Hong Kong Med J 2016 Feb;22(1):56–61 | Epub 8 Jan 2016
DOI: 10.12809/hkmj154600
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Hysteroscopic intrauterine morcellation of submucosal fibroids: preliminary results in Hong Kong and comparisons with conventional hysteroscopic monopolar loop resection
Menelik MH Lee, FHKCOG, FHKAM (Obstetrics and Gynaecology);
Tomoko Matsuzono, FHKCOG, FHKAM (Obstetrics and Gynaecology)
Department of Obstetrics and Gynaecology, Queen Elizabeth Hospital, Jordan, Hong Kong
Corresponding author: Dr Menelik MH Lee (menelik.lee@gmail.com)
Abstract
Introduction: Hysteroscopic management of submucosal fibroids using the intrauterine morcellation technique is increasingly being adopted worldwide but no literature concerning its safety and efficacy is available within our local population. We aimed to determine the safety, satisfaction, and efficiency of hysteroscopic intrauterine morcellation of submucosal fibroids, and to compare this technique with conventional hysteroscopic monopolar loop resection to identify its potential benefits.
Methods: All cases of hysteroscopic resection of
submucosal fibroids performed in a regional hospital
in Hong Kong between 1 January 2011 and 31
December 2014, either by hysteroscopic intrauterine
morcellation (MyoSure; Hologic, Bedford [MA], US)
or conventional hysteroscopic monopolar loop resection,
were selected and case notes reviewed. Technical
details such as fibroid size, operating time, fluid
deficit, operative complications, patient satisfaction,
and improvement in haemoglobin level were
analysed and compared between the hysteroscopic
intrauterine morcellation and the conventional
groups. All statistical results were calculated using
the Mann-Whitney test.
Results: During the 3-year period, 29 cases of
submucosal fibroids were managed by hysteroscopic
surgery. Conventional hysteroscopic monopolar loop
resection was performed in 14 patients and another 15
underwent hysteroscopic intrauterine morcellation
with the MyoSure device. At 3-month follow-up,
there was no significant difference in overall patient
satisfaction (84.6% for conventional method vs 93.3%
for hysteroscopic intrauterine morcellation method;
P=0.841). Both techniques showed improvement
in haemoglobin level at 3 months but without
significant difference between the two groups: +21.5
g/L (+1 to +44 g/L) for conventional group and +17.0 g/L (-4 to +40 g/L)
for hysteroscopic intrauterine
morcellation group (P=0.235). Both techniques
achieved 100% satisfaction if the submucosal fibroid
had over 60% of its contents protruding into the
uterine cavity. The operating time was significantly
reduced for the hysteroscopic intrauterine
morcellation technique (mean, 36.6 mins vs 53.6
mins in conventional hysteroscopic monopolar loop
resection; P=0.005), particularly in those whose
fibroids were ≤3.0 cm (mean, 27.6 mins
vs 53.4 mins; P=0.019).
Conclusions: This retrospective review suggests
that hysteroscopic intrauterine morcellation of
submucosal fibroids is a safe and effective method in
the management of menorrhagia in Chinese women.
Preliminary data suggest this technique to be less
time-consuming, especially when managing fibroids
of ≤3.0 cm.
New knowledge added by this study
- Hysteroscopic intrauterine morcellation of submucosal fibroids is as effective as conventional hysteroscopic resection of submucosal fibroids. The operating time is shorter than the conventional technique, particularly when the submucosal fibroid is ≤3.0 cm.
- Reduced operating time for management of submucosal fibroids will enable more such procedures to be performed within a set limit of time. This may reduce waiting time for surgery and improve overall patient satisfaction, particularly in a public hospital setting.
Introduction
Submucosal fibroids are a common cause of heavy
menstrual bleeding.1 Traditionally, conventional
hysteroscopic monopolar loop resection of such fibroids
represents the surgical treatment of choice (Fig 1a).
Hysteroscopic management of such fibroids using
the intrauterine morcellation (IUM) technique (eg
MyoSure, Hologic, Bedford, US; Truclear, Smith
& Nephew Inc, Andover, US; Fig 1b), however, is
increasingly being used worldwide but no literature
concerning its safety and efficacy is available within
our local population.
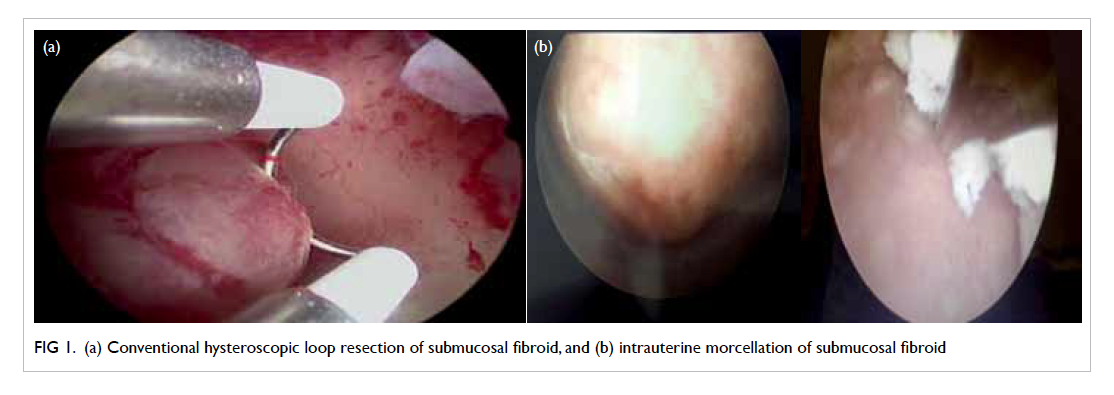
Figure 1. (a) Conventional hysteroscopic loop resection of submucosal fibroid, and (b) intrauterine morcellation of submucosal fibroid
Our hospital is one of the first to introduce
the use of the hysteroscopic IUM device in Hong
Kong. This preliminary review looks at the safety,
satisfaction, and efficiency of such technique when
performed within our hospital and within a Chinese
population. Comparisons were made between
the conventional hysteroscopic monopolar loop resection
technique and IUM technique with the aim of
identifying the potential benefits that have been
described by previous studies worldwide.
Methods
All cases of hysteroscopic resection of submucosal
fibroids performed at Queen Elizabeth Hospital,
Hong Kong, between 1 January 2011 and 31
December 2014, either by IUM (MyoSure) or
conventional hysteroscopic monopolar loop resection, were
selected and the case notes were reviewed. Choice of
method was dependant on the operator but all cases
using the IUM method were performed between
the years 2013 and 2014 after its introduction in
our department. Patients were identified from the
Clinical Data Analysis and Reporting System through
specialised coding. Detailed technical aspects of
both operations were collected using a self-designed
proforma with information collected via the Clinical
Management System computerised record system.
Analysis and comparison of technical details
such as fibroid size, operating time, fluid deficit,
operative complications, and patient satisfaction
were made between the IUM and the conventional
groups. Fibroid size was measured via preoperative
abdominal and/or vaginal fluid–infused sonography, and confirmed during diagnostic
hysteroscopy prior to resection. Those cases with
prolonged operating time due to multiple operations
for other indications or complications were excluded
from final analysis. In our hospital, monopolar
energy was used during conventional loop resection,
hence glycine was used as the distending medium.
With the IUM technique, since no energy source
was required during morcellation, normal saline
was used as the distending medium. Operating
time was measured from the time the patient was
anaesthetised to completion of the operation.
Hence operating time included the time required to
position the patient, cleaning, draping, and the time
for setting up equipment. In the IUM system, fluid
deficit calculations were accurately measured by the
Aquilex Fluid Control System (Hologic, Bedford, US).
With the conventional method, deficit calculations
were based on the amount of fluid entered minus
the amount of fluid suctioned and retrieved intra-operatively.
Postoperatively, a satisfactory outcome
was considered when the patient subjectively
reported reduced menstrual bleeding and considered
the operation to have improved menstrual
symptoms at 3 months’ follow-up. Pre- and post-operative
haemoglobin levels within 3 months of
follow-up and differences between them were also
investigated. All results were statistically analysed
using the Statistical Package for the Social Sciences
(Windows version 22.0; SPSS Inc, Chicago [IL], US).
Statistical significance was represented by P values
that were calculated using the Chi squared test for
patient satisfaction and Mann-Whitney test for the
remaining tests. P values of <0.05 were considered
statistically significant for all of the data.
The research protocol was approved by the
Ethics Committee of the study hospital. The patients
were not required to undergo additional tests or
visits, and therefore consent from the patients was
not required.
Results
During the study period, 29 patients with submucosal
fibroids were treated with hysteroscopic surgery at
Queen Elizabeth Hospital, Hong Kong. Conventional
hysteroscopic monopolar loop resection was performed in
14 patients and IUM with the MyoSure device in 15.
Among those who underwent surgery using the
conventional technique, one patient experienced a
uterine perforation that required surgical repair and
was excluded from data analysis. No complications
occurred in any patient in the IUM group. Two
patients from the IUM group and one from the
conventional group were excluded due to the need
for multiple procedures including endometrial
ablation or laparoscopic ovarian cystectomy during
the same operation. The remaining patients were
all well and discharged the day after their operation
regardless of the hysteroscopic technique used.
The mean size of fibroids resected was 3.3 cm
(range, 2-5 cm; median, 3 cm) for the conventional
technique and 3.5 (range, 1.5-6 cm; median, 3
cm) for the IUM group, although they were not
significantly different (P=0.470). The operating time
was significantly shorter using the IUM technique
(mean, 36.6 mins; range, 17-72 mins) compared with
the conventional technique (mean, 53.6 mins; range,
39-102 mins) [P=0.005]. Total fluid deficit,
however, was significantly greater when using the
IUM technique (1005 mL; range, 40-2600 mL)
compared with the conventional technique (225 mL;
range, 0-1000 mL) [P=0.003; Table 1]. No patient in
either group developed any complication associated
with excessive fluid absorption.
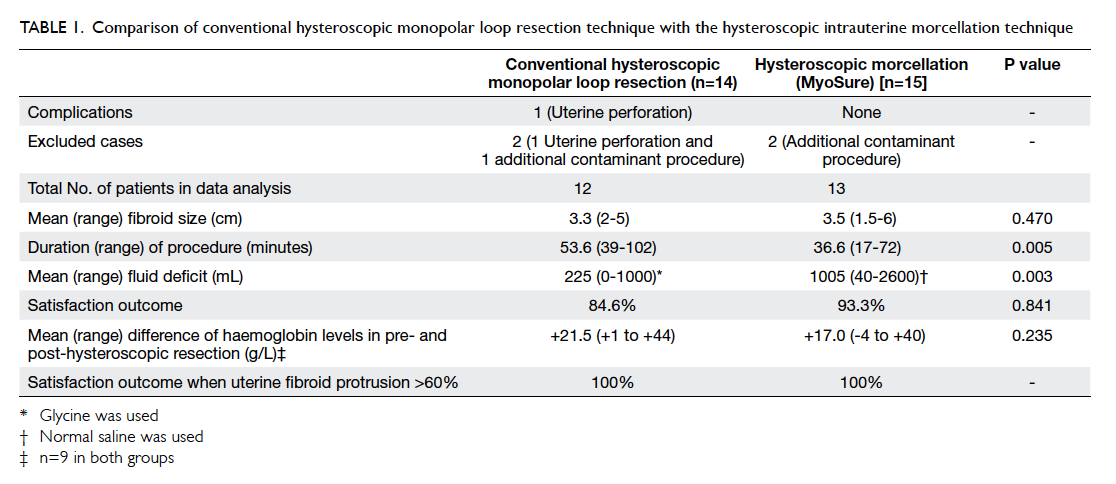
Table 1. Comparison of conventional hysteroscopic monopolar loop resection technique with the hysteroscopic intrauterine morcellation technique
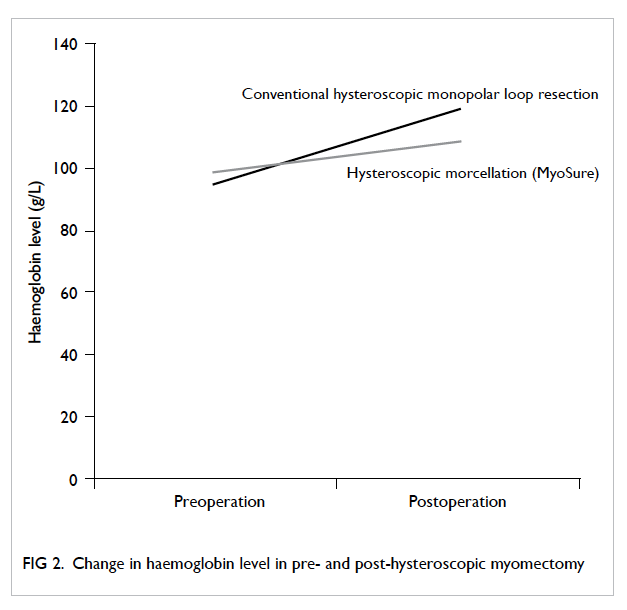
At 3 months’ follow-up, there was no
significant difference in the overall outcome
between the two groups: 84.6% of patients who
underwent the conventional method versus 93.3% of
those who underwent IUM were pleased with their
overall outcome (P=0.841). Within the conventional
group, the mean preoperative haemoglobin level
was 95.4 g/L (range, 81-121 g/L). The mean
postoperative haemoglobin level of nine patients
who returned with blood results was 119 g/L (range,
91-137 g/L). The difference between pre- and post-haemoglobin
level in the conventional resection
group was +21.5 g/L (range, +1 to +44 g/L). In the
IUM group, two patients were excluded from this
part of the analysis as the indication for surgery was
post-menopausal bleeding, not menorrhagia. For
the remaining 11 patients, the mean preoperative
haemoglobin level was 99.1 g/L (range, 62-120 g/L).
The mean postoperative haemoglobin level among
the nine patients in the IUM group who returned
with results was 108.8 g/L (range, 90-124 g/L). The
mean improvement in haemoglobin level was +17.0
g/L (range, -4 to +40 g/L). There was no significant
difference between the change in haemoglobin level
pre- and post-operatively between the IUM and
conventional groups (P=0.235, Mann-Whitney test;
Fig 2).
For both techniques, each group had two
patients in whom fibroid protrusion was <60%
within the uterine cavity, with the remaining
patients all having >60% protrusion. Of those with
<60% protrusion, each group had one (50%) of two
patients who was satisfied with the procedure. In
those with >60%, 100% of patients were satisfied
(n=10 for conventional group and n=11 for IUM
group; Table 1).
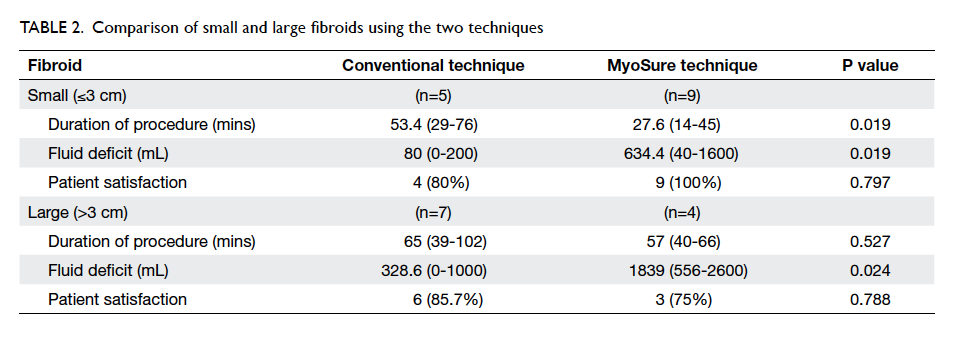
The data were further divided into groups of
small and large fibroids with the cut-off of 3.0 cm
to differentiate the two groups. With regard to small
fibroids of ≤3.0 cm, the mean duration of procedure
was significantly reduced among those using the IUM
system (mean, 27.6 mins vs 53.4 mins; P=0.019), but
fluid deficit was significantly greater (mean, 634.4 mL
using IUM vs 80 mL using conventional technique;
P=0.019; Table 2). There was no statistical difference
in overall satisfaction for the two methods. When
the procedure involved larger fibroids (>3.0 cm),
there was no difference in operating time (P=0.527)
or patient satisfaction (P=0.788) between the two
methods but considerably more fluid deficit was
again generated using the IUM system (mean, 328.6
mL using conventional technique vs 1839 mL using
IUM; P=0.024; Table 2).
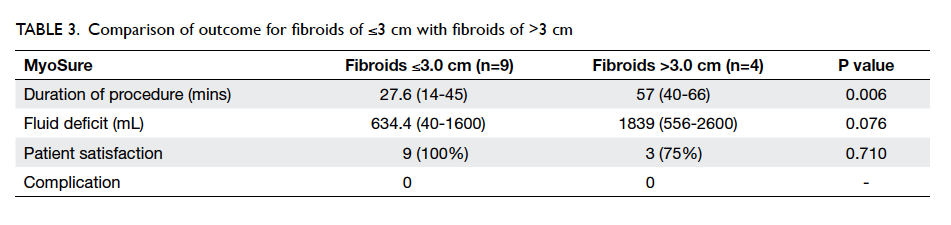
When we reviewed the data for all patients
who underwent submucosal fibroid resection using
the IUM technique, the procedural time was significantly reduced, while fluid deficit had a lowering trend with smaller
fibroids compared with larger fibroids. Regardless
of fibroid size, however, there was no significant
difference in overall patient satisfaction (P=0.710;
Table 3).
Discussion
Hysteroscopic surgery using hysteroscopic monopolar loop resection has always been the conventional
method to resect submucosal fibroids. Recently,
hysteroscopic intrauterine morcellators such as
MyoSure have been increasingly used as an alternative.
Reports have suggested that such techniques to
remove submucosal fibroids and polyps are as
effective as the conventional hysteroscopic resection
while fibroid symptom–related quality of life is
improved and the recurrence of endometrial polyp
reduced.2 3 Reports have suggested that IUM may be associated with adverse complications such as bowel
damage, hysterectomy, uterine perforation, and
pelvic infection, but an adverse event complication
rate of <1% for hysteroscopic morcellation technique
is lower than that for conventional electrocautery.4
Other reports have suggested additional benefits
such as reduction in instances of uterine perforation,
cervical dilation, thermal bowel injury, and
intrauterine adhesions when comparing the use of
such a device with conventional methods. Operating
time, fluid absorption, and the need for a second
operation may also be reduced.5 6 7
Despite its increasing popularity worldwide,
the IUM technique remains a relatively new concept
within the Chinese population. In this retrospective
review, among the 13 patients who underwent
IUM for the management of submucosal fibroids,
none developed intra-operative complications or
postoperative complications that could lead to an
extended hospital stay.
Excessive fluid deficit and subsequent fluid
absorption remains a concern with hysteroscopic
surgery. Electrolyte imbalance as well as cardiac
collapse and death can occur in severe cases. This is
more likely if hypotonic glycine is used as the uterine
distention medium: normal saline reduces such risks.8
In our study, the IUM technique was associated with
significantly higher fluid deficit regardless of fibroid
size being morcellated. One explanation of this is
the fast fluid pumping device that is used with the
IUM. High fluid flow within the cavity is important
to maintain a clear view during the morcellation
procedure and to maintain a high intrauterine
pressure to prevent bleeding during the myoma
morcellation process. Normal saline was used in the
IUM technique instead of glycine (which was used
in conventional technique). Despite its significantly
higher fluid deficit, no patients experienced any
associated complications.9 In both techniques and
regardless of the size of the submucosal fibroids, the
total amount of fluid deficit remained within or just
above the maximum limit of 2500 mL of saline or
1000 mL glycine set by AAGL (American Association
of Gynecologic Laparoscopists).10 One patient who
underwent IUM had 100 mL (2600 mL) above the
recommended maximum fluid deficit limit. This was
due to the additional time required to completely
resect a large 6-cm fibroid and avoided a second
operation. This patient recovered well and did not
have any complications. Hence despite the excessive
fluid deficit, IUM remains a safe procedure.
When the technicalities of both techniques
were compared, the total time required for the
operation was significantly reduced when the IUM
technique was used. This was particularly significant
if the fibroid size was ≤3 cm but not if the fibroid
was >3 cm; 3 cm was chosen as the cut-off between
small and large fibroid as previous studies have
already shown morcellation of submucosal fibroids
of ≤3.0 cm to be safe and effective.11 12 One of the
main reasons for the reduced operating time was the
constant suction mechanism at the morcellator blade
of the IUM device. This suction constantly removes
resected material to maintain a clear view of the
uterine cavity. The material is collected directly into
the Aquilex Fluid Control System that is required
for the MyoSure IUM device. As a result, unlike the
conventional method, the need to constantly remove
fibroid chips during the procedure is avoided and
hence operating time is reduced. With the larger-sized
fibroids, the time needed to morcellate the
large fibroid will still be considerable so there is a
smaller difference compared with conventional
methods. One may suggest that the reduced
time difference may be due to the experience of
the operator, as the IUM is a new technique within
our department. Previous study has suggested that
both experienced operators and training doctors
favour the morcellation technique and the learning
curve is minimal.12 Familiarisation with the setup
of the system, the technique of hysteroscopic
morcellation, management of a loose cervix that
can cause fluid leakage as well as fluid control to
maintain haemostasis versus a clear visual field
remain a challenge. Given more experience with
the IUM system, reduced operating times will
become more significant. This proposed reduction
in operating time will benefit both patient (eg
anaesthetic exposure) and the institution (reduced
waiting time for operation). Other potential benefits
described by other studies such as reduced uterine
perforation, cervical dilation, thermal bowel injury,
and intrauterine adhesions5 6 7 cannot be determined
given the small number of cases performed so far.
Nonetheless, there has been one case of uterine and
subsequent bowel perforation with the conventional
technique and none with the IUM technique in this study.
Patient satisfaction in terms of reduced or
improved menstrual symptoms showed no significant
difference at 3 months’ follow-up when the IUM
technique was compared with the conventional
technique. Haemoglobin levels improved following
hysteroscopic resection of fibroid regardless of
the technique used, with no significant difference
in improvement between the two groups. Patient
satisfaction again showed no statistically significant
difference regardless of the size of the submucosal
fibroids, suggesting that the IUM technique can
be applied to large fibroids. If cases were carefully
selected and only submucous fibroids with less
than 50% of the contents intramural were surgically
resected as suggested by Di Spiezio Sardo et al,7 the
satisfaction rate would remain the same between
the two techniques, that is both achieved 100%
satisfaction.
Limitations
Although results regarding safety, effectiveness,
and benefits of the IUM technique appear to
be promising, this study remains a preliminary
overview as the strength of the evidence is limited
by the small number of cases. The limited sample
may not be representative of the general population
and the two groups using different techniques may
not be comparable. As a result of the small numbers,
this in itself and the non-parametric test used due
to the lack of numbers reduce its statistical power.
Limitations also arise when the skill of the surgeon
varies and the total operating time incorporates
the time for preparation and setting up for the
procedure. The latter may cause discrepancy in the
actual total operating time. Further prospective
studies or randomised controlled trials with more
subjects, a limited number of surgeons with similar
hysteroscopic skills, and a more accurate surgical
time measurement would be more beneficial. More
standardised outcome measures using a combination
of haemoglobin improvement, menstrual chart, and/or patient satisfaction surveys may also improve the
strength of future studies.
Conclusions
This retrospective review suggests that hysteroscopic
IUM is a safe and effective technique for management
of menorrhagia secondary to submucosal fibroid.
Preliminary data suggest the technique to be as
safe and effective as, and less time-consuming
than, conventional techniques. Maximum benefit
would be achieved if submucosal fibroid cases
for IUM resection were carefully selected, with
particular reference to patients in whom >50% of the
fibroid protrudes into the uterine cavity and where
maximum diameter is ≤3 cm.
Declaration
No conflicts of interest were declared by authors.
References
1. Puri K, Famuyide AO, Erwin PJ, Stewart EA, Laughlin-Tommaso SK. Submucosal fibroids and the relation to
heavy menstrual bleeding and anemia. Am J Obstet
Gynecol 2014;210:38.e1-7. Crossref
2. Rubino RJ, Lukes AS. Twelve-month outcomes for patients
undergoing hysteroscopic morcellation of uterine polyps
and myomas in an office or ambulatory surgical center. J
Minim Invasive Gynecol 2015;22:285-90. Crossref
3. AlHilli MM, Nixon KE, Hopkins MR, Weaver AL,
Laughlin-Tommaso SK, Famuyide AO. Long-term
outcomes after intrauterine morcellation vs hysteroscopic
resection of endometrial polyps. J Minim Invasive Gynecol
2013;20:215-21. Crossref
4. Haber K, Hawkins E, Levie M, Chudnoff S. Hysteroscopic
morcellation: review of the manufacturer and user facility
device experience (MAUDE) database. J Minim Invasive
Gynecol 2015;22:110-4. Crossref
5. Wamsteker K, Emanuel MH, de Kruif JH. Transcervical
hysteroscopic resection of submucous fibroids for
abnormal uterine bleeding: results regarding the degree of
intramural extension. Obstet Gynecol 1993;8:736-40.
6. Stamatellos I, Apostolides A, Tantis A, Stamatopoulos P,
Bontis J. Fertility rates after hysteroscopic treatment of
submucous fibroids depending on their type. Gynecol Surg
2006;3:206-10. Crossref
7. Di Spiezio Sardo A, Mazzon I, Bramante S, et al.
Hysteroscopic myomectomy: a comprehensive review of
surgical techniques. Hum Reprod Update 2008;14:101-19. Crossref
8. Tarneja P, Tarneja VK, Duggal BS. Complications of
hysteroscopy surgery. Medical Journal Armed Forces India
2002;58:331-4. Crossref
9. Isaacson KB, Olive DL. Operative hysteroscopy in
physiologic distention media. J Am Assoc Gynecol Laparosc
1999;6:113-8. Crossref
10. AAGL Advancing Minimally Invasive Gynecology
Worldwide, Munro MG, Storz K, Abbott JA, et al. AAGL
Practice Report: Practice Guidelines for the Management of
Hysteroscopic Distending Media: (Replaces Hysteroscopic
Fluid Monitoring Guidelines. J Am Assoc Gynecol
Laparosc. 2000;7:167-168.). J Minim Invasive Gynecol
2013;20:137-48. Crossref
11. Hamerlynck TWO, Dietz V, Schoot BC. Clinical
implementation of the hysteroscopic morcellator for the
removal of intrauterine myomas and polyps. A retrospective
descriptive study. Gynecol Surg 2011;8:193-6. Crossref
12. Emanuel MH, Wamsteker K. The Intra Uterine
Morcellator: a new hysteroscopic operating technique to
remove intrauterine polyps and myomas. J Minim Invasive
Gynecol 2005;12:62-6. Crossref