DOI: 10.12809/hkmj144324
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Robotic left hepatectomy and Roux-en-Y right
hepatico-jejunostomy for biliary papillomatosis
Carmen CW Chu, MB, ChB, FRCSEd; Eric CH Lai, MB, ChB, FRACS; Oliver CY Chan, MB, ChB, FRCSEd; Daniel TM Chung, MB, ChB, FRCSEd; CN Tang, MB, BS, FRCSEd
Department of Surgery, Pamela Youde Nethersole Eastern Hospital, Chai Wan, Hong Kong
Corresponding author: Dr Eric CH Lai (ericlai@alumni.cuhk.edu.hk)
Case report
An 83-year-old male was referred to us for
deranged liver function in December 2010. There
was mildly elevated bilirubin level of 36 µmol/L,
alkaline phosphatase level of 281 µmol/L, and
transaminase level of 98 µmol/L. Tumour markers
(carcinoembryonic antigen, alpha-fetoprotein,
and carbohydrate antigen 19-9) were normal.
Ultrasonography revealed a markedly dilated common bile duct (CBD) and intrahepatic ducts with
irregular mural lesions.
Endoscopic retrograde cholangiopancreatography
(ERCP) showed a grossly dilated CBD and intrahepatic ducts filled with thick mucus
and multiple large filling defects. Brush cytology
revealed atypical cells. A nasobiliary drainage
catheter was inserted for biliary decompression.
Bilateral percutaneous transhepatic biliary drainage
(PTBD) catheters were later inserted due to
inefficient nasobiliary drainage.
Further evaluation by computed tomographic
scan showed dilatation of the whole biliary system
with multiple papilloma-like lesions as shown
in Figure 1. The presence of mucus in the biliary
tree and image findings raised the suspicion of
biliary papillomatosis. In order to localise and
assess the extent of involvement, intra-operative
choledochoscopy was performed via the PTBD
tract. The PTBD tract was serially dilated up to 14
Fr to allow passage of a choledochoscope. Multiple
biliary papillomas over the left hepatic duct,
hilar bifurcation, and upper main bile duct were
visualised. The right biliary system, lower CBD, and ampullary region were disease-free.
After thorough assessment by intra-operative
choledochoscopy, left hepatectomy and main bile
duct excision with right hepatico-jejunostomy
via robot-assisted laparoscopic approach was
performed.
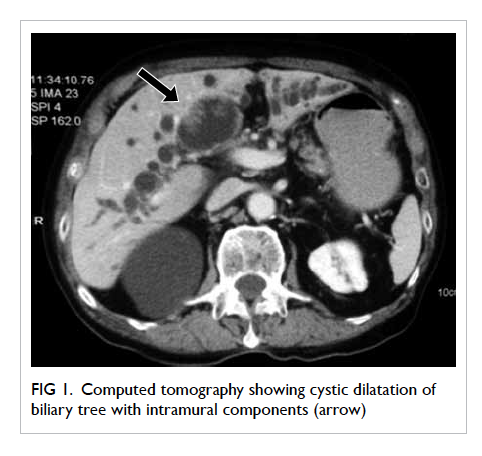
Figure 1. Computed tomography showing cystic dilatation of biliary tree with intramural components (arrow)
The patient was placed in the reverse
Trendelenburg position with legs spread apart, and a
5- to 12-mm subumbilical port was inserted with the
establishment of carbon dioxide pneumoperitoneum.
After diagnostic laparoscopy, five trocars were
inserted under direct vision. The extent of disease
was assessed by intra-operative ultrasonography (BK
Medical, Denmark). The da Vinci S Surgical System
(Intuitive Surgical Inc, Sunnyvale [CA], US) was
brought into position over the patient’s head and
docked in. The assistant surgeon stayed on the right
side of the patient and performed suction, stapling,
and clipping through an assistant port over the right
lower quadrant.
The intended extent of parenchymal
resection was first marked on the liver surface with
electrocautery. The main extrahepatic bile duct was
dissected and slung with vascular tape. The right
hepatic duct and lower CBD were transected and
confirmed to have clear resection margins on frozen
section. Porta dissection was performed. The left
hepatic artery and left porta vein were dissected
and transected. The main and right hepatic artery,
and main and right portal vein were identified and
protected. Left hemihepatectomy was performed
with an ultrasonic surgical aspirator (SonoSurg,
SS; Olympus Medical Systems Corporation, Tokyo,
Japan) and coagulative scissors, under hemivascular
inflow control. Large branches of vascular structures
were controlled with endostaplers. A right hepatico-jejunostomy
via Roux-en-Y reconstruction was
fashioned with 3-0 poliglecaprone 25 (Monocryl,
Ethicon; Johnson & Johnson, Amersfoort, The
Netherlands) sutures intracorporeally. The side-to-side jejunojejunostomy was performed and
the enterotomy site closed intracorporeally with
an endostapler and 3-0 monocryl sutures. The
specimen (Fig 2) was delivered via the extension
of the left abdominal port. Operating time was
367 minutes and operative blood loss was 200 mL.
The postoperative course was uneventful and the
patient was discharged on postoperative day 13.
Histopathological examination revealed extensive
papillomatosis with villous adenomatous changes
over both left hepatic ducts and the CBD associated with moderate-to-severe dysplasia.
There was no evidence of invasion to suggest
malignant transformation. At 50-month follow-up,
the patient remained disease-free with no further
biliary obstruction.
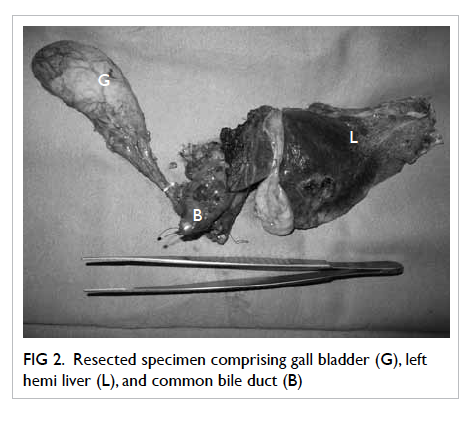
Figure 2. Resected specimen comprising gall bladder (G), left hemi liver (L), and common bile duct (B)
Discussion
Biliary papillomatosis is a rare condition
characterised by papillary proliferation of the lining
columnar epithelium of the bile ducts. It was first
reported by Chappet1 in 1894 and was initially
thought to be an entity with low malignant potential.
Malignant transformation, however, is noted in
20% to 50% of cases as a consequence of adenoma
carcinoma sequence.2 3
Middle-aged to elderly patients are commonly
affected with a slight male predominance. The clinical
presentation varies from being asymptomatic, as in
our patient, to the presence of recurrent abdominal
pain, obstructive jaundice, or recurrent cholangitis
due to biliary obstruction by mucus.
The exact pathogenesis remains to be
elucidated, but biliary papillomatosis is associated
with conditions such as recurrent pyogenic
cholangitis and congenital choledochal cyst. It has
been postulated that longstanding irritation by
stones or infection stimulates reactive hyperplasia
with subsequent dysplasia in the biliary system.
Despite considerable improvements in
imaging techniques, diagnosis remains a challenge
as the presenting symptoms are more commonly
caused by choledocholithiasis. Ultrasonography and
computed tomography reveal intrabiliary masses
with cystic dilatation in the proximal biliary tree.
On the other hand, ERCP or magnetic resonance
cholangiopancreatography shows an irregular
filling defect that causes obstruction with proximal
dilatation. The presence of mucobilia should raise
the suspicion of biliary papillomatosis.
Histopathological examination reveals that the
biliary system is often replaced by velvety papillary
growth that possesses a fibrovascular core lined by
columnar epithelium with varying degrees of cellular
atypia.
Management is difficult due to the diffuse
nature of the disease. A range of treatment strategies
that include local ablation, photodynamic therapy,
radical excision, or total hepatectomy with liver
transplantation have been reported. Local ablative
therapy and curettage, and radical excision with
clear resection margins are associated with better
survival.2 4
Accurate localisation and assessment of the
extent of disease involvement remains pertinent to
an accurate choice of treatment. In a Korean series
by Lee et al,2 curative resection was associated with
significantly better survival (60 months in curative
resection vs 36 months in palliative surgery group);
similar results were demonstrated by another series
of 18 cases in China.5 Due to the high propensity
for diffuse involvement, recurrence and malignant
transformation, timely diagnosis and radical
resection remain the cornerstone for successful
treatment.
The advent of robotic surgery has brought
about revolutionary changes in current surgical
developments, but the feasibility and benefits in
hepatobiliary surgeries are yet to be explored. Deep
anatomical locations, complex vascularity, and
large organ volume in hepatobiliary surgery often
pose a challenge to the conventional laparoscopic
approach. Such hurdles can be overcome by robotic
surgery: recent studies have shown that a robot-assisted
approach offers a safe and feasible option for
hepatobiliary surgery with promising results.6 7 8 9 10 The
enhanced dexterity of EndoWrist (Intuitive Surgical
Inc, Sunnyvale [CA], US), with its 7 degrees of
freedom of movement, allows meticulous dissection
and precise tissue handling, enabling intracorporeal
suturing even in the most technically demanding
areas that would otherwise be impossible to
access in conventional laparoscopic surgery. The
three-dimensional stereoscopic video system with
magnification enhances visualisation and depth
perception. The third robotic arm also allows better
organ retraction. The improving technical abilities of
the robotic system for dissection and suturing extend
the indications of minimally invasive liver surgery
to liver resection requiring a biliary reconstruction.
Without any doubt, the operation described in this
case requires high technical skill and experience,
and cannot be quickly introduced into routine
practice. We performed this operation following
accumulation of 10 years’ experience of conventional
laparoscopic liver surgery and 2 years’ experience of
robotic liver resection and robotic biliary surgery.8 9 10 11 12
Nonetheless, we believe that with the increasing
popularity of robotic surgery, the required skill
can be acquired with time. With the help of a
robotic system, unilateral hepatico-jejunostomy
reconstruction and porta structure dissection can be
performed more easily than with the conventional
laparoscopic technique.
In conclusion, the robotic approach to
treatment of biliary papillomatosis is feasible and
safe in selected patients. It also has the advantage of
being minimally invasive.
References
1. Chappet V. Cancer epithelial primitif du canal cholédoque.
Lyon Med 1894;76:145-57.
2. Lee SS, Kim MH, Lee SK, et al. Clinicopathologic
review of 58 patients with biliary papillomatosis. Cancer
2004;100:783-93. Crossref
3. Wu SD, Lu CD, Lu CJ, Huang J, Zhou J. Mucin-producing
intrahepatic biliary papillomatosis. Surg Today
2010;40:845-50. Crossref
4. Ludwig L, Büchler P, Kleeff J, et al. Multidisciplinary
treatment of aggressive and rapidly progressing biliary
papillomatosis. Dig Dis Sci 2010;55:3627-9. Crossref
5. Jiang L, Yan LN, Jiang LS, et al. Biliary papillomatosis:
analysis of 18 cases. Chin Med J (Engl) 2008;121:2610-2.
6. Giulianotti PC, Sbrana F, Coratti A, et al. Totally robotic
right hepatectomy: surgical technique and outcomes. Arch
Surg 2011;146:844-50. Crossref
7. Choi GH, Choi SH, Kim SH, et al. Robotic liver resection:
technique and results of 30 consecutive procedures. Surg
Endosc 2012;26:2247-58. Crossref
8. Lai EC, Tang CN, Yang GP, Li MK. Multimodality
laparoscopic liver resection for hepatic malignancy—from
conventional total laparoscopic approach to robot-assisted
laparoscopic approach. Int J Surg 2011;9:324-8. Crossref
9. Lai EC, Tang CN, Li MK. Robot-assisted laparoscopic
hemi-hepatectomy: technique and surgical outcomes. Int
J Surg 2012;10:11-5. Crossref
10. Lai EC, Yang GP, Tang CN. Robot-assisted laparoscopic
liver resection for hepatocellular carcinoma: short-term
outcome. Am J Surg 2013;205:697-702. Crossref
11. Lai EC, Tang CN, Ha JP, Li MK. Laparoscopic liver resection
for hepatocellular carcinoma: ten-year experience in a
single center. Arch Surg 2009;144:143-7; discussion 148. Crossref
12. Lai EC, Tang CN, Yang GP, Li MK. Minimally invasive
surgical treatment of hepatocellular carcinoma: long-term
outcome. World J Surg 2009;33:2150-4. Crossref

