Hong Kong Med J 2016 Jun;22(3):202–9 | Epub 29 Mar 2016
DOI: 10.12809/hkmj154575
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Comparison of clinical and pathological
characteristics between screen-detected and self-detected
breast cancers: a Hong Kong study
Silvia SS Lau, MPH (HK), MSc1;
Polly SY Cheung, FCSHK, FHKAM (Surgery)2;
TT Wong, FCSHK, FHKAM (Surgery)2;
Michael KG Ma, FRCS (Eng), FHKAM (Surgery)2;
WH Kwan, FHKCR, FHKAM (Radiology)3
1 Medical Physics & Research Department, Hong Kong Sanatorium & Hospital, Happy Valley, Hong Kong
2 Breast Care Centre, Hong Kong Sanatorium & Hospital, Happy Valley, Hong Kong
3 Department of Radiotherapy, Hong Kong Sanatorium & Hospital, Happy Valley, Hong Kong
Corresponding author: Dr Silvia SS Lau (silvialauss@yahoo.com.hk)
Abstract
Introduction: Breast cancer is the leading cause
of death of Hong Kong women with increasing
incidence. This study aimed to determine any
prognostic differences between screen-detected and
self-detected cases of breast cancer in a cohort of
Hong Kong patients.
Methods: This was a case series with internal
comparison carried out in a private hospital in Hong
Kong. Approximately 3000 cases of Chinese patients
diagnosed with ductal carcinoma in situ or invasive
breast cancer were reviewed.
Results: The screen-detected group showed better
pathological characteristics than the self-detected
group. Number of lymph nodes involved, invasive
tumour size, and tumour grade were more favourable
in the screen-detected group. There was also a lower
proportion of patients with pure invasive ductal
carcinoma and mastectomy in the screen-detected
group.
Conclusion: This study provides indirect evidence
that women in the local population may gain clinical
benefit from regular breast cancer screening. The
findings need to be validated in a representative
population of Hong Kong women.
New knowledge added by this study
- It is possible that in the Hong Kong local population, breast cancer detected by screening mammogram or ultrasound has more favourable pathological characteristics than self-detected tumours.
- Further large-scale clinical trials to evaluate the cost-effectiveness and clinical efficacy of breast cancer screening in the Hong Kong local population should be conducted. Change in prevalence of breast cancer in the female population of Hong Kong and advances in breast imaging technology may have altered the cost-benefit ratio of breast cancer screening.
Introduction
Breast cancer is the second leading cause of death
due to cancer in the world with an age-standardised
incidence rate of 43.1 per 100 000 population in 2012.1
Gøtzsche and Nielsen2 showed that early detection
of breast cancer can reduce mortality. The benefit
of mammographic screening in terms of lives saved
is greater than the harm caused by overdiagnosis;
according to Duffy et al,3 2 to 2.5 lives are saved for
every overdiagnosed case.
Breast cancer is also a significant health
problem in Hong Kong. It is the third leading cause
of death due to cancer and the most common cancer
of women.4 The crude incidence rate of breast cancer
in Hong Kong increased from 57 per 100 000 in 2000
to 91.7 per 100 000 in 2012.4
Despite this, Hong Kong does not have a
universal breast cancer screening programme for the
whole population. Women who wish to be screened
must arrange and pay for it. As the incidence of
breast cancer in Hong Kong is low compared with
western populations, there is concern about the cost-effectiveness
of a universal screening programme.
The incremental cost-effectiveness ratio for
mammography examination is relatively higher than
in the United States.5
In view of the controversy there is a need
for further studies in Hong Kong to provide local
data on the efficacy of breast cancer screening
by mammogram. This will enable policy makers,
doctors, and patients to decide on the most cost-effective
method of early breast cancer detection.
This study aimed to investigate whether there
are any prognostic differences between screen-detected
(mammography, ultrasound examination
of breasts, or clinical examination) and self-detected
breast cancers in a cohort of Hong Kong breast
cancer patients and to determine whether there is
any benefit of detection by screening.
Methods
Background of database used
A retrospective study was conducted at the Hong
Kong Sanatorium & Hospital (HKSH), a private
hospital in Hong Kong where the Breast Care
Centre provides a comprehensive breast screening
programme and breast cancer consultation services
for patients. Since 2003, all breast cancer cases
in the hospital have been discussed at a weekly
multidisciplinary breast conference. Over 50% of
cases are referred from public hospitals spread
across the whole territory.
Clinical history, and information about
diagnosis, neoadjuvant chemotherapy, surgical
treatment, postoperative pathology, and treatment
recommendations for each patient are recorded
in a structured datasheet before the conference.
The Chairman of the conference validates data by
checking the data logic during case presentation
and, if necessary, clarifying details with the doctor-in-charge. A research assistant again checked data
validity and logic by computer for cases selected
for analysis. Frequency tables, scatter plots, and cross-tabulation tables were generated for each required
variable to ensure completeness and to determine
whether any data deviated from usual clinical practice.
Subjects
All Chinese females confirmed to have in-situ or
invasive breast cancer from or referred to HKSH
between 2003 and 2010 were included in this study.
For analysis of trends of prognostic factors, only
patients between 2004 and 2010 were included as
the sample size for year 2003 was small after dividing
data into subsets by year and prognostic factors.
Ethics
The use of the database for data analysis for health
care research purposes was approved by the Research
Ethics Committee of HKSH.
Epidemiological analysis
Patients were classified into two groups, screen-detected
or self-detected tumour, before the outcomes
were reviewed. The screen-detected group included
screening mammogram, screening ultrasonogram,
or clinical examination. The self-detected
group included self-examination or presence of
symptoms at presentation. Such information was
recorded on the datasheet that was anonymised.
Demographic data of patients were retrieved and
significant prognostic factors according to St Gallen’s
risk categorisation were analysed.
Data analysis
The Statistical Package for the Social Sciences
(Windows version 18.0; SPSS Inc, Chicago [IL], US)
was used for analysis. Descriptive statistics were
used to summarise demographics, as well as pathological
and clinical characteristics of patients. Univariate
logistic regression was used to determine odds ratio
(OR) of screening status for different pathological
characteristics. Association between type of surgery
and screening status, tumour size, and age was
determined by univariate logistic regression. In
order to know how effective the models were in
predicting the type of surgery, Hosmer-Lemeshow
goodness-of-fit test was used, in which the null
hypothesis was no significant difference between
observed and predicted values of dependent variable.
Multivariate analysis was performed on the type
of surgery, which was dichotomous having breast-conserving
surgery (BCS) as reference group with
adjustment of confounding factors that included
detection mode, lymph node status, tumour size,
tumour grade, tumour stage, oestrogen receptors
(ER), progesterone receptors (PR), HER2 score,
and age. Nagelkerke’s R2 was used to show
explanatory power of model.
Data for invasive tumour size were plotted
against screening status to gain an overview of
changes between 2004 and 2010.
Results
Data from 2763 Chinese women out of 3373 cases
confirmed to have in-situ or invasive breast cancer
between 2003 and 2010 were analysed. Of the 610
cases excluded from analysis, 210 were due to
unknown histology, 258 with unknown report type,
and 142 with unknown first-detection method. Of
the patients included, 75.7% were in the self-detected
group and 24.3% in the screen-detected group. The
mean age of patients was 50.2 (range, 24-92) years,
with the highest number in both groups aged 40
to 49 years (Table 1). There was also a significant
proportion of younger patients (<40 years) in the
self-detected group (16.6%). The screen-detected
group had a statistically significant higher age at first
live birth, though the difference in mean age was
only 1 year.
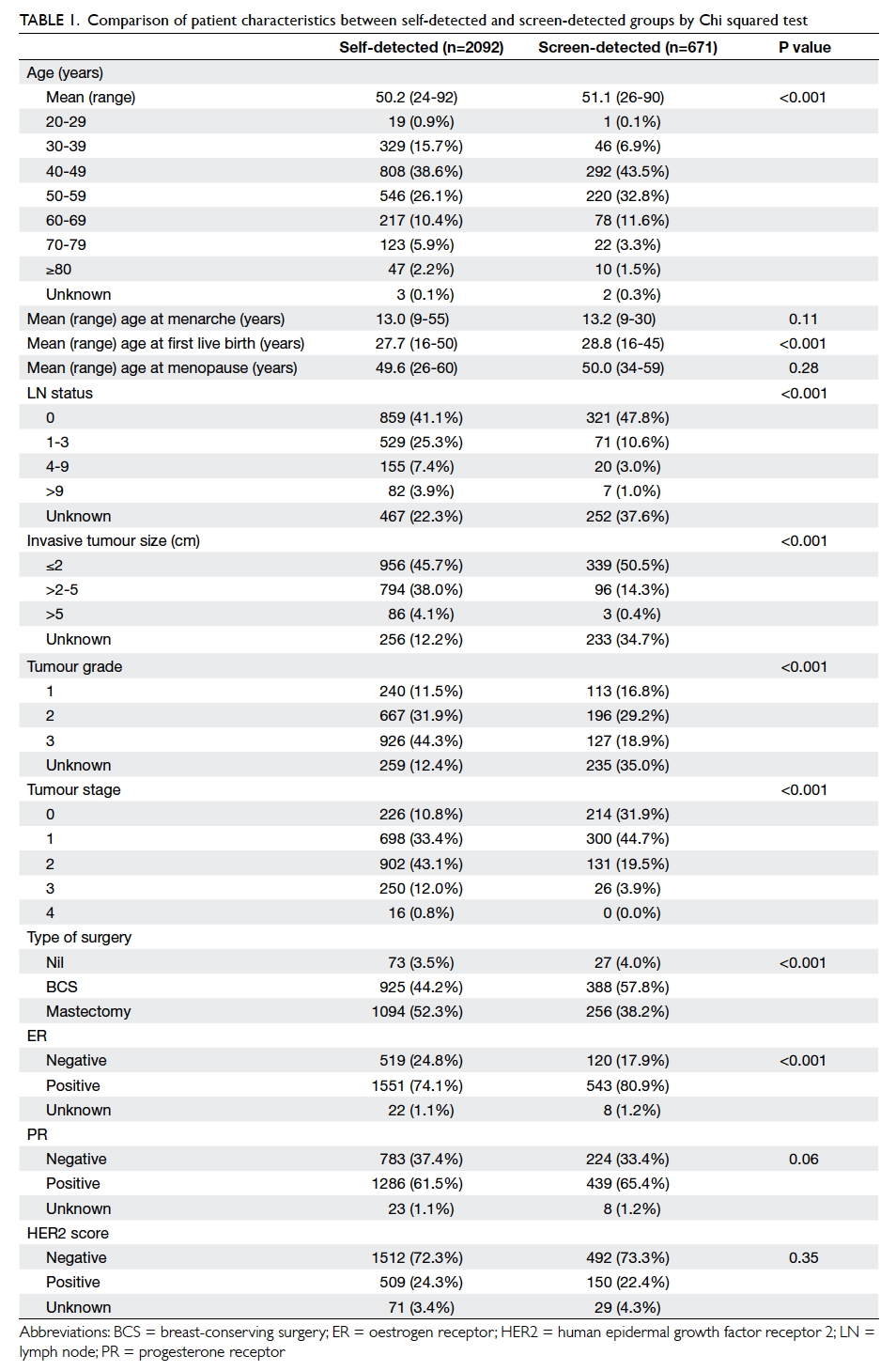
Table 1. Comparison of patient characteristics between self-detected and screen-detected groups by Chi squared test
Pathological characteristics of self-detected
and screen-detected groups are shown in Table 1. There was a significant difference in ER, but no
demonstrable significant difference in PR or HER2
status. Approximately 4% of patients in both groups
did not undergo surgery for a variety of reasons, thus
only limited information was available from biopsy
specimens about pathological characteristics.
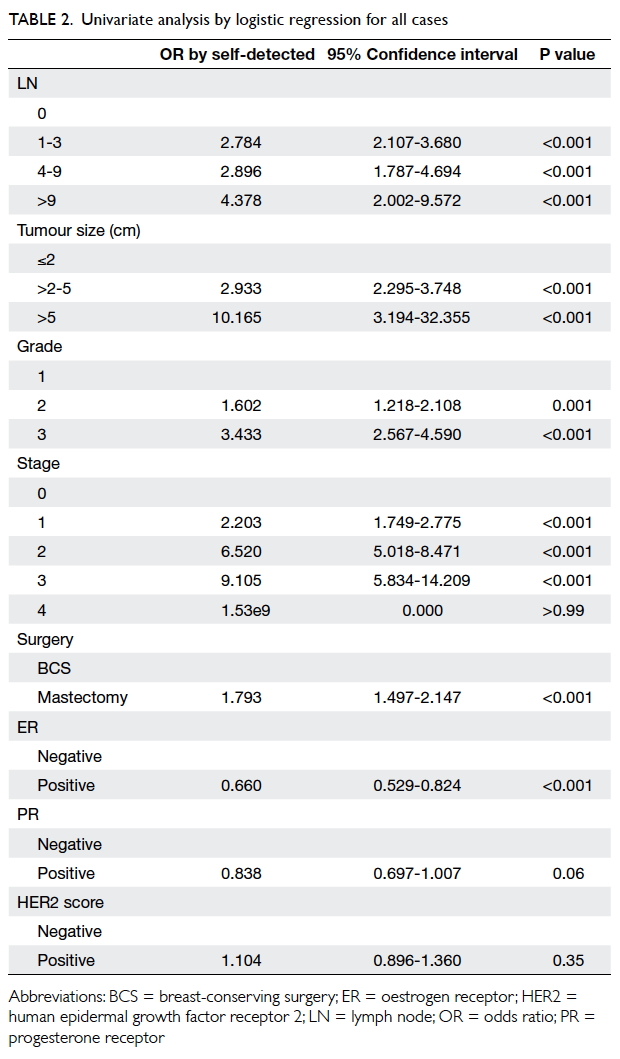
The odds of having 0 lymph nodes, smaller
tumour size, or ER/PR positivity were all higher in the
screen-detected group. Results were not statistically
significant for HER2 positivity although it showed
higher odds in the self-detected group (Table 2).
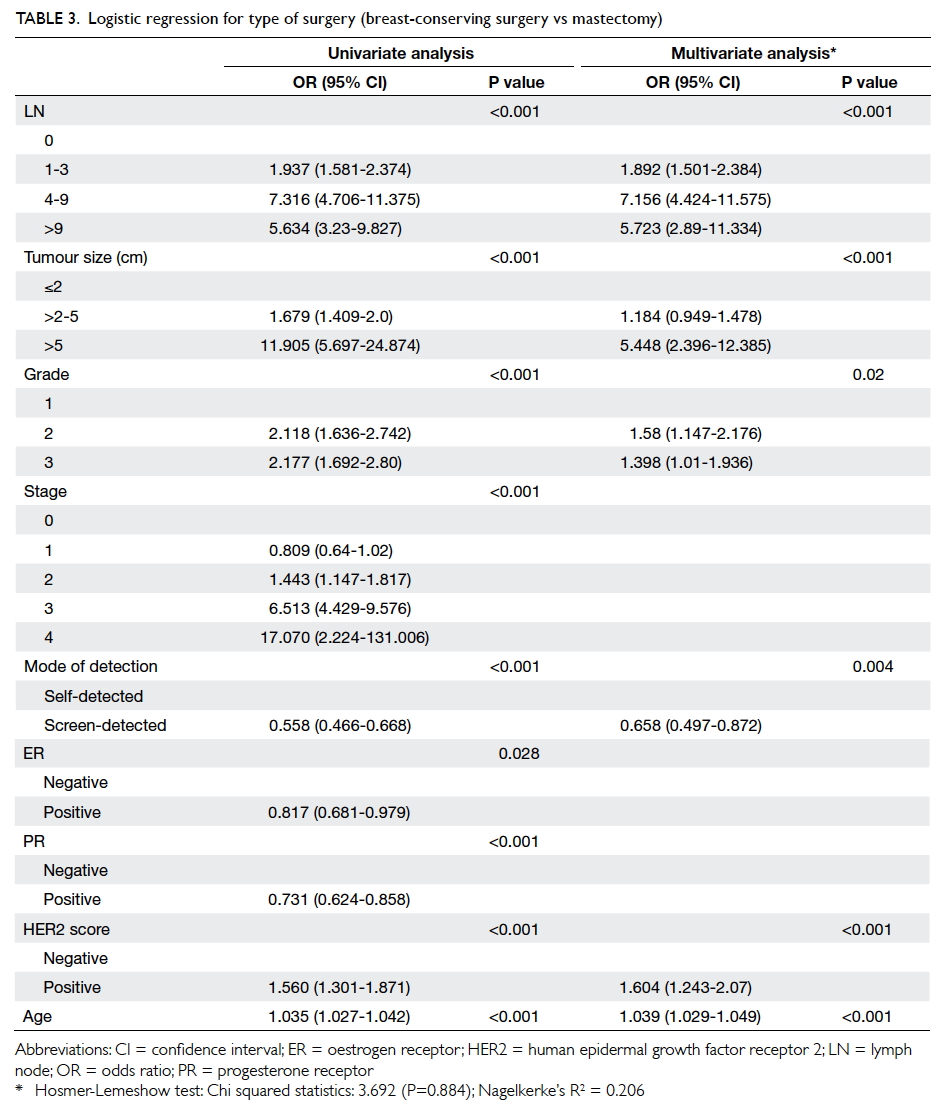
Table 3 shows that after adjustment for
potential confounding factors, patients with
screen-detected cancers were less likely to require
mastectomy (OR=0.658, P=0.004). Statistically
significant factors associated with a higher risk of
mastectomy included: positive lymph node, tumour grading
higher than 1, tumour size of >2 cm, older age, and
positive HER2 score. The Hosmer-Lemeshow
test had a P value of 0.88, meaning the goodness of fit
of the model was satisfactory at the 5% significance
level.
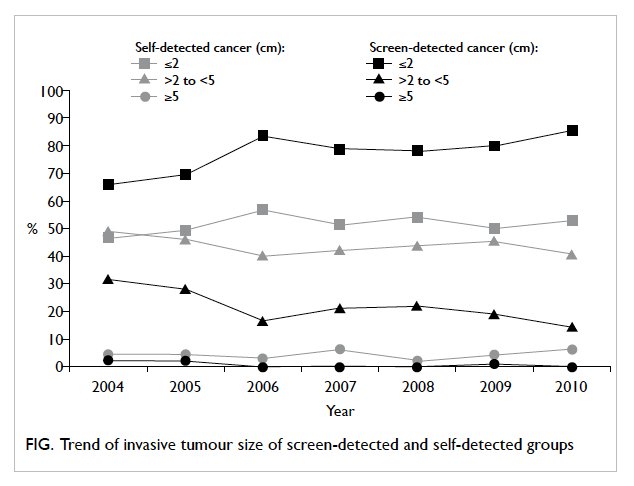
The Figure shows the trend in differences
between groups for invasive tumour size between
2004 and 2010. In the screen-detected group, there
was an increasing proportion of invasive tumours
detected when ≤2 cm and a decreasing trend for
detection of tumour of >2 to 5 cm. There was, however, no
significant difference between groups for trend of
histology, lymph node involvement, tumour grade,
type of surgery, ER positivity, or HER2 positivity.
Discussion
Although the incidence of breast cancer in Hong
Kong is half that of the United Kingdom, the
screen-detected group showed a pattern of breast
cancer diagnosis at an earlier stage compared with
the self-detected group. This is consistent with the
findings of similar studies in other countries, such
as Singapore.6 This study may provide evidence that
supports the benefits of regular screening to detect
breast cancer lesions at an early stage in Hong Kong
women. This will facilitate less invasive surgery
and a possibly better overall clinical outcome.
Breast cancer screening programmes have been
established in many countries around the world.
In order to bring Hong Kong in line with world
health care standards, more research that will result
in established and unified guidelines for the local
population is required.
Pathological risk factors
Significant prognostic factors in the St Gallen’s risk
categorisation, including number of lymph nodes
with disease, size of primary tumour, and histological
grade between the self-detected and screen-detected
groups were analysed. These prognostic factors were
chosen because they have been verified as significant
in the local population.7
In this study, screen-detected breast tumours
were of smaller size, at a lower stage and grade, and
with less lymph node involvement. Screen-detected
breast cancers in the Hong Kong population may
thus carry a better prognosis than self-detected
ones. This can serve as evidence that fulfils most
of the Wilson and Jungner criteria for a screening
evaluation programme8 and also supports breast
cancer screening in Hong Kong. Some of the criteria
for breast cancer screening that have been fulfilled
include: an important health problem (it is the second
leading cause of death from cancer in Hong Kong),
acceptable treatment is well established, facilities
for diagnosis and treatment are widely available,
natural history of the disease is well understood, and
effective treatment is available for early-stage disease.
Findings of this study suggested that breast tumours
detected on screening have a better prognosis. The
cost-benefit balance was not addressed, however,
nor screening/case-finding policies.
In the screen-detected group, a higher
percentage of tumours were ER positive. It was
revealed that ER and PR are significant prognostic
factors within the first 10 years following diagnosis.9
It is known that HER2 positivity shows poorer
prognosis8 but there was no significant difference
in HER2 status between screen-detected and self-detected
groups.
Trends
By observing the trend in size of invasive tumour
at first presentation, the stable pattern in the self-detected
group suggests that tumour detection by
the general population has not improved. On the
contrary, an increasing detection of tumours of
≤2 cm in the screen-detected group is an evidence
of the improved efficacy of screening using new
technology such as mammogram or sonogram. There
remains room for improvement in the application of
radiology. Apart from magnetic resonance imaging,
digital mammography may be more efficacious in
women younger than 50 years.9 This may change
future trends in early diagnosis.
Hormonal receptor and HER2 status
Unlike tumour size and number of lymph nodes
involved, both of which are increased in breast
tumours detected at a later stage with a consequent
poorer prognosis, prognostic factors such as status
of ER/PR and HER2 are intrinsic characteristics of
tumours. They should not differ whether or not a
tumour is detected at an earlier stage. Therefore no
statistically significant difference in these intrinsic
characteristics was expected between screen-detected
and self-detected tumours. Nonetheless, in this study, tumours in the screen-detected group
were more likely to be positive for ER, and this may
carry some prognostic implication. Further studies
may be required to investigate whether tumours
detected at an earlier stage show differences in
intrinsic factors.
Surgical treatment
When choosing between BCS and mastectomy,
detection mode, number of positive lymph nodes,
invasive tumour size, grading, staging, ER, PR, HER2
score, and age were potential significant factors.
With adjustment of these factors, detection mode
may be an independent factor that affects choice
of surgery. Screen-detected patients tended to have
BCS when the effect of number of positive lymph
nodes, tumour size, grading, HER2 score, and age
was excluded. Such surgery is less invasive than
mastectomy and is associated with better cosmetic
outcome, and may have an important impact on the
psychological health and coping ability of patients
recovering from breast cancer. Breast cancer
screening may lead to less invasive treatment with
better rehabilitation outcome.
Potential biases
Many studies have claimed longer survival in
patients with breast cancer detected by screening
mammogram. Nonetheless, this may be due to lead-time
bias: survival time appears longer because
diagnosis is earlier than in patients where tumour
has been self-detected or become symptomatic. In
addition, there is selection bias since women with
a family history of breast cancer or who are better
informed are more likely to submit to breast cancer
screening.
Cost-effectiveness
A local study suggested that population-based breast
cancer screening by mammography may not be
cost-effective in Hong Kong women.5 This balance
between cost and benefit may be altered by the rising
incidence of breast cancer in Hong Kong and the
availability of advanced breast imaging technology
that is associated with fewer false-positive diagnoses.
There may also be a broader range of screening
options, hence cost will be lowered. Therefore, the
incremental cost-effectiveness ratio may be lowered.
Recommendations
A prospective randomised controlled trial would be
the most effective study design to evaluate the
effectiveness of mammogram screening. This would require a huge amount of resources, however. In
addition, education level and household income,
which are risk factors for breast cancer, may affect a
woman’s decision to undergo a mammogram. These
confounding factors should be considered when
determining the effect of mammogram examination
on development of breast cancer. Postmenopausal
hormone replacement therapy also affects the density
of breast tissue that may hinder the effectiveness of
mammography for breast cancer screening.10
The lack of a population-based breast cancer
screening programme in Hong Kong should prompt
study of the attitude of Hong Kong women towards
breast cancer screening. Quantitative surveys or
qualitative interviews such as focus groups could help
determine their opinion of mammogram screening,
what proportion of women perform regular self-examination
or undergo clinical breast examinations
and regular mammogram examinations and how
often, and whether age is a contributing factor.
Trend study may also be meaningful if a particular
age-group shows an increasing or decreasing trend
for any of the examinations. Understanding level
of knowledge about risk factors for breast cancer
can also guide appropriate education about breast
cancer prevention.
Limitations of this study
The major strength of this study is the large number
of cases in the database, which is one of the most
comprehensive breast cancer databases available in
Hong Kong in terms of surgical and pathological
characteristics. This provides valuable information
about the characteristics of breast cancers detected
by oneself and through screening, thus allowing
a better understanding of the potential benefits
of screening by mammogram or ultrasound
examination.
This study has limitations. First, it was
not a randomised controlled trial. The presence
of confounding factors such as living standard,
household income, and education level could not be
totally excluded. There were also more self-detected
than screen-detected patients in this study, thus
data might skew towards self-detected cases. It is
ethically difficult to randomise women to a control
group of education and regular breast self-examination,
or an intervention group of regular breast cancer
screening by imaging.
Second, data were derived from a single private
hospital and findings may not be representative of
the Hong Kong population in general. Self-selection
bias, especially for attending a private hospital, is
also possible. Nonetheless, this is probably one of
the largest breast cancer databases in Hong Kong,
thus one of the best available sources of information
options at present.
Third, secondary data that had been used
in this study may not be in a format that met the
research question. Some information required may
not be available from secondary data. Only 2198
(79.6%) patients were included in the multivariate
logistic regression. Other medical and non-medical
factors that could have affected the choice of surgery
in individual patients might be related to the practice
of screening. Data on parity of women and breastfeeding
experience, which may be of interest/relevance, were also not available. Also, the potential
benefits and harm of screening were not thoroughly
examined due to the unavailability of data for
survival, mortality, and side-effects. For this study,
a long period of time was required to examine the
data and filter out required variables for analyses as
there were more than 200 variables in the database.
Information bias also exists as complete blinding of
the analysts was not possible.
Conclusion
This study suggests that in the local Hong Kong
population, breast cancers detected by screening
mammogram or ultrasound tend to be of smaller
size, lower stage, lower grade and with less lymph
node involvement, and consequent better prognosis.
Although this may not be considered conclusive
evidence to support regular screening imaging of
Hong Kong women on a population-wide basis, it
provides indirect evidence that women in our local
population may gain clinical benefit from such a
programme.
Acknowledgements
This article is adapted from a dissertation submitted
in partial fulfilment of the requirements for the Master of Public Health at the University
of Hong Kong, Hong Kong Special Administrative
Region, China. The dissertation was awarded
distinction in 2012. Part of the material in this article
was presented in the Hong Kong Sanatorium &
Hospital Li Shu Pui Symposium 2012 in Hong Kong.
The first author would like to acknowledge Dr
Joseph Wu, Assistant Professor, School of Public
Health, Li Ka Shing Faculty of Medicine, The
University of Hong Kong, for his supervision of the
project leading to completion of the dissertation
for the Master of Public Health course. The authors
would also like to thank Dr Andrew Ho, Senior
Research Assistant, who is statistical advisor
of the project. Finally, the authors would like to
express sincere appreciation to staff of Information
Technology Department of Hong Kong Sanatorium
& Hospital, who helped retrieve all necessary data
for the study.
Declaration
All authors have disclosed no conflicts of interest.
References
1. GLOBOCAN 2012: Estimated cancer incidence, mortality
and prevalence worldwide in 2012. Available from: http://globocan.iarc.fr/Pages/fact_sheets_population.aspx. Accessed Dec 2015.
2. Gøtzsche PC, Nielsen M. Screening for breast cancer
with mammography. Cochrane Database Syst Rev
2011;(1):CD001877. Crossref
3. Duffy SW, Tabar L, Olsen AH, et al. Absolute numbers of
lives saved and overdiagnosis in breast cancer screening,
from a randomized trial and from the Breast Screening
Programme in England. J Med Screen 2010;17:25-30. Crossref
4. Hong Kong Cancer Registry. Female breast cancer in Hong
Kong. Available from: http://www3.ha.org.hk/cancereg/breast_2012.pdf. Accessed Jan 2016.
5. Wong IO, Kuntz KM, Cowling BJ, Lam CL, Leung GM.
Cost-effectiveness analysis of mammography screening
in Hong Kong Chinese using state-transition Markov
modelling. Hong Kong Med J 2010;16(Suppl 3):38S-41S.
6. Chuwa EW, Yeo AW, Koong HN, et al. Early detection of
breast cancer through population-based mammographic
screening in Asian women: a comparison study between
screen-detected and symptomatic breast cancers. Breast J
2009;15:133-9. Crossref
7. Yau TK, Soong IS, Chan K, et al. Evaluation of the
prognostic value of 2005 St. Gallen risk categories for
operated breast cancers in Hong Kong. Breast 2008;17:58-63. Crossref
8. Wilson JM, Jungner G. Principles and practice of screening
for disease. Public Health Papers. No. 34. Geneva: World
Health Organization; 1968.
9. Soerjomataram I, Louwman MW, Ribot JG, Roukema JA,
Coebergh JW. An overview of prognostic factors for long-term
survivors of breast cancer. Breast Cancer Res Treat
2008;107:309-30. Crossref
10. Cox B, Ballard-Barbash R, Broeders M, et al. Recording of
hormone therapy and breast density in breast screening
programs: summary and recommendations of the
International Cancer Screening Network. Breast Cancer
Res Treat 2010;124:793-800. Crossref