DOI: 10.12809/hkmj154763
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
MEDICAL PRACTICE
Guidelines for allergy prevention in Hong Kong
Alson WM Chan, FHKCPaed, FHKAM (Paediatrics)1;
June KC Chan, RD (USA), MSc2;
Alfred YC Tam, FHKCPaed, FHKAM (Paediatrics)1;
TF Leung, MD, FHKAM (Paediatrics)3;
TH Lee, ScD (Cantab), FRCP (Lond)2
1 Department of Paediatrics and Adolescent Medicine, The University of Hong Kong, Pokfulam, Hong Kong
2 Allergy Centre, Hong Kong Sanatorium & Hospital, Happy Valley, Hong Kong
3 Department of Paediatrics, The Chinese University of Hong Kong, Shatin, Hong Kong
This guideline was presented in part at the Symposium on Allergy
Prevention that was co-hosted by the Hong Kong Institute of Allergy &
the Hong Kong Society for Paediatric Immunology, Allergy and Infectious
Diseases, 17 September 2015, Hong Kong.
Corresponding author: Dr Alson WM Chan (awmc@hku.hk)
Abstract
Allergic diseases are a global problem. Mothers are
advised to enjoy a healthy diet with no restrictions
during pregnancy and lactation, as prophylactic
dietary restriction is unlikely to reduce the
development of atopic disease. Breastfeeding is
recommended for the first 6 months of the newborn’s
life. Atopic eczema has been shown to be significantly
reduced in high-risk infants fed a hydrolysed formula
compared with standard cow’s milk formula.
Complementary food is also recommended for
infants over 4 months if they are developmentally
ready. Various environmental factors may influence
the prevalence and course of allergic diseases. There
is a strong epidemiological association between
air pollution from traffic and allergies. Smoking is
also a significant risk factor. Home dampness and
visible mold are associated with recurrent wheeze
and asthma. House dust mite is a possible cause of
asthma. Lifestyle factors also play a role. Obesity
shows a clear relationship with asthma and eczema.
Stressful life events may increase the risk of atopic
disease. Immunotherapy has been shown to be
effective. It reduces new sensitisations and prevents
progression of allergic rhinitis to asthma. Summary
of the above recommendations are presented.
Introduction
There has been a continuous rise over the last 50
years in the prevalence of allergic diseases in both
developed and developing countries. The situation
is especially dramatic in children. Up to 40% to 50%
of schoolchildren are now sensitised to one or more
common allergens. The growing burden of allergic
diseases has been recognised as a new pandemic of
the 21st century.1
It has long been acknowledged that genetically
predisposed children usually develop various
allergic diseases in the typical evolution described
as ‘Allergic March’. Cow’s milk and food are the
first allergens that infants encounter soon after
birth. Their allergies then progress from the gut and
skin to the respiratory tract when they grow older
and come into contact with more environmental
allergens. Prevention strategies applied during
infancy or early childhood have been shown to stop
the manifestations of allergy and its ‘marching’ from
gut to skin and to airway.2
Recent studies have shown that induction of
immune tolerance is the key to success in allergy
prevention. Early food allergen introduction between
4 and 6 months leads to better immune tolerance.3
New evidence is also showing the association of
allergy with various environmental and lifestyle
factors that might be amenable to manipulation.
As the burden of allergic diseases has been
increasing and the concept of allergy has been
changing quickly over the last few years, there is
a need to develop updated guidelines for allergy
prevention.
Epidemiology of allergic diseases in Hong Kong children
Allergic diseases constitute a major health problem
worldwide, with asthma as one of the most common
chronic diseases of childhood. The population-based
International Study of Asthma and Allergies
in Childhood (ISAAC) determined that about one
tenth of secondary schoolchildren have asthma
and 15% have atopic dermatitis. About one third of
Hong Kong children aged 6 to 7 years suffer from
rhinitis.4 The phase-2 ISAAC confirmed aeroallergen
sensitisation as a major risk factor for childhood
allergies,5 but this relationship varied substantially
among populations and increased with economic
development.
There are limited data on the prevalence
and risk factors for atopic disorders among Asian
preschool children. Using an ISAAC-based
questionnaire, we reported the prevalence of ‘ever’
and ‘current’ wheeze among Hong Kong children
aged 2 to 6 years to be 16.7% and 9.3%, respectively.6
Consistent with our earlier report for older Chinese
children,7 the use of foam pillow and gas as the
cooking fuel in infancy were significant risk factors
for current wheeze in these young children.
The incidence rates of asthma and allergies
have been increasing in many developed countries.
Our phase-3 ISAAC nonetheless found a reduced
asthma prevalence over an 8-year period among
Hong Kong secondary schoolchildren.8 The
prevalence of asthma ever, wheeze ever, and current
wheeze was also similar in local children aged 6 to 7
years between 1995 and 2001, although there was a
significant increase in lifetime and current rhinitis,
current rhinoconjunctivitis, and lifetime eczema
during this period.9
A territory-wide questionnaire study
investigated the prevalence of adverse food reactions
(AFR) among local children attending 21 randomly
selected nurseries and kindergartens in 2004/2005.10
The prevalence rates of parent-reported AFR and parent-reported, doctor-diagnosed AFR were 8.1%
and 4.6%, respectively. The occurrence of AFR in
these pre-schoolers adversely affected their parents’
quality of life.11 Shellfish was the most important
food for AFR, followed by egg, peanut, cow’s
milk, beef, tree nuts, and fish. Another local study
supported these findings.12 These figures suggested
similar epidemiology and spectrum of food allergy
between our Chinese and Caucasian children.
Because questionnaire data may be subject to biased
reporting, we also collected data for probable food
allergy that was defined by the presence of suggestive
clinical features and either positive skin prick test
or in-vitro allergen-specific immunoglobulin (Ig) E
assays.13 The prevalence of probable food allergy was
2.8% in our primary schoolchildren.14
In another more recent study, our group
adopted the same sampling strategy and
methodology to investigate longitudinal changes in
food allergy prevalence among Chinese preschool
children.15 The prevalence of parent-reported
AFR was 9.7%, but there was no change in parent-reported,
doctor-diagnosed AFR. When adjusted for
maternal education as a covariate, the prevalence
of parent-reported AFR was static whereas that of
parent-reported, doctor-diagnosed AFR significantly
decreased during this 9-year period.15
Maternal diet during pregnancy
It is universally recommended for all mothers to eat
a healthy diet without restriction during pregnancy.
Prophylactic dietary restriction of potent food
allergens should not be encouraged.16
During the first trimester, higher maternal
intake of peanut, milk, and wheat is associated with
a significant reduction in the risk of developing
a peanut allergic reaction, asthma and allergic
rhinitis, and atopic dermatitis in mid-childhood,
respectively.17 In addition, a restrictive diet may have
adverse effects on maternal or fetal nutrition.
Maternal consumption of fruits and
vegetables, fish, long-chain omega-3 fatty acids, a
good ratio of omega-3–to–omega-6 fatty acids, and
milk fat during pregnancy is associated with a lower
prevalence of allergy. The consumption of fruits
and vegetables is beneficial for their antioxidants
and natural prebiotics that may have prophylactic
properties by promoting a more diverse microbiota
and consequently a positive effect on fetal immune
development.18 The consumption of fish during
pregnancy has a protective effect against the
development of atopic diseases in children. The
current German guidelines recommend that fish
consumption is encouraged in pregnancy.19
Maternal diet during lactation
Studies that examined the effect of food avoidance
during lactation have been criticised for
methodological shortcomings and small sample
size, and more research is required in this area.
Currently, there is no evidence to support maternal
dietary avoidance of potent food allergens while
breastfeeding as a means of preventing development
of food allergy in their children.16
Breastfeeding
For all infants, breastfeeding is recommended for at
least the first 4 to 6 months of life.19 20 21 Breastfeeding
has many health benefits for both mothers and
infants, and the World Health Organization
recommends that infants should be exclusively
breastfed for the first 6 months of life. Evidence
suggests that exclusive breastfeeding for at least
3 months reduces the risk of atopic dermatitis in
infancy although data are weaker for other allergic
diseases.22 When compared with conventional cow’s
milk formula, breast milk has a significant protective
effect against atopic dermatitis and wheezing in
the first 2 years of life and might play a role in the
development of oral tolerance.23
Formula feeding
The GINI (German Infant Nutritional Intervention)
study’s 15-year data show that in high-risk infants,
compared with standard cow’s milk formula, the
consumption of extensively hydrolysed casein
formula is associated with a reduced cumulative
incidence of eczema and allergic rhinitis, as well
as a reduced prevalence of eczema and asthma
in adolescence. The consumption of partially
hydrolysed whey formula is associated with a reduced
cumulative incidence of eczema and prevalence of
allergic rhinitis in adolescence. On the contrary,
there is no significant benefit for consumption of
extensively hydrolysed whey formula, indicating the
degree of hydrolysis alone does not fully explain the
preventive power of a formula and further research
will be needed in this area.24 There is no evidence
for the use of soy formula or goat formula in the
prevention of food allergies and amino acid formula
has not been well studied.
Introduction of complementary foods
Introduction of complementary foods is
recommended for infants aged over 4 months. There
is no benefit in delaying introduction beyond 4 to
6 months in order to prevent allergic diseases.25
An infant diet consisting of high levels of fruits,
vegetables, and home-prepared foods is associated
with less food allergy by the age of 2 years.26 When
introducing complementary foods, consideration of
developmental readiness, parental needs, nutritional
needs, and behavioural risks of the infant should be
made.
Introduction of potential food allergens
There is emerging evidence that delaying solid food
introduction beyond 6 months, especially those
containing potent food allergens, may increase the
risk of food allergy or eczema.23 Data from a Finnish
cohort study indicate that late introduction of
potatoes, oats, rye, wheat, meat, fish, and eggs was
significantly and directly associated with sensitisation
to food allergens,27 while late introduction of
potatoes, rye, meat, and fish was associated with
inhalant allergen sensitisation. Recently, the LEAP
(Learning Early About Peanut allergy) study has
demonstrated that consumption of peanuts within
the first year of life in high-risk infants can lower the
chance of peanut allergy compared with avoidance
until the age of 5 years.28 Another randomised
controlled trial found that infants exposed to whole
egg powder daily starting at 4 to 8 months had higher
egg-specific IgG4 levels compared with a control
group.29 Furthermore, introduction of fish before
9 months of age is associated with a lower risk of
eczema and is recommended by one of the national
guidelines.19
At present, there is insufficient evidence to
recommend early introduction of all potential food
allergens. The current recommendation is neither
to withhold nor encourage early introduction of any
food allergens.19 20 21 Breastfeeding during the period
of solid food introduction is likely to attenuate any
allergic response.33
Environmental influence on allergy
Air pollution
It has long been recognised that atmospheric air
pollution is associated with exacerbation of asthma
and allergic rhinitis, and is blamed for surges in
hospital admissions for asthma. In the past decade,
much epidemiological evidence has linked exposure
to air pollution from traffic, especially diesel
exhaust particulates, oxides of nitrogen, and soot
(carbon dust) to the development of asthma, allergic
sensitisation, and compromised lung function.30
Another report investigated the relationship between
traffic-associated pollution and eczema in children
aged 6 years. Eczema prevalence was significantly
higher in children who lived in traffic-related, highly
polluted areas.31
Mechanisms implicated in the association
between air pollution and paediatric asthma include
the up-regulation of allergic immune responses,
activation of oxidative stress pathways, and
epigenetic regulation.
Tobacco smoke
The effect of both active smoking (AS) and passive
smoking (PS) on the development of allergic diseases
in adults and children has been recently reviewed.32
When all studies including cohort, case-control, and
cross-sectional studies were included, allergic rhinitis
was not associated with AS, but was associated with
PS. Allergic dermatitis was associated with both AS
and PS. In children and adolescents in particular,
allergic rhinitis was associated with both AS and PS,
as was allergic dermatitis. Among cohort studies,
PS was significantly associated with an increased
risk of food allergy in children and adolescents.
From these studies, it can be seen that the effect
of tobacco smoke is more severe in children and
adolescents compared with adults. In countries with
high smoking prevalence, the authors estimated
that 14% of allergic rhinitis cases and 13% of allergic
dermatitis are attributable to AS.33
The European Community Respiratory Health
Survey has reported the effects of PS from fetus to
adulthood.33 34 Maternal smoking during pregnancy,
maternal smoking, or both parents smoking was
more likely to be associated with asthma symptoms
in offspring, even after accounting for smoking
behaviour, exposure to PS, and occupational
exposure.32 Total IgE levels were higher in smokers
than non-smokers. The smokers were more likely
to be sensitive to house dust mite (HDM) but not
to cat dander or grass pollen. On the other hand,
PS was significantly associated with bronchial
responsiveness to methacholine and with current
asthma.
Indoor environment
The meta-analysis from eight European birth
cohorts showed that exposure to visible mold and/or dampness during the first 2 years of life was
associated with an increased risk of developing
asthma, including early asthma symptoms and
asthma later in childhood.35 In another study, high
visible mold in the home environment was also
associated with recurrent wheeze at the age of 3
years and a positive Asthma Predictive Index.36
Other risk factors at home that have been reported
to be associated with recurrent wheezing include use
of foam pillow and exposure to gas cooking fuel.6
Another recent review and meta-analysis
reported an overall 25% reduction in doctor-diagnosed
asthma and recurrent wheeze in children
exposed to a farming environment.37 The mechanism
of effect of farm exposure on allergy development
has been thought to be related to raw farm milk
consumption and/or exposure to a wider range of
micro-organisms in the farm, and its resultant gut
microbiome.
Allergen exposure, especially to HDM allergen,
has been implicated as a possible cause of allergic
asthma. Many studies have attempted to prevent
allergies and asthma by controlling HDM and
other allergens in the home environment. A recent
meta-analysis38 reported a significant reduction
in physician-diagnosed asthma as a result of
interventions to reduce exposure to HDM (relative
risk [RR]=0.74; 95% confidence interval [CI], 0.58-0.95). There was, however, no significant effect on
parent-reported wheeze (RR=0.95; 95% CI, 0.78-1.15). This may suggest that reduced exposure to
HDM prevents the more severe form of asthma but
not the more common and milder forms that may
not be allergic in origin. A pooled analysis of over
22 000 children participating in 11 European birth
cohorts concluded that there was neither an increase
nor reduction in the risk of asthma or allergic rhinitis
in children in relation to pet ownership in early life.39
The situation with other allergens is not clear.
In conclusion, dampness, visible mold,
and HDM are important indoor factors in the
development of allergic disease. The control of
these factors is likely to lead to a lesser chance of
development of allergic disease including asthma.
Although a farming environment is known to
be associated with a lower incidence of allergy,
recommendation is still difficult and awaits further
analysis of the mechanism of action.
Viral respiratory infections
Early viral respiratory infections have been
implicated in the development of asthma and other
respiratory allergies later in life. Human rhinovirus
and respiratory syncytial virus have been found to be
associated with a markedly higher risk of persistent
wheezing at 6 years of age.40 Another study of over
2000 children confirmed an increased risk of new-onset
wheeze at the age of 2 years in those suffering
from childhood infections like common cold, fever,
and diarrhoea during the first 3 months of life.41
Preventive strategies, apart from general infection
control measures, consist of giving respiratory
syncytial virus Ig to vulnerable infants.42
Lifestyle
Overweight and obesity
A healthy lifestyle with a balanced calorie intake
and expenditure should be encouraged. A recent
meta-analysis has revealed that being overweight
poses an increased risk of asthma. This risk is
further elevated in obese subjects with a clear dose-response
relationship between body mass index and
risk of asthma.43 European birth cohorts recruiting
more than 12 000 subjects have demonstrated that
a rapid rise of body mass index in the first 2 years
of life increased the risk of asthma up to 6 years old
(hazard ratio=1.3; 95% CI, 1.1-1.5).44 There is also a
significant association between overweight/obesity
and eczema.45 Excessive body weight should be
avoided to help prevent the development of allergic
diseases.
Psychosocial factors
A growing number of studies indicate that experiencing
stressful life events (eg parental separation,
death of a parent, parental unemployment), either
during pregnancy or in early childhood, increases
the risk of subsequent atopic diseases.46 Early
therapeutic counselling may represent a preventive
approach in these children.
Pharmaceuticals
A population-based study of over 16 000 Finnish
patients revealed an increased risk of cow’s milk
allergy associated with maternal/child use of
antibiotics in a dose-related manner.47 Further
studies are needed to confirm this observation
in other populations. At present, no causal
relationship has been established between the use
of pharmaceuticals and the development of atopic
disease.
Probiotics
Probiotics have been shown in some studies to
prevent the development of eczema.48 Nonetheless,
more studies are required to confirm their efficacy
and most allergy guidelines do not make any
recommendations about probiotics.
Vaccinations
There is no evidence to show that vaccination
practices have any adverse effect on the incidence
of allergic diseases in population-based cohort
studies.49 It is advised that children are vaccinated
according to the current recommended schedule,
including high-risk children.
Vitamin D
Clinical studies have produced conflicting results
with regard to the relevance of vitamin D in the
development of allergic diseases. There are currently
insufficient data to support any recommendation.
Immunotherapy
Immunotherapy, both subcutaneous and sublingual,
is an important tool in the secondary prevention
of allergic diseases. There is evidence that
immunotherapy of allergic rhinitis can prevent
the subsequent progression to asthma.50 It can
also reduce new sensitisations in patients monosensitised
to aeroallergens and has an impact on the
natural history of respiratory allergies.51
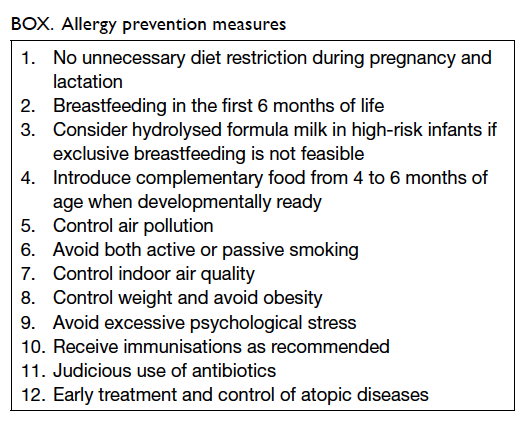
Conclusions
The strengthening of immune tolerance is the
current focus of allergy prevention. In addition
to allergen avoidance, further studies are now
underway to investigate how immune tolerance to
different allergens can be boosted, while minimising
sensitisation and further allergic responses. In
general, the greater the exposure to environmental
and commensal microbes in terms of diversity and
quantity during infancy and early childhood, the
greater the development of immune tolerance and
less atopic tendency later on, even in those who are
genetically susceptible.52 The allergy prevention
measures we recommend are summarised in the
Box. For those who are at higher risk of allergy development, that is those with a family history
of allergy or the presence of several risk factors
(eg breastfeeding for <6 months; maternal AS or PS
during pregnancy; delivered by caesarean section),
it is recommended that they observe the allergy prevention
measures and consult a medical doctor
early should they develop clinical features of allergic
diseases. Besides recommendations on a personal
level, the development of a community-based action
plan would be beneficial and cost-effective. The
implementation of National Allergy Programme, a
new programme designed after the success of the
previous Finnish Asthma Programme in 2000 to
2010, has already shown that the burden and cost
of allergic diseases can be reduced by a pragmatic
public health action plan.53 A successful community-based
programme requires contributions from
various stakeholders for effective implementation.
Educational campaigns and networking between
specialists and primary care doctors, pharmacists,
nurses, teachers, parents, allergic patients, and the
general public should be promoted. The treatment
modalities for allergy are relatively limited at present,
so prevention is the key to control this pandemic.
Allergic diseases in Hong Kong and worldwide have
increased dramatically in the past few decades. It
is now pressing and timely to implement allergy
prevention to promote a healthy lifestyle for the
Hong Kong population and beyond.54
Declaration
The authors have no conflicts of interest to declare.
References
1. Pawankar R, Canonica GW, Holgate ST, Lockey RF,
Blaiss MS. WAO White book on allergy: update 2013.
World Allergy Organization. Available from: http://www.worldallergy.org/UserFiles/file/WhiteBook2-2013-v8.pdf.
Accessed Apr 2016.
2. Zheng T, Yu J, Oh MH, Zhu Z. The atopic march:
progression from atopic dermatitis to allergic rhinitis and
asthma. Allergy Asthma Immunol Res 2011;3:67-73. Crossref
3. Grimshaw KE, Maskell J, Oliver EM, et al. Introduction of
complementary foods and the relationship to food allergy.
Pediatrics 2013;132:e1529-38.
4. Wong GW, Hui DS, Chan HH, et al. Prevalence of
respiratory and atopic disorders in Chinese schoolchildren.
Clin Exp Allergy 2001;31:1225-31. Crossref
5. Wong GW, Leung TF, Ko FW. Changing prevalence of
allergic diseases in the Asia-pacific region. Allergy Asthma
Immunol Res 2013;5:251-7. Crossref
6. Wong GW, Leung TF, Ma Y, Liu EK, Yung E, Lai CK.
Symptoms of asthma and atopic disorders in preschool
children: prevalence and risk factors. Clin Exp Allergy
2007;37:174-9. Crossref
7. Wong GW, Ko FW, Hui DS, et al. Factors associated with
difference in prevalence of asthma in children from three
cities in China: multicentre epidemiological survey. BMJ
2004;329:486. Crossref
8. Wong GW, Leung TF, Ko FW, et al. Declining asthma
prevalence in Hong Kong Chinese schoolchildren. Clin
Exp Allergy 2004;34:1550-5. Crossref
9. Lee SL, Wong W, Lau YL. Increasing prevalence of allergic
rhinitis but not asthma among children in Hong Kong
from 1995 to 2001 (Phase 3 International Study of Asthma
and Allergies in Childhood). Pediatr Allergy Immunol
2004;15:72-8. Crossref
10. Leung TF, Yung E, Wong YS, Lam CW, Wong GW. Parent-reported
adverse food reactions in Hong Kong Chinese
pre-schoolers: epidemiology, clinical spectrum and risk
factors. Pediatr Allergy Immunol 2009;20:339-46. Crossref
11. Leung TF, Yung E, Wong YS, et al. Quality-of-life
assessment in Chinese families with food allergic children.
Clin Exp Allergy 2009;39:890-6. Crossref
12. Ho MH, Lee SL, Wong WH, Ip P, Lau YL. Prevalence of
self-reported food allergy in Hong Kong children and
teens—a population survey. Asian Pac J Allergy Immunol
2012;30:275-84.
13. Wong GW, Mahesh PA, Ogorodova L, et al. The
EuroPrevall-INCO surveys on the prevalence of food
allergies in children from China, India and Russia: the
study methodology. Allergy 2010;65:385-90. Crossref
14. Wong GW, Li J, Ma Y, et al. Comparative study of food
allergy in urban and rural schoolchildren: The Europrevall-INCO Survey in China. J Allergy Clin Immunol 2011;127(2
Suppl):AB34. Crossref
15. Leung TF, Sy HY, Tsan CS, Tang MF, Wong GW. Is food
allergy increasing in Hong Kong Chinese children?
[abstract]. Proceedings of the 34th Congress of European
Academy of Allergology and Clinical Immunology; 2015 Jun 6-10; Barcelona, Spain.
16. Kramer MS, Kakuma R. Maternal dietary antigen avoidance
during pregnancy or lactation, or both, for preventing
or treating atopic disease in the child. Evid Based Child
Health 2014;9:447-83. Crossref
17. Bunyavanich S, Rifas-Shiman SL, Platts-Mills TA, et
al. Peanut, milk, and wheat intake during pregnancy is
associated with reduced allergy and asthma in children. J
Allergy Clin Immunol 2014;133:1373-82. Crossref
18. Hörmannsperger G, Clavel T, Haller D. Gut matters:
microbe-host interactions in allergic diseases. J Allergy
Clin Immunol 2012;129:1452-9. Crossref
19. Schäfer T, Bauer CP, Beyer K, et al. S3-Guideline on allergy
prevention: 2014 update: Guideline of the German Society
for Allergology and Clinical Immunology (DGAKI) and the
German Society for Pediatric and Adolescent Medicine
(DGKJ). Allergo J Int 2014;23:186-99. Crossref
20. Muraro A, Halken S, Arshad SH, et al. EAACI food allergy
and anaphylaxis guidelines. Primary prevention of food
allergy. Allergy 2014;69:590-601. Crossref
21. Greer FR, Sicherer SH, Burks AW; American Academy of
Pediatrics Committee on Nutrition; American Academy
of Pediatrics Section on Allergy and Immunology. Effects
of early nutritional interventions on the development of
atopic disease in infants and children: the role of maternal
dietary restriction, breastfeeding, timing of introduction of
complementary foods, and hydrolyzed formulas. Pediatrics
2008;121:183-91. Crossref
22. Kramer MS. Breastfeeding and allergy: the evidence. Ann
Nutr Metab 2011;59 Suppl 1:20S-26S. Crossref
23. Lack G. Update on risk factors for food allergy. J Allergy
Clin Immunol 2012;129:1187-97. Crossref
24. von Berg A, Filipiak-Pittroff B, Schulz H, et al. Allergic
manifestation 15 years after early intervention with
hydrolyzed formulas—the GINI Study. Allergy
2016;71:210-9. Crossref
25. de Silva D, Geromi M, Halken S, et al. Primary prevention
of food allergy in children and adults: systematic review.
Allergy 2014;69:581-9. Crossref
26. Grimshaw KE, Maskell J, Oliver EM, et al. Diet and food
allergy development during infancy: birth cohort study
findings using prospective food diary data. J Allergy Clin
Immunol 2014;133:511-9. Crossref
27. Nwaru BI, Erkkola M, Ahonen S, et al. Age at the
introduction of solid foods during the first year and allergic
sensitization at age 5 years. Pediatrics 2010;125:50-9. Crossref
28. Du Toit G, Roberts G, Sayre PH, et al. Randomized trial of
peanut consumption in infants at risk for peanut allergy. N
Engl J Med 2015;372:803-13. Crossref
29. Palmer DJ, Metcalfe J, Makrides M, et al. Early regular egg
exposure in infants with eczema: A randomized controlled
trial. J Allergy Clin Immunol 2013;132:387-92.e1. Crossref
30. Nordling E, Berglind N, Melén E, et al. Traffic-related air
pollution and childhood respiratory symptoms, function
and allergies. Epidemiology 2008;19:401-8. Crossref
31. Krämer U, Sugiri D, Ranft U, et al. Eczema, respiratory
allergies, and traffic-related air pollution in birth cohorts
from small-town areas. J Dermatol Sci 2009;56:99-105. Crossref
32. Accordini S, Janson C, Svanes C, Jarvis D. The role of
smoking in allergy and asthma: lessons from the ECRHS.
Curr Allergy Asthma Rep 2012;12:185-91. Crossref
33. Burney PG, Luczynska C, Chinn S, Jarvis D. The European
Community Respiratory Health Survey. Eur Respir J
1994;7:954-60. Crossref
34. European Community Respiratory Health Survey
II Steering Committee. The European Community
Respiratory Health Survey II. Eur Respir J 2002;20:1071-9. Crossref
35. Tischer CG, Hohmann C, Thiering E, et al. Meta-analysis
of mould and dampness exposure on asthma and allergy
in eight European birth cohorts: an ENRIECO initiative.
Allergy 2011;66:1570-9. Crossref
36. Iossifova YY, Reponen T, Ryan PH, et al. Mold exposure
during infancy as a predictor of potential asthma
development. Ann Allergy Asthma Immunol 2009;102:131-7. Crossref
37. Genuneit J. Exposure to farming environments in
childhood and asthma and wheeze in rural populations:
a systematic review with meta-analysis. Pediatr Allergy
Immunol 2012;23:509-18. Crossref
38. Macdonald C, Sternberg A, Hunter PR. A systematic
review and meta-analysis of interventions used to reduce
exposure to house dust and their effect on the development
and severity of asthma. Environ Health Perspect
2007;115:1691-5. Crossref
39. Lødrup Carlsen KC, Roll S, Carlsen KH, et al. Does pet
ownership in infancy lead to asthma or allergy at school
age? Pooled analysis of individual participant data from 11
European birth cohorts. PLoS One 2012;7:e43214. Crossref
40. Jartti T, Korppi M. Rhinovirus-induced bronchiolitis
and asthma development. Pediatr Allergy Immunol
2011;22:350-5. Crossref
41. Mommers M, Thijs C, Stelma F, et al. Timing of infection
and development of wheeze, eczema, and atopic
sensitization during the first 2 yr of life: the KOALA Birth
Cohort Study. Pediatr Allergy Immunol 2010;21:983-9. Crossref
42. Meissner HC. Economic impact of viral respiratory disease
in children. J Pediatr 1994;124:S17-21. Crossref
43. Chen YC, Dong GH, Lin KC, Lee YL. Gender difference
of childhood overweight and obesity in predicting the risk
of incident asthma: a systematic review and meta-analysis.
Obes Rev 2013;14:222-31. Crossref
44. Rzehak P, Wijga AH, Keil T, et al. Body mass index
trajectory classes and incident asthma in childhood:
results from 8 European Birth Cohorts—a Global Allergy
and Asthma European Network initiative. J Allergy Clin
Immunol 2013;131:1528-36. Crossref
45. Mitchell EA, Beasley R, Björkstén B, Crane J, García-Marcos L, Keil U; ISAAC Phase Three Study Group. The association between BMI, vigorous physical activity
and television viewing and the risk of symptoms of
asthma, rhinoconjunctivitis and eczema in children
and adolescents: ISAAC Phase Three. Clin Exp Allergy
2013;43:73-84. Crossref
46. de Marco R, Pesce G, Girardi P, et al. Foetal exposure to
maternal stressful events increases the risk of having
asthma and atopic diseases in childhood. Pediatr Allergy
Immunol 2012;23:724-9. Crossref
47. Metsälä J, Lundqvist A, Virta LJ, Kaila M, Gissler M,
Virtanen SM. Mother’s and offspring’s use of antibiotics
and infant allergy to cow’s milk. Epidemiology 2013;24:303-9. Crossref
48. Fiocchi A, Pawankar R, Cuello-Garcia C, et al. World
Allergy Organization-McMaster University Guidelines for
Allergic Disease Prevention (GLAD-P): Probiotics. World
Allergy Organ J 2015;8:4. Crossref
49. McKeever TM, Lewis SA, Smith C, Hubbard R. Vaccination
and allergic disease: a birth cohort study. Am J Public
Health 2004;94:985-9. Crossref
50. Jacobsen L , Niggemann B, Dreborg S, et al. Specific
immunotherapy has long-term preventive effect of
seasonal and perennial asthma: 10-year follow-up on the
PAT study. Allergy 2007;62:943-8. Crossref
51. Marogna M, Spadolini I, Massolo A, Canonica GW,
Passalacqua G. Long-lasting effects of sublingual
immunotherapy according to its duration: a 15-year
prospective study. J Allergy Clin Immunol 2010;126:969-75. Crossref
52. Roduit C, Frei R, Depner M, et al. Increased food diversity
in the first year of life is inversely associated with allergic
diseases. J Allergy Clin Immunol 2014;133:1056-64. Crossref
53. Haahtela T, Valovirta E, Kauppi P, et al. The Finnish Allergy
Programme 2008-2018—scientific rationale and practical
implementation. Asia Pac Allergy 2012;2:275-9. Crossref
54. Chan YT, Ho HK, Lai CK, et al. Allergy in Hong Kong: an
unmet need in service provision and training. Hong Kong
Med J 2015;21:52-60. Crossref