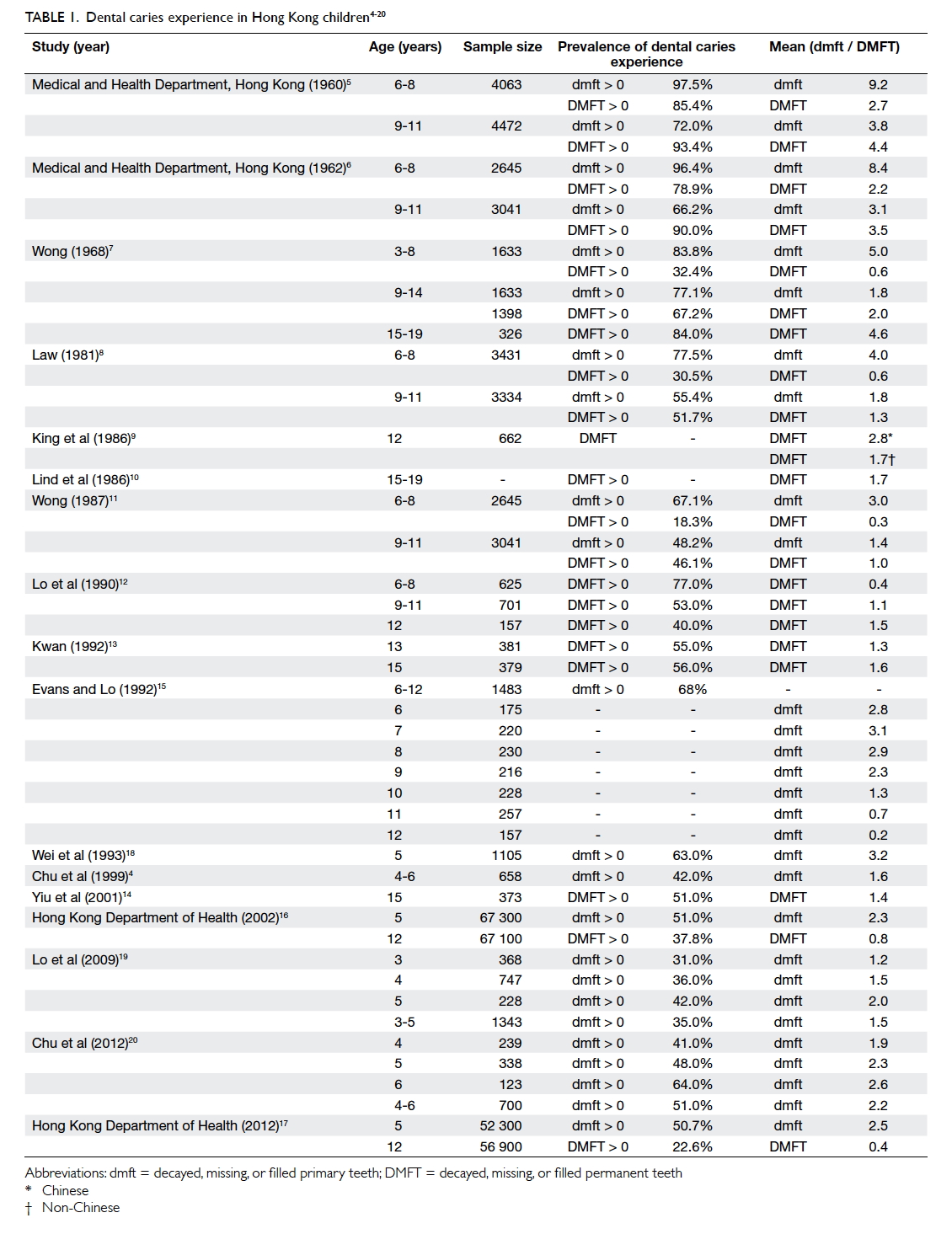
Dental caries experience
A number of population-based oral epidemiological
studies involving children have been conducted in
Hong Kong since the 1960s. Available epidemiological
data regarding dental caries experience and the
extent/severity of dental caries among Hong Kong
children are summarised in Table 1.4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 These studies
employed different sampling methods as criteria of
assessment differed prior to the 1970s. More recent
surveys have followed World Health Organization’s
criteria for caries assessment.
Dental caries experience of schoolchildren and adolescents (aged 6-18 years)
To date, there are 13 population-based
epidemiological studies reporting the prevalence
and extent of dental caries experience among Hong
Kong schoolchildren and adolescents. A remarkable
decrease in caries experience and severity among
schoolchildren and adolescents has been observed
since the 1960s.
The earliest report of dental caries experience
among schoolchildren and adolescents was carried
out in 1960, a year before the implementation of
water fluoridation.5 The epidemiological findings
gave cause for concern. Almost all children aged 6
to 11 years who participated in the study (aged 6-8: 97.5%; aged 9-11: 93.4%) had dental caries. The mean
number of decayed, missing, or filled permanent
teeth (DMFT) in 6-8-year-olds and 9-11-year-olds was 2.7 and
4.4, respectively; the mean decayed, missing, or filled
primary teeth (dmft) in 6-8- and 9-11-year-olds was
9.2 and 3.8, respectively. Decayed teeth constituted
the major component (>90%) of the dmft/DMFT
index in both dentitions, and extracted and filled
teeth components were minimal. This signified
that there were no systematic dental care services
available at the time and with limited preventive
measures.
In 1962, the second population-wide oral
health survey was conducted using similar sampling
methodology to the 1960 survey,6 1 year after the
implementation of water fluoridation. There was a
reported slight decrease in the prevalence of dental
caries experience (for those aged 6-8 years: 96.4%; for
those aged 9-11 years: 90.0%). The mean dmft and DMFT
showed a significant decline of approximately 20%
(mean DMFT: 2.2 for those aged 6-8 years and 3.5 for
those aged 9-11 years; mean dmft: 8.4 for those aged 6-8 years
and 3.1 for those aged 9-11 years). As in the 1960 survey,
decayed teeth constituted the major component of
the DMFT, showing limited change in the provision/usage of dental care services. As this survey was
conducted a year after water fluoridation, the
decrease in dental caries could not be fully explained
by exposure to fluoridated water. No report on the
difference in dmft/DMFT among children who
had received fluoridated water for the whole time,
intermittently, or not at all was provided.
The third oral health survey of Hong Kong was
completed in 1968, 7 years after the introduction of
water fluoridation.7 The sampling method differed to
the earlier surveys. Subjects aged 3 to 54 years were
selected. The dental caries experience in the primary
dentition was 83.8% (mean dmft: 5.0) for 3-8-year-olds, whereas the dental caries experience in the
permanent dentition was 67.2% (mean DMFT: 2.0)
for 9-14-year-olds, and 84.0% (mean DMFT: 4.6) for
15-19-year-olds. It represented a significant decrease
in both caries experience and its extent among
children when compared with previous surveys.
This favourable change was attributed to water
fluoridation as there were no other widely available
caries preventive measures or systematic dental care
services in the 1960s.
In 1980, another population-based dental
health survey collected baseline data for future
evaluation of the SDCS.8 The majority of
schoolchildren (aged 6-11 years) examined were caries-free
in their permanent dentition. The mean DMFT
was <1 for children aged <9 years and 1.5 for 11-year-olds. The caries experience in the primary dentition
of the children was high, however. The mean dmft
for 6-year-olds was 4.3. The number of extracted and
filled teeth for both dentitions was low. More than
90% of decayed teeth were untreated, indicating the
lack of utilisation of dental services and a very high
unmet treatment need.
The epidemiological studies conducted in the
1980s after the commencement of SDCS to monitor
the effect of fluoride on dental caries experience
of Hong Kong schoolchildren and adolescents
after over 20 years of water fluoridation showed a
further decrease in caries experience and severity.
The reported mean DMFT of schoolchildren and
adolescents in these surveys ranged from 0.3 to 2.89 10 11 12
and the mean dmft was 2.2.11 The caries experience
was >65% in primary dentition and 18.3% to 77% in
permanent dentition.11 12 The major component of
the DMFT of the children of this time was decayed
teeth, demonstrating that there was still a high
unmet need for dental services, although the SDCS
was already enacted. Caries was mostly experienced
in molar teeth for children aged 9 to 12 years.
The caries prevalence and extent among Hong
Kong schoolchildren and adolescents continued to
show improvements. Kwan13 reported the first survey
of schoolchildren aged 13 and 15 years who joined
the SDCS in 1992. The dental caries experience
was approximately 55%, with a mean DMFT of 1.3
for 13-year-olds and 1.6 for 15-year-olds. The result
corresponded to a study by Yiu et al14 that reported
a caries experience of 51% and a mean DMFT of 1.4
among 15-year-olds. In 1992, Evans and Lo15 also
studied the effects of the SDCS on the dental status
of primary teeth among a sample of Chinese children
aged 6 to 12 years. The caries experience was 68%,
with dmft indices for 6-, 7-, 8-, 9-, and 10-year-olds being
2.8, 3.1, 2.9, 2.3, and 1.3, respectively. The ratio of
decayed-to-filled teeth decreased from 3.2 at age 6
to 1.0 at age 9. The mean number of filled teeth was
the major component of the dmft index in these
surveys, indicating that many children had received
dental care.
The Hong Kong SAR Government conducted a
population-based survey of the oral health status of
12-year-old children in 2001 and 2011.16 17 More than
one-third (37.8%) of the children in 2001 had a caries
experience in their permanent dentition and in 2011,
22.6% of the children had a caries experience. The
extent/severity of caries was low (mean DMFT: 0.8 in
2001, 0.4 in 2011). Most of the decay experience was
attributed to the filled component. The proportion
of untreated decay was also rather low, with only
5.4% reported to have untreated decayed teeth
in 2011. This positive development in oral health
was associated with reported better oral health
knowledge and oral care habits in both parents and
children. A large number of the participants claimed
they had regular dental check-ups.
In the past 50 years, for Hong Kong
schoolchildren and adolescents, the prevalence
of dental caries experience in permanent teeth
has reduced from more than 90% (in the 1960s) to
approximately 50% in the 1980s/90s and to less than
25% currently. The mean number of DMFT has also
declined from over 4 in the 1960s to approximately 2
in the 1980s/90s, and to less than 1 currently.
Dental caries experience of preschool children (aged ≤5 years)
There were seven epidemiological studies reporting
dental caries experience among preschool children.
Improvement among preschool children is less since
the 1960s, compared with improvements among
schoolchildren and adolescents and it remains a
considerable problem.
The earliest oral health survey that involved
young children was the population-based survey
conducted in 1968.7 The prevalence of dental caries
experience among 3-8-year-old children at that
time was over 80%, with a dmft of 5. One quarter
of the primary teeth of the children were decayed.
The second report of preschool children caries
experience in Hong Kong was drawn up by Wei
et al.18 Conducted between 1986 and 1988 among
approximately 10% of 5-year-old children, the
percentage of children with caries in their primary
dentition was 63%. The mean dmft was 3.2. Dental
caries experience was higher for children from
socio-economically disadvantaged families. Over
70% of the children had never visited a dentist.
The caries experience of Hong Kong preschool children
further decreased to about 50%
in the late 1990s.4 The mean dmft of children
(4-6-year-olds) was 1.6. More than 90% of the dmft score
was attributed to decayed untreated teeth. Similar
to the findings of Wei et al,18 the children’s caries
experience was associated with underprivileged
socio-economic background, and parental educational level, dental knowledge, and attitudes.
In the recent decade, no great changes among
preschool children caries status have been observed.
The caries prevalence in preschool children remains
similar, with a reported prevalence of 35% to
51%.16 17 19 20 The extent/severity of caries, however,
showed a slight increase when compared with the
late 1990s (mean dmft of children aged 3-5 years ranged
from 1.5 to 2.5). Over 90% of the decayed teeth of
the children were untreated. Almost one tenth of
the children presented with abscess, with a higher
percentage reported in the 2011 survey than in the
2001 survey.16 17 These recent surveys also found
that children’s caries experience was associated with
their place of birth, socio-economic background,
and dietary habits.
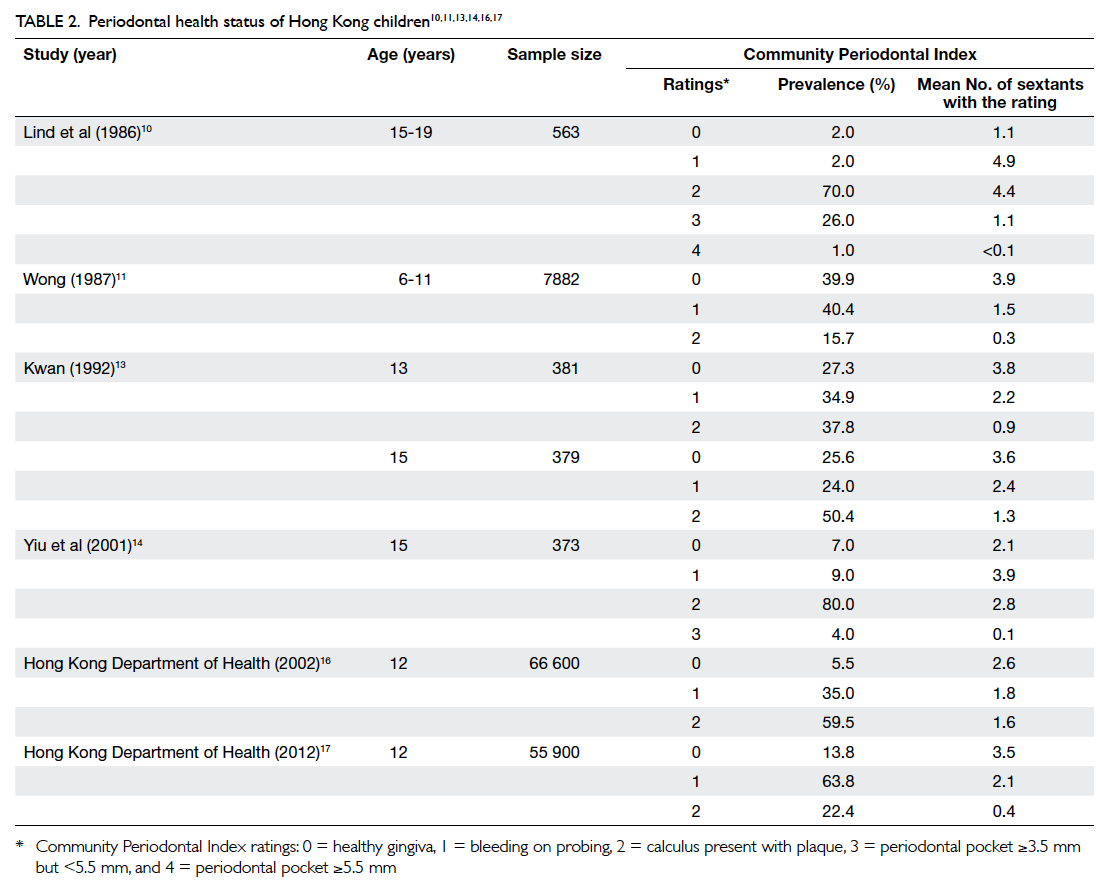
Periodontal health status
Detailed information about the periodontal status
of Hong Kong children is less readily available when
compared with information about dental caries
experience. Different assessment criteria have been
used to assess periodontal health among children
and adolescents, making it difficult to compare
surveys.
The earliest report of the periodontal health
status of Hong Kong children (aged 3-19 years) was
drawn up by Wong in 1968.7 Wong7 reported that
“oral hygiene was only fair in 70% of the children”
and that “over 60% of the children had inflamed
gingiva, and material alba was found on over 90%
of the teeth surfaces”. Inflamed gingiva (gingivitis)
is the reversible and non-destructive form of
periodontal disease. This suggested that the children
had poor periodontal health, though the criteria of
assessment were not defined.
Law8 provided more specific details about the
periodontal health status of 5-14-year-old Hong
Kong children. Approximately 85% were reported
to have soft deposits (assume plaque), of whom approximately one (19.2%) in five had ‘intensive gingivitis’ (inflamed gingiva). Calculus was observed among over a
quarter (26.4%) of the children, and the percentage
of calculus deposits increased with age.
Epidemiological studies conducted in the late
1980s employed the Community Periodontal Index
(CPI) to assess the periodontal health status. It is
the standard epidemiological index for assessing
periodontal health,21 and results of the surveys were
comparable. The epidemiological studies reporting
periodontal health status of Hong Kong children
using the CPI are shown in Table 2.10 11 13 14 16 17 The
majority reported periodontal health status of
adolescents. Among adolescents (13-18 years old),
two of three studies10 13 14 reported that less than
10% had ‘healthy’ periodontal status (CPI=0) and
more than half had evidence of calculus in some
parts of the mouth (CPI=2). This showed that the
periodontal health of Hong Kong adolescents was
unsatisfactory.
For Hong Kong schoolchildren, the first
detailed report of their periodontal health status
was conducted by Wong11 among 7882 primary
schoolchildren (aged 6-11 years) in 1987. More than
half of the sextants (3.9) of the children had healthy
gingiva (CPI=0). Nonetheless, more than half
(56.1%) of the children had bleeding gingiva (CPI=1) or calculus deposits (CPI=2).
Two population-based oral health surveys
among schoolchildren (12-year-old children)
were conducted by the government in 2001 and
2011.16 17 The 2011 survey showed an improvement
in periodontal health status. More schoolchildren
were found to have healthy gingiva (CPI=0) in 2011: 13.8% compared with 5.5% in the 2001 survey; and
less children had calculus deposits (CPI=2) in 2011: 22.4% compared with 59.5% in the 2001 survey. Of
note, more than half of their sextants had either
bleeding gingiva or calculus deposits in 2001 and an
average of two of the sextants had these problems in
2011.
Studies that applied the Visible Plaque Index to assess periodontal health of Hong Kong
preschool children are shown in Table 3.16 17 22 Such Index was introduced by Ainamo and Bay23 as a
standardised assessment of oral hygiene status. It is
simple and reliable to use and has been employed in
surveys as a proxy of gingival health, representing
the site prevalence of ‘clearly visible dental plaque’
at the gingival margin. The oral hygiene of the preschool children
in Hong Kong was poor.16 17 22 Almost all 5-year-old children (97%) had at least one site
with ‘clearly visible dental plaque’.16 17 The mean percentage of tooth surfaces with visible dental
plaque was 22.1% in 2011 and 23.5% in 2001. A study
conducted among 531 children aged 3 to 4 years in
2009, however, reported that 49.7% of the tooth
surfaces had visible plaque.22 In general, the gingival
condition and tooth cleanliness of both schoolchildren
and preschool children were unsatisfactory and
required much improvement.
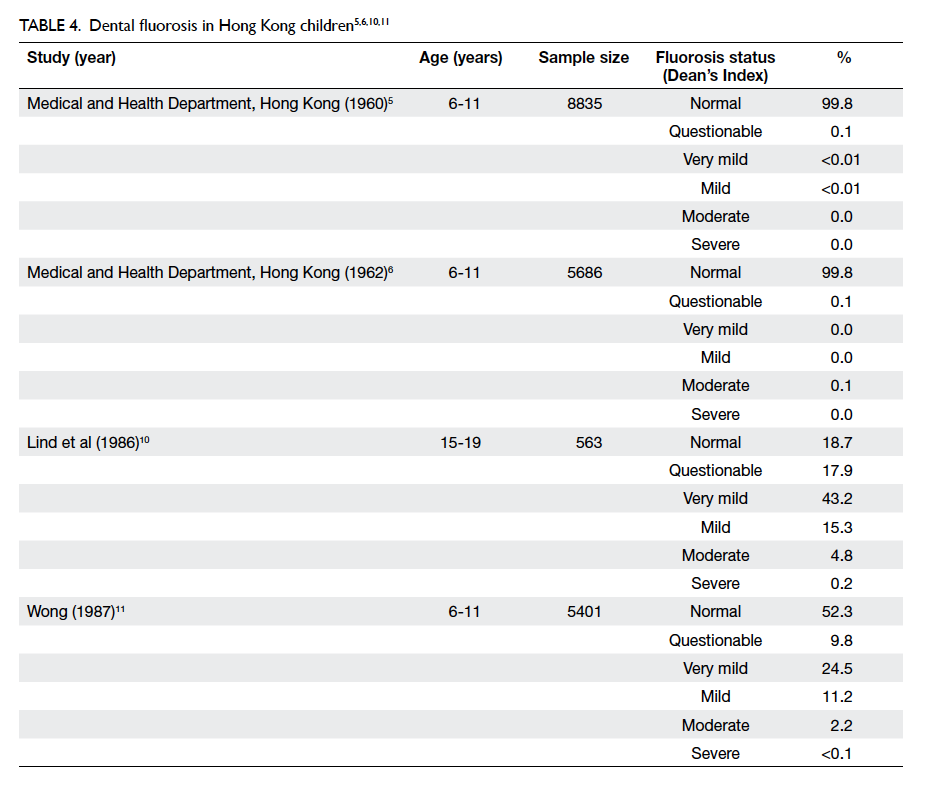
Dental fluorosis/enamel defects
Dental fluorosis consequent to exposure to fluoride
may develop during the formation of teeth in young
children. Table 4 outlines the studies reporting dental fluorosis using Dean’s Index in Hong
Kong to date.5 6 10 11 Epidemiological studies reporting
dental fluorosis showed that the level was low in the
1960s.5 6 Nearly all examined children aged 6 to 11 years
had ‘normal’ enamel. Less than 1% were assessed as
having a ‘mild’ or ‘questionable’ degree of fluorosis in
1960 or having a ‘moderate’ or ‘questionable’ degree
of fluorosis in 1962.
Dental fluorosis was reported to be more
prevalent in the 1980s, particularly among
adolescents.10 11 Over 80% of the 15-19-year-olds in the study by Lind et al10 exhibited signs of dental
fluorosis; and approximately 50% of the 6-11-year-olds in the study by Wong11 showed various degrees of dental fluorosis.
King24 reported the prevalence of enamel
defects among a random sample of 12-year-old
children in Hong Kong. The prevalence of teeth
with opacities was 99.6%; 82.8% had evidence of
hypoplasia and 16.6% had discoloured teeth. The
author believed that many of the enamel defects were
likely to be related to dental fluorosis. The findings in
the 1980s suggested a marked increase in the level
of dental fluorosis since the introduction of water
fluoridation in the 1960s and it was then advocated
to lower the water fluoridated level.1 The prevalence
declined considerably over the decades when the
level of fluoride in the water supply was adjusted and
lowered.25 At present the level of water fluoridation
is optimal at 0.5 ppm. The trend of decreasing dental
fluorosis prevalence was evident in the study by
Evans and Stamm.26 The prevalence decreased from
64% to 47% across the cohort of children from older
(aged 12) to younger (aged 7) born before and after
reduction of fluoride level to 0.7 ppm in 1978.
The prevalence and severity of developmental
defects of enamel (DDE) have also been studied.
Cross-sectional surveys showed that the prevalence
of diffuse opacities among random samples of
12-year-old children (based on maxillary incisors and
assessed using standardised intra-oral photographs)
declined from 89.3% in 1983 to 32.4% in 2001, but
increased to 42.1% in 2010.27 The mouth prevalence
of DDE among maxillary incisor teeth of the
children also decreased from 92.1% in 1983 to 35.2%
in 2001.28 Wong et al29 also reported the prevalence
of DDE among Hong Kong 12-year-old children
at 90% in a 2010 cohort study (89.5% had diffuse
opacities, 8.6% demarcated opacities, and 1.8%
hypoplasia), using the modified version of the DDE
index by FDI (Fédération Dentaire Internationale)
to diagnose DDE.30 The prevalence of molar incisor
hypomineralisation was reported as 2.8% among
Primary 6 Chinese schoolchildren in a 2006
retrospective study.31
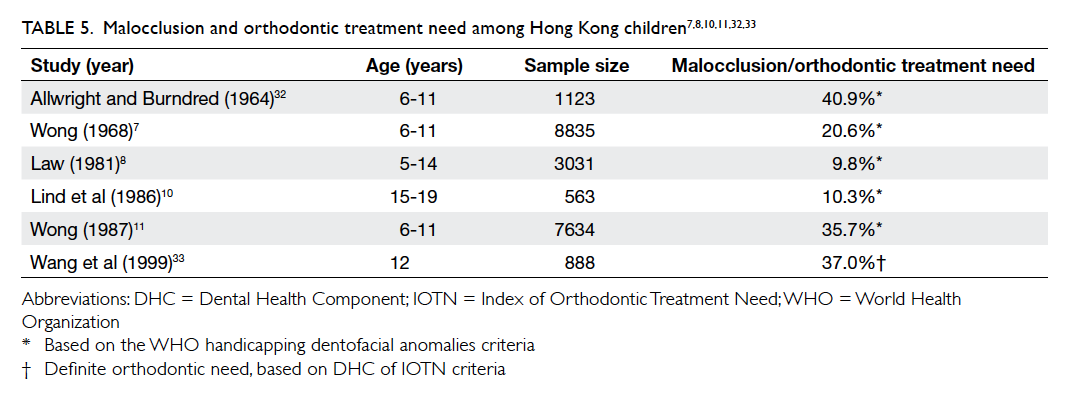
Malocclusion and orthodontic treatment need
Epidemiological data on malocclusion and
orthodontic treatment need among Hong Kong
children are scant. Relatively few surveys have
been conducted since the 1960s but details of the
available studies are shown in Table 5.7 8 10 11 32 33 The studies were heterogeneous in terms of criteria
used to assess dentofacial anomalies that require
orthodontic intervention and age of the sampled
children. Comparison and description of estimates
of orthodontic treatment are difficult.
Earlier epidemiological studies of malocclusion
and orthodontic treatment need among Hong Kong
children suggested that dentofacial deformities
requiring treatment intervention was ≤20%. More
recent studies suggest orthodontic treatment need to
be closer to 40%. It is estimated that about one third
of children have a ‘definite’ orthodontic treatment
need. A report by Allwright and Burndred32
provided the first published study of the prevalence
of dentofacial anomalies requiring treatment
intervention among Hong Kong children. Their
study included 31% of the 6-11-year-old children
who participated in the 1962 oral health survey6
and reported that 40.9% of the children exhibited
certain dentofacial anomalies. The most common
malocclusions were crowding (20.3%), maxillary
overjet (14.5%), mandibular overjet (8.1%), overbite
(6.9%), spacing (2.9%), and open bite (1.1%). The
prevalence of handicapping dentofacial anomalies
was higher among those aged 9 to 11 years (54.2%)
than among those aged 6 to 8 years (36.4%).
Wong7 reported that approximately one (20.6%)
in five of 5-14-year-old children had dentofacial
anomalies that required dental treatment. The most
common dentofacial anomaly was crowding (17.6%),
followed by maxillary overjet (9.5%), overbite (4.2%),
mandibular overjet (2.7%), spacing (1.1%), and
open bite (0.7%). The prevalence of anomalies was
higher among those aged 9 to 15 years (28.2%) than
among those aged 5 to 8 years (16.4%). The reduction
in the prevalence estimates of malocclusion when
compared with the 1960 study6 could be due to the
participation of different examiners (orthodontists
in 1960 study vs general dental practitioners in 1968
study) and the wider age range of children involved
in the 1968 survey.7
In the 1980s, the reported prevalence of dentofacial
anomalies that required treatment was 10%
to 36%.8 10 11 The percentage of children with cleft
palates and/or lip was approximately 0.2%, with a
slightly higher proportion of children with cleft lip.8 11 The most common reported dentofacial anomalies
that required treatment were crowding (3.3-18.5%),
maxillary overjet (2.8-5.1%), cross-bite (2.4-7.5%),
reverse overjet anomaly (1%), deep overbite (0.9-5.4%), and open bite (0.5-1.9%). The prevalence
of dentofacial anomalies was higher among 9-11-year-old children (13-38%) compared with 6-8-year-old children (6.7-34%).8 11 Among all the reported studies, only Wang et al33 used DHC IOTN (Dental
Health Component of the Index of Orthodontic
Treatment Need)34 to assess treatment
need. The prevalence of malocclusion was estimated
to be 88% and over a third (37%) of the study
sample were deemed to have a ‘definite’ orthodontic
treatment need and 33% had a moderate need.
Discussion
The introduction of water fluoridation in the 1960s
resulted in improvements in dental caries in Hong
Kong. Prior to its implementation, nearly all children
in the population had dental caries, with a high mean
number of decayed, missing, or filled teeth because
of tooth decay (mean dmft of 9.2 and DMFT of
4.4).5 The implementation of water fluoridation in
the community led to a gradual decline in the caries
experience and severity in children, as confirmed by
the first three oral epidemiological studies in Hong
Kong.5 6 7 The caries experience remained constant (plateaued) with approximately 50% of preschool children
and 20% to 40% of schoolchildren since 1980s/1990s
having a dental caries experience. This indicates
that children in Hong Kong are benefiting from the
continual effects of water fluoridation as well as
exposure to fluoride from other sources, together
with changing living conditions, lifestyles, and
improved oral self-care habits in recent decades. The
stable caries prevalence in recent years signifies that
dental caries in children is controlled to a certain
degree, but still remains prevalent, however.
Despite great improvements in the oral health
of Hong Kong children over the past 50 years,
dental caries remains an oral health burden in the
community, in particular among preschool children
where prevalence and incidence remain high.
Although caries prevalence and severity among preschool children
declined during the first 30 years
following water fluoridation, the prevalence remains
similar and its extent/severity has been even higher
in recent decades.16 17 19 20 This suggests that there
remain some preschool children for whom the
current measures alone (water fluoridation and oral
health education) are insufficient to ensure optimal
oral health.
The dental caries prevalence and severity in
preschool children tended to rise with increasing
age.4 19 20 From the epidemiological studies, it is
thus common to find a higher percentage of caries
experience in children at the upper end of the preschool
age range. Moreover, caries experience
is not uniformly distributed within populations
of children. Children from disadvantaged and
socially marginalised populations had a higher
caries experience and severity.4 18 19 20 Preventive
measures and oral health education should start
earlier among younger children and their parents or
caregivers. In particular, efforts should focus on the
underprivileged population in our community.
The dental caries condition among Hong Kong
schoolchildren (12 years old) is relatively good by
international comparisons. Dental caries affects
60% to 90% of schoolchildren in most industrialised
countries.35 36 The current dental caries experience
in 12-year-old Hong Kong children is relatively very
low.16 17 Of note, most of the dental caries experience
was related to filled teeth, few (approximately 1
in 20) had untreated decay. This pattern can be
largely attributed to the contribution of the SDCS,
which began in the 1980s as a school-based dental
care system that effectively overcomes many social
barriers to dental care access by schoolchildren (eg
family income, education, dental health awareness).
Schoolchildren receive regular quality dental care and
treatment through the SDCS. The observed low level
of untreated dental caries among schoolchildren is in
stark contrast to findings prior to the introduction of
SDCS when most decay remained untreated or was
treated by extraction.5 6 7 8 The SDCS has also raised
awareness of oral health among schoolchildren.
Education about the importance of oral health has
likely changed children’s lifestyle and improved their
self-care practice and use of fluoride oral health care
products.
Dental attendance among primary
schoolchildren is high because of high participation
in the SDCS,37 but remains worryingly low among
secondary school and preschool children. Many
adolescents and their parents do not consider
there to be a need for such care. Less than a third
of such children reported regular attendance for
dental check-ups, presumably because this group of
children have to be seen privately to access dental
care.10 13 16 17 18 19 20 Early and regular dental check-ups to
enable preventive care should be advocated.
Conclusions
The introduction of a number of public health
measures in Hong Kong, mainly water fluoridation
and the SDCS, has improved the oral health of Hong
Kong children over the past 50 years. There has been
a decline in dental caries among schoolchildren
and adolescents. Nonetheless, the dental caries
experience has remained unchanged in recent
decades for preschool children; even a slight increase
in extent/severity has been observed. Although there
is evidence of improvement, the overall periodontal
health of Hong Kong children remains unsatisfactory.
A decrease in the prevalence and severity of enamel
defects among Hong Kong children was observed,
but there has recently been a slight increase. In view
of the limited data regarding malocclusion in Hong
Kong children, epidemiological studies should be
considered. The utilisation of dental services is low,
especially among preschool children who are not
covered by the SDCS. New policies to develop dental
care protocols to ensure evidence-based standards
of care, and to advocate regular access to dental care
and preventive services may further improve the oral
health of Hong Kong children.
References
1. Evans RW, Lo EC, Lind OP. Changes in dental health in
Hong Kong after 25 years of water fluoridation. Community
Dent Health 1987;4:383-94.
2. Chiu GK, Davies WI. The historical development of
dentistry in Hong Kong. Hong Kong Med J 1998;4:73-6.
3. Hong Kong Department of Health. Health Statistics.
Surveillance & Epidemiology Branch, Centre for Health
Protection. Health facts of Hong Kong. Available from:
http://www.dh.gov.hk/english/statistics/statistics_hs/files/Health_Statistics_pamphlet_E.pdf. Accessed Oct 2014.
4. Chu CH, Fung DS, Lo EC. Dental caries status of preschool
children in Hong Kong. Br Dent J 1999;187:616-20. Crossref
5. Medical and Health Department. Report on the 1st (pre-fluoridation) dental survey of school children in Hong
Kong. Medical and Health Department, Hong Kong; 1960.
6. Medical and Health Department. Report on the 2nd (post-fluoridation) dental survey of school children in Hong
Kong. Medical and Health Department, Hong Kong; 1962.
7. Wong KK. Report of a dental survey in Hong Kong 1968.
The Government Dental Service, Hong Kong and the
World Health Organization; 1968.
8. Law YH. Dental health status of primary school children
in Hong Kong. The Bulletin. Hong Kong Soc Community
Med 1981;12:1-16.
9. King NM, Ling JY, Ng BV, Wei SH. The dental caries status
and dental treatment patterns of 12-year-old children in
Hong Kong. J Dent Res 1986;65:1371-4. Crossref
10. Lind OP, Evans RW, Holmgren CJ, Corbet EF, Lim LP,
Davies WI. Hong Kong Survey of Adult Oral Health 1984.
Hong Kong: Department of Periodontology and Public Health,
Faculty of Dentistry, University of Hong Kong; 1986.
11. Wong PY. A report on a dental survey of primary school
children in Hong Kong. Medical and Health Department,
Hong Kong; 1987.
12. Lo EC, Evans RW, Lind OP. Dental caries status and
treatment needs of the permanent dentition of 6-12-year-olds
in Hong Kong. Community Dent Oral Epidemiol
1990;18:9-11. Crossref
13. Kwan EL. Oral health status of 13 and 15 year-old secondary school children in Hong Kong [dissertation]. Hong Kong: University of Hong Kong; 1992.
14. Yiu C, Wong MC, Chan M, et al. Oral health of 15-year-old
secondary school students in H.K. Hong Kong: Faculty of
Dentistry, University of Hong Kong; 2001.
15. Evans RW, Lo EC. Effects of School Dental Care Service
in Hong Kong—primary teeth. Community Dent Oral
Epidemiol 1992;20:193-5. Crossref
16. Hong Kong Department of Health. Oral health survey
2001: common dental diseases and oral health related
behaviour. Hong Kong SAR: Dental Services Head Office,
Department of Health; 2002.
17. Hong Kong Department of Health. Oral health survey
2011: common dental diseases and oral health related
behaviour. Hong Kong SAR: Dental Services Head Office,
Department of Health; 2012.
18. Wei SH, Holm AK, Tong LS, Yuen SW. Dental caries
prevalence and related factors in 5-year-old children in
Hong Kong. Pediatr Dent 1993;15:116-9.
19. Lo EC, Loo EK, Lee CK. Dental health status of Hong Kong
preschool children. Hong Kong Dent J 2009;6:6-12.
20. Chu CH, Ho PL, Lo EC. Oral health status and behaviours
of preschool children in Hong Kong. BMC Public Health
2012;12:767. Crossref
21. Ainamo J, Barmes D, Beagrie G, Cutress T, Martin J, Sardo-Infirri J. Development of the World Health Organization
(WHO) community periodontal index of treatment needs
(CPITN). Int Dent J 1982;32:281-91.
22. Wu D. Provision of outreach dental service and caries
risk assessment to preschool children in Hong Kong
[dissertation]. Hong Kong: University of Hong Kong; 2011.
23. Ainamo J, Bay I. Problems and proposals for recording
gingivitis and plaque. Int Dent J 1975;25:229-35.
24. King NM. Developmental defects of enamel in Chinese
girls and boys in Hong Kong. Adv Dent Res 1989;3:120-5.
25. Evans RW. Changes in dental fluorosis following an
adjustment to the fluoride concentration of Hong Kong’s
water supplies. Adv Dent Res 1989;3:154-60.
26. Evans RW, Stamm JW. Dental fluorosis following downward
adjustment of fluoride in drinking water. J Public Health
Dent 1991;51:91-8. Crossref
27. Wong HM, McGrath C, King NM. Diffuse opacities in
12-year-old Hong Kong children—four cross-sectional
surveys. Community Dent Oral Epidemiol 2014;42:61-9. Crossref
28. Wong HM, McGrath C, Lo EC, King NM. Association
between developmental defects of enamel and different
concentrations of fluoride in the public water supply.
Caries Res 2006;40:481-6. Crossref
29. Wong HM, Peng SM, Wen YF, King NM, McGrath CP. Risk
factors of developmental defects of enamel—a prospective
cohort study. PLoS One 2014;9:e109351. Crossref
30. A review of the developmental defects of enamel index
(DDE Index). Commission on Oral Health, Research &
Epidemiology. Report of an FDI Working Group. Int Dent
J 1992;42:411-26.
31. Cho SY, Ki Y, Chu V. Molar incisor hypomineralization
in Hong Kong Chinese children. Int J Paediatr Dent
2008;18:348-52. Crossref
32. Allwright WC, Burndred WH. A survey of handicapping
dentofacial anomalies among Chinese in Hong Kong. Int
Dent J 1964;14:505-19.
33. Wang G, Hägg U, Ling J. The orthodontic treatment need
and demand of Hong Kong Chinese children. Chin J Dent
Res 1999;2:84-92.
34. Brook PH, Shaw WC. The development of an index of
orthodontic treatment priority. Eur J Orthod 1989;11:309-20.
35. Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S,
Ndiaye C. The global burden of oral diseases and risks to
oral health. Bull World Health Organ 2005;83:661-9.
36. Dye BA, Tan S, Smith V, et al. Trends in oral health status:
United States, 1988-1994 and 1999-2004. Vital Health Stat
11 2007;(248):1-92.
37. King NM. Paediatric dentistry in Hong Kong. Int J Paediatr
Dent 1998;8:1-2. Crossref