Hong Kong Med J 2015 Dec;21(6):542–52 | Epub 6 Nov 2015
DOI: 10.12809/hkmj154691
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
REVIEW ARTICLE CME
Clinicopathological effects of pepper (oleoresin capsicum) spray
MF Yeung, MB, ChB, MRCP (UK)1;
William YM Tang, FRCP (Edin), FHKAM (Medicine)2
1 Department of Medicine and Geriatrics, Tuen Mun Hospital, Tuen Mun, Hong Kong
2 Private practice, Hong Kong
Corresponding author: Dr MF Yeung (wmfyeung@hotmail.com); (yeungmf1@ha.org.hk)
Abstract
Objectives: Pepper (oleoresin capsicum) spray is one of the most common riot-control measures used
today. Although not lethal, exposure of pepper spray can cause injury to different organ
systems. This review aimed to summarise the major
clinicopathological effects of pepper
spray in humans.
Data sources: MEDLINE, EMBASE database,
and Cochrane Database of Systematic Reviews
were used to search for terms associated with
the clinicopathological effects of pepper spray in
humans and those describing the pathophysiology
of capsaicin. A phone interview with two individuals
recently exposed to pepper spray was also conducted
to establish clinical symptoms.
Study selection: Major key words used for the
MEDLINE search were “pepper spray”, “OC spray”,
“oleoresin capsicum”; and other key words as “riot
control agents”, “capsaicin”, and “capsaicinoid”.
We then combined the key words “capsaicin” and
“capsaicinoid” with the major key words to narrow
down the number of articles. A search with other
databases including EMBASE and Cochrane
Database of Systematic Reviews was also conducted
with the above phrases to identify any additional
related articles.
Data extraction: All article searches were confined
to human study. The bibliography of articles was
screened for additional relevant studies including
non-indexed reports, and information from these
was also recorded. Non-English articles were
included in the search.
Data synthesis: Fifteen articles were considered
relevant. Oleoresin capsicum causes almost
instantaneous irritative symptoms to the skin,
eyes, and respiratory system. Dermatological
effects include a burning sensation, erythema,
and hyperalgesia. Ophthalmic effects involve
blepharospasm, conjunctivitis, peri-orbital oedema,
and corneal pathology. Following inhalation, a
stinging or burning sensation can be felt in the nose
with sore throat, chest tightness, or dyspnoea. The
major pathophysiology is neurogenic inflammation
caused by capsaicinoid in the pepper spray. There
is no antidote for oleoresin capsicum. Treatment
consists of thorough decontamination, symptom-directed
supportive measures, and early detection
and treatment of systemic toxicity. Decontamination
should be carefully carried out to avoid contamination
of the surrounding skin and clothing.
Conclusion: Pepper (oleoresin capsicum) spray is an
effective riot-control agent and does not cause life-threatening
clinical effects in the majority of exposed
individuals. Early decontamination minimises the
irritant effects.
Introduction
Pepper spray has been commonly employed for
decades by government agencies or military forces
worldwide as a non-lethal incapacitating agent
against interpersonal violence or civil unrest, and for
law enforcement, criminal incapacitation, personal
self-defence, and sometimes control of wild animals.
It was first used by Federal Bureau of Investigation
personnel in the US in 1973. It is usually used when
someone is under threat and wants to defend himself
from an attacker. It is also known as a riot-control
agent or harassing agent. Pepper spray is also used
by the Hong Kong Police Force. In this article, the
related clinicopathological effects of pepper spray
are discussed with a review of the medical literature.
Chemistry of oleoresin capsicum
The active ingredient in pepper spray is oleoresin
capsicum (OC), an oily concentrated extract from
pepper plants of the genus Capsicum, commonly
referred as chilli pepper (Capsicum annuum).
For centuries, people have used pepper extracts
to prepare spicy foods. Other uses include
neurobiological research, local anaesthesia, and
the production of self-defence products. Oleoresin
capsicum comprises a group of fat-soluble pungent
chemical phenols described as ‘capsaicinoids’.
There are five naturally occurring capsaicinoids:
capsaicin, dihydrocapsaicin, nordihydrocapsaicin,
homocapsaicin, and homodihydrocapsaicin. The
most pungent capsaicinoid analogues are capsaicin
(trans-8-methyl-N-vanillyl-6-nonenamide,
C18H27NO3 with molecular weight of 305.4) and
dihydrocapsaicin: together they constitute 80%
to 90% of the total concentration in pepper spray
products.1 2 The absolute and relative abundance of
each capsaicinoid analogue varies in fresh peppers
and OC spray products. Nonivamide, or ‘synthetic’
capsaicin, exhibits the same pungency as capsaicin.3
Methods
A literature review was conducted using the
MEDLINE database (from 1946 to present), and
major key words of “pepper spray”, “OC spray”,
“oleoresin capsicum” and other key words of “riot
control agents”, “capsaicin”, and “capsaicinoid”.
We then combined the key words “capsaicin” and
“capsaicinoid” with the major key words to narrow
down the number of articles. All article searches
were limited to human study. Search with other
databases including EMBASE and Cochrane
Database of Systematic Reviews was also conducted
with the above phrases to look for any additional
related articles. The bibliography of relevant
articles was screened for additional relevant studies
including non-indexed reports. Non-English articles
were included in the search. Phone interview was
conducted with individuals recently exposed to
pepper spray in Hong Kong to obtain information
about exposure history and symptomatology.
Results
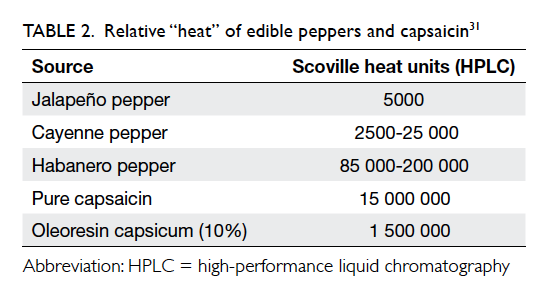
A total of 111 articles were identified of which 15
were considered relevant to our review. The details
are summarised in Table 1.4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Our search identified 10 studies published formally in peer-reviewed
medical and scientific journals that addressed the
clinicopathological effects of OC spray in humans.
The remaining five papers were case reports of the
clinical effects of OC spray on a particular organ
system.
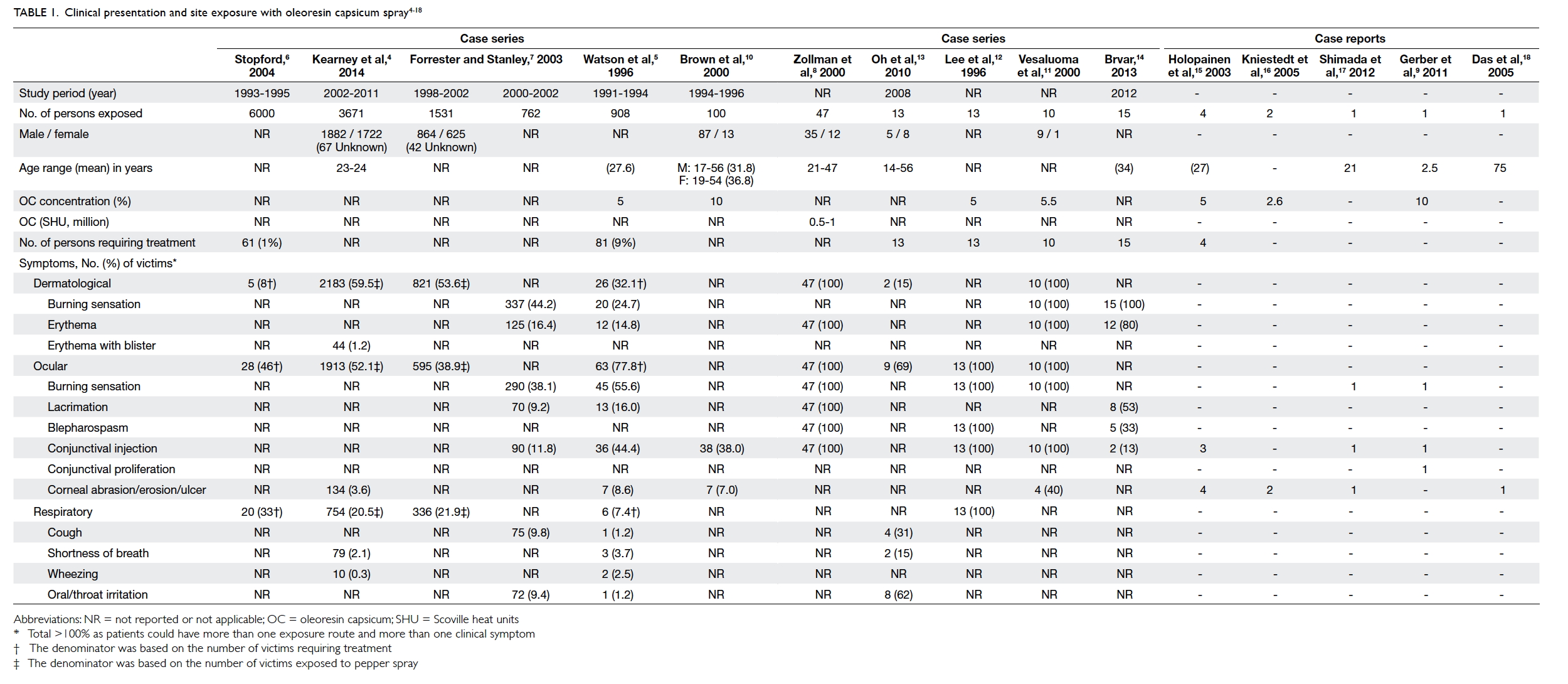
Table 1. Clinical presentation and site exposure with oleoresin capsicum spray4 5 6 7 8 9 10 11 12 13 14 15 16 17 18
One of the authors (MF Yeung) conducted a
telephone interview with two pepper spray victims.
One 22-year-old man sustained direct lateral spray
to his neck and forearm from a distance of 1 to 2 m.
He experienced an almost immediate burning
sensation over the sprayed areas, described as a very
strong mint feeling. He then flushed himself with
water but the chemical contaminated his clothes and
other skin areas resulting in persistent burning pain
for 30 minutes. Pain gradually resolved after an hour.
Another 29-year-old woman sustained spray to her
arm and forearm from a distance of approximately
5 m. Immediately she experienced a severe burning
sensation over the affected areas (Fig 1), described as touching chilli seeds. She irrigated herself with
water in the public toilet. The upper chest was also
involved due to contamination of her clothing.
Following irrigation, pain reduced over the next few
hours to a mild hot sensation but still continued. She
took a bath with warm water and baby shampoo 3
hours after exposure but experienced increased pain
over the sprayed area. The pain resolved completely
around 5 hours post-exposure.

Figure 1. Dermatitis in the affected area 4 hours following exposure
(Reproduced with permission of Miss YY Tse)
Clinical features
Exposure to OC can be via direct contact with
skin, eyes or mucous membranes, or as a result of
inhalation or ingestion. The irritant effects result
in almost instantaneous onset of symptoms: within
seconds it can induce a burning sensation on
skin, involuntary closure of eyes, and diminished
hand-eye coordination. Victims are usually rapidly
incapacitated although most symptoms resolve
within 30 to 60 minutes. The use of pepper spray by
the US police has been reported to be successful in
subduing aggressive individuals in 90% of cases.19
Dermatological injury
Initial contact of capsaicin with skin or mucous
membranes produces a violent irritation with
subsequent desensitisation to irritant chemicals.
Victims experience acute burning pain, tingling,
erythema, oedema, and pruritus (the pain can be
prolonged for several hours in persons not adequately
decontaminated).4 20 In prolonged exposure and
in severe cases, persistent dermatitis with severe
erythema and/or blister formation may occur.4 20
Kearney et al4 made a retrospective chart
review of all human exposures to pepper spray
recorded in the electronic database of the California
Poison Control System during 2002-2011 (Table 1). Of the 3671 victims recorded, the most common
type of exposure was dermal (2183 victims, 59.5%)
with 2080 (56.7%) victims reporting minor/self-limiting
symptoms, and 103 (2.8%) reporting more
severe symptoms that required medical evaluation,
including persistent dermatitis, dermal burns, and/or blister formation.
Watson et al5 conducted a retrospective study
based on medical record review of 81 patients
who presented to an emergency department after
exposure to OC (908 individuals in total exposed
during law enforcement) in 1991 to 1994 in Kansas
City, Missouri, US. In 26 (32.1%) cases the chief
symptoms upon arrival to casualty were pain or
a burning sensation in exposed skin. In the US, a
retrospective case review of approximately 6000
officers was conducted at the Department of
Corrections; these officers were exposed to pepper
spray during training in 1993 to 1995.6 21 Only 61 (1%) required medical treatment: five (8%) complained of
dermatological symptoms of whom two had hives.
Forrester and Stanley7 used data derived from
telephone calls to the Texas Poison Center Network
to investigate the epidemiology of OC exposure.
Of 762 human exposures during 2000 to 2002, 337
(44.2%) experienced dermal irritation/pain and 125
(16.4%) had erythema on exposed skin.
Ophthalmic injury
Contact of the eye with OC causes redness, swelling,
severe burning pain, tingling, lacrimation, and
involuntary or reflex closing of the eyelids. More
severe symptoms include persistent pain, foreign
body sensation, photophobia, discharge or exudate,
or peri-orbital oedema. Zollman et al8 showed that in
police cadet volunteers sprayed in the face with OC,
the most significant symptoms were conjunctival
and scleral irritation and blepharospasm.
Symptoms usually resolved within 1.5 to 2 hours of
decontamination although mild chemosis, corneal
oedema, or hyphaema could persist.
Conjunctival proliferation has been reported
in a young child following mild spray injury and was
refractory to steroid therapy with subsequent need
for surgical excision.9 Decreased tear production
as evidenced by a lower Schirmer test score was found. An
impaired corneal reflex lacrimation and corneal
blink reflex have also been observed.22
Oleoresin capsicum spray can affect both
morphology and sensitivity of the cornea. Brown et
al10 demonstrated that of 100 exposed individuals
(10% OC spray), 7% (n=7) had corneal abrasion. Watson et al5 found 8.6% (n=7) of 81 affected officers who required medical treatment actually had corneal
abrasion. Epstein and Majmudar23 described a case with keratopathy, and the victim’s eye showed a corneal epithelial defect
after OC spray to the eyes. Although the defects
healed within 5 days of treatment with polymyxin-bacitracin
ophthalmic ointment, smouldering
inflammation persisted. Further treatment with
tobramycin-dexamethasone drops every 4 hours
caused the inflammation to subside but superficial
stromal opacity remained, resulting in irregular
astigmatism.23
Zollman et al8 demonstrated that corneal
sensation was severely affected after 10 minutes and
1 hour of exposure. At 1 week, sensation returned
to baseline and corneal abnormalities disappeared.
Apart from capsaicin, the carrier vehicle in which
the active ingredient is dissolved may be toxic to
corneal epithelial cells and cause temporary ocular
irritation or superficial keratitis or erosion.12
Oral, nasal, and respiratory toxicity
Exposure may occur through inhalation, causing
immediate inflammation of mucous membranes.
Throat irritation results in a burning sensation,
cough, choking, and inability to speak (due to
laryngospasm or laryngeal paralysis). In the
nasal mucosa, OC produces irritation, burning
pain, sneezing, and a dose-dependent serous
discharge.24 Other respiratory symptoms have also
been reported, including severe coughing, mucus
secretion, shortness of breath, bronchoconstriction
presenting as wheeze, and chest tightness. Direct
contact of capsaicinoids with the vocal cords causes
laryngospasm lasting 45 seconds.21 Duration or
magnitude of bronchoconstriction did not differ
among normal subjects, smokers, and asthmatics.21
A review by Watson et al5 of 81 victims of law
enforcement action revealed that 7.4% (n=6) had
respiratory symptoms after inhalation of OC spray,
and 3.7% (n=3) complained of shortness of breath.
Oh et al13 studied an incident of OC gas leak in an
urban shopping mall that affected 13 victims, of
whom two (15%) experienced shortness of breath
and eight (62%) complained of oral/throat irritation.
A controlled clinical trial involving 35 healthy
subjects exposed to OC spray did not detect
significant changes in predicted forced expiratory
volume in 1 second (FEV1) or oxygen saturation
when compared with population norms.25 The
prone maximum restraint position reduced forced
vital capacity (FVC) and FEV1 by 15% compared
with a sitting position, but there was no statistically
significant difference in these parameters when use
of OC and controls were compared in the restraint
position.25
Systemic toxicity and death
Inhalation of OC spray can cause laryngeal and
pulmonary oedema and chemical pneumonitis but
this is rare.21 An 11-year-old child who directly
inhaled a jet spray from a pressurised container
ultimately recovered but was reported to develop
subglottic obstruction of the trachea and bilateral
pulmonary infiltration that required intubation.26
Billmire et al27 described a 4-week-old healthy
infant exposed to 5% OC when a self-defence device
was accidentally discharged; the infant developed
respiratory failure and hypoxaemia requiring
extracorporeal membrane oxygenation. The patient
was discharged and 12-month follow-up revealed
several episodes of viral respiratory infections.27
Some studies have reported systemic
symptoms including disorientation, fear, loss of
body motor control (eg diminished hand-eye
coordination),28 hyperventilation, tachycardia, and
pulmonary oedema.21 The acute increase in blood
pressure could cause headache, increased stroke risk
and heart attack.21 In a review of approximately 6000
(police) officers directly exposed to OC, eight (0.1%)
trainees reported headache and chest problems that
persisted for more than 1 week.6
Since 1993, over 70 in-custody deaths have
involved the use of OC spray during the arrest
process.29 At the same time, Amnesty International
has claimed that since the early 1990s more than 100
people in the US have died following exposure to
pepper spray.30 Steffee et al31 reported an in-custody death in a known asthmatic who had been sprayed
10 to 15 times with OC spray (Table 2). O’Halloran and Frank29 reported 21 cases of restraint in-custody
death, of which 10 were preceded by use of OC spray. Granfield et al32 reported 30 cases of
in-custody death following OC exposure in the US
but this review concluded that pepper spray was not
the cause of death in any of the cases. Pollanen et
al33 reported 21 in-custody restraint deaths in which
four of the subjects had been sprayed with OC.
Details are shown in Table 3.29 31 32 33
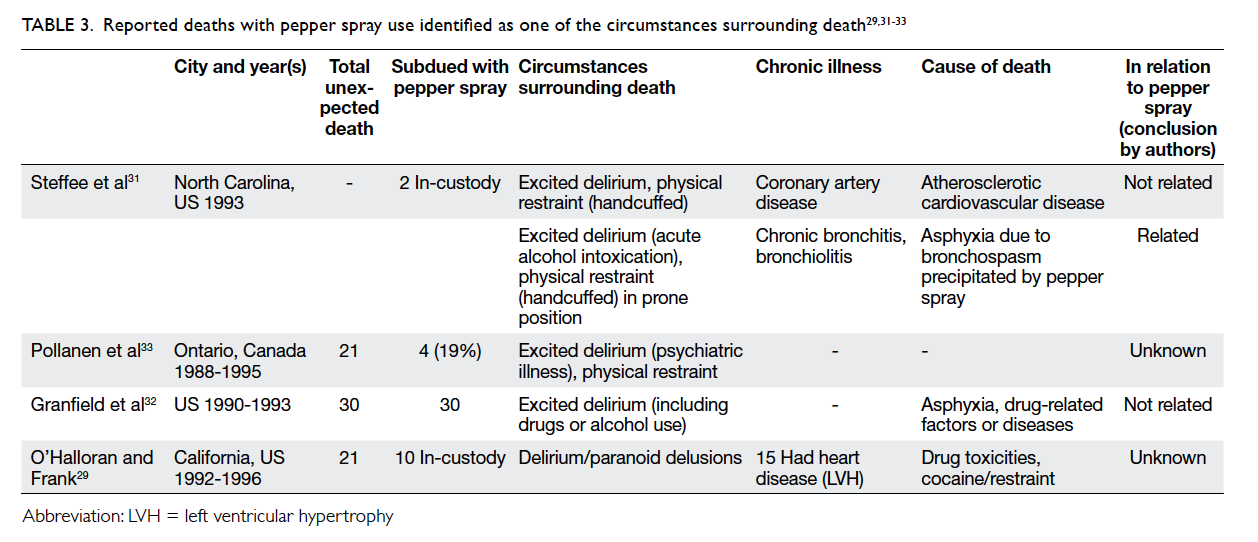
Table 3. Reported deaths with pepper spray use identified as one of the circumstances surrounding death29 31 32 33
Decontamination
The pre-hospital management of an individual
exposed to pepper spray should include prompt on-scene
removal of exposure to reduce the source of
irritation. First, victims should move away from any
continuing source of exposure. The presence of any
signs or symptoms of serious systemic distress such
as cardiovascular or respiratory problems should
be ascertained.13 The immediate and most readily
available method of decontamination at the scene of
exposure is likely to be water. The affected skin and
mucous membranes should be irrigated thoroughly
with copious amounts of cool water to help soothe
the burning sensation and flush away any spray
residue.12
Some authors suggest that eyes exposed to OC
should be irrigated with copious amounts of room-temperature
water or normal saline for at least 15
minutes.4 If the victim is wearing contact lenses, they
should be removed as quickly as possible.12 Washing
the eyelids with a mild, oil-free soap will help break
down the OC resin and speed up its removal.12 If
a high level of spray residue is present in clothing,
it should be removed and placed in sealed plastic
bags until it can be cleaned or discarded.12 Removal
of contaminated clothing will aid in preventing
secondary contamination. Contamination by used
towels should be avoided.12 Showering with soap and
water is advised to remove the irritant from skin that
should be blotted dry, not rubbed.12
For acute relief of burning dermal pain,
one study suggested application of magnesium-aluminium
hydroxide suspension.34 Vegetable oil
immersion and vinegar have been reported to
be more effective than water in relief of burning
sensation.35 36 One study of 49 volunteer adult law
enforcement trainees exposed to OC during a routine
training exercise, who were randomised to one of five
treatment groups (aluminium hydroxide–magnesium
hydroxide, 2% lidocaine gel, baby shampoo, milk,
or water), reported no significant difference in pain
relief. Time after exposure appeared to be the best
predictor for decrease in pain.37 Medical treatment
for dermatitis may include topical steroids, oral
antihistamines, and topical antibiotics.
Discussion
Pepper sprays are generally regarded as immediately
effective and less toxic than other riot-control
agents such as chloroacetophenone (CN) and o-chlorobenzylidene
malononitrile (CS). Both CN and
CS are effective lacrimating agents with CN the most
lethal. The estimated lethal dose (LCt50) of CN, CS,
and OC is 8500, 25 000 and >100 000 mg/min/m3,
respectively.38
Oleoresin capsicum spray contains the active
ingredient capsaicin, which is obtained from chilli
pepper. Typically, pepper spray weapons contain
a 10% to 20% solution of OC. The capsaicinoid
content determines the ‘hotness’ of preparation,
commonly referred to as Scoville Heat Unit (SHU;
Table 2). The scale is named after its creator, American pharmacist Wilbur Scoville. Sprays
used in police work typically fall between 0.5 and
2 million SHUs.8 The SHU governs the efficacy
and pungency of pepper spray, thus the higher the
SHU, the greater the inflammatory effect on skin
and mucous membranes. A higher concentration
of OC lengthens the necessary recovery period,
thus affecting decontamination.39 Greater than 5%
OC might not atomise well into a fine spray (may
clog the aerosol spray).40 The capsaicin and related
capsaicinoid content in most law enforcement OC
sprays is between 1.3% and 2%. Areas of exposure
can be dermatological, ocular, inhalational, ingestion
or mixed, thus symptoms often involve more than
one system. The prevalence of severe symptoms
observed in various epidemiological studies varies
from 2.7% to 15%.4 5 7 10
We found dermatological manifestation as
the most common symptom in the case series
(32%-100%),5 8 11 although another study reported dermatological symptoms in only 8% of cadet officers
exposed to OC.6 The predominant site of exposure
will be affected by any protective measures adopted:
use of protective goggles or shields will greatly
diminish exposure of skin to OC. Circumstances
of OC spray use will also affect the predominant
sites of exposure and severity of symptoms. Faced
with confrontation during a public demonstration,
officers will target OC spray at the eyes of protestors
to quickly incapacitate them. This will result in a
greater degree of both dermatological (face) and
ocular exposure. Kearney et al4 analysed the risk
factors with the largest independent associations
with more severe symptoms among 3671 cases
exposed to direct OC spray designed to incapacitate
during law enforcement crowd-control activities.
Multiple exposure of skin or mucous membranes
over a period of seconds or minutes exaggerate
the inflammatory response. Capsaicin exposure may
diminish sensitivity to heat- or chemical-induced
pain, and thus increase the risk and severity of
dermal burns. Some authors have suggested that
capsaicin can powerfully stimulate heat receptors
to cause reflex sweating and vasodilatation, and
activate hypothalamus-mediated cooling; this may
result in an increased risk of hypothermia if victims
are decontaminated with cold water on cold days.41 42
Further, capsaicin-related cutaneous sensation may
be heightened by perspiration, lacrimation, high
humidity, and bathing at a warm temperature.43
The dermatological effects of capsaicin in OC
spray have been further described in some case
reports. ‘Hunan hand’ syndrome describes painful
contact dermatitis in people preparing chilli peppers
(containing capsaicin) by direct handling,44 while
Sweet’s syndrome has been described following
exposure to jalapeño peppers.45
Respiratory effects of OC spray involve cough
reflex stimulation via capsaicin-sensitive nerves
and bronchoconstriction. Although OC spray
exposure causes cough and transient increase in
airway resistance, experimental studies and clinical
case reports show no evidence that patients with
bronchial hypersensitivity are any more susceptible
to the irritant effects of OC spray than those without.5
No cases of occupational asthma due to capsaicin
have been reported.21 A cross-sectional study of
workers exposed to capsaicin detected a statistically
significant increase in complaints of cough in
capsaicin-exposed workers, although there was no
significant difference in FEV1 and FVC between the
two groups.46 Not all asthmatics are sensitive to the
bronchoconstrictive effects of OC spray.21
As capsaicinoids are lipophilic and have
limited water solubility (16 µg/mL),47 alcohols or
other organic solvents are commonly used as a
base to facilitate aerosolisation in pepper spray
products. Suitable solvents include methylene
chloride, isopropanol, propylene glycol, ethanol,
and methanol. The solvent enhances capsaicinoid
solubility to enable delivery to the intended target
tissue. A gaseous propellant (usually nitrogen or
carbon dioxide) is incorporated in the spray to
discharge the canister contents.1 Inhalation of high
doses of some of these chemicals may produce
adverse cardiac, respiratory, and neurological
effects, including arrhythmia.21 The health effects of
solvent and propellants are beyond the scope of our
study, but their potential hazards and effects need to
be considered.
Little is known about the long-term effects of
pepper spray. Concern has been raised about their
mutagenic and carcinogenic effects considering
the organic solvent content, but the findings of
numerous studies are inconclusive. Genotoxic effects
have been demonstrated for capsaicin, but usually in
cultured cells and at micromolar concentrations.48
These levels would not normally be achieved in field
use. Some authors suggest that single or incidental
relatively low doses of OC spray, as used by the
police, will not produce a significant cancer risk.19
Nonetheless the long-term risks for those sprayed
on multiple occasions are unknown.21
In the cases of fatality that we identified, a
causal connection between OC spray exposure and
death remained controversial. A number of deaths in
custody occurred after exposure to pepper spray but
the cause was not thoroughly investigated. In a report
by Steffee et al,31 autopsy findings and toxicology
results were analysed alongside pre-mortem chain
of events, symptomatology, and degree of natural
disease process. One asthmatic victim died because
of severe acute bronchospasm, probably precipitated
by the use of OC spray.31 Another review of various
fatalities49 found that positional asphyxia (subjects
are placed prone, typically handcuffed behind
the back, hog-tied, and breathing becomes more
difficult), drugs (alcohol intoxication, excited
delirium [cocaine-induced], methamphetamine),
pre-existing respiratory or cardiovascular disease,
obesity and other conditions caused or contributed
to almost all deaths.21 Exposure to OC spray was not
judged to be a precipitating factor in any of these
cases.50 Some authors have concluded that OC spray
is not inherently lethal or dangerous.51 From the
literature search, most cases of death associated with
the use of pepper spray involved other factors and
there was no convincing evidence that OC spray was
implicated.
Although OC is lipophilic and many substances
have been recommended for decontamination,
water is easily available and of no harm. In the
presence of ocular exposure, it is helpful to irrigate
the upper and lower palpebral cul-de-sac because
spray residue tends to collect in these locations and
becomes entrapped.12 In one individual whose eyes
were exposed to OC, the best-corrected visual acuity
with spectacles did not improve beyond 20/40 after 7
months because of irregular astigmatism associated
with persistent corneal opacity.23 Therefore prompt
ocular irrigation is important to avoid potentially
permanent ocular sequelae.
The severity of health effects from pepper
spray exposure may be contingent on several
product-, dispersal-, and patient-related factors.
Various handheld pressurised canisters of OC
spray are available and at least three variables affect
their overall effectiveness. The first is the type,
level of ‘hotness’, or concentration of pepper spray.
Since the concentration of extract in pepper sprays
varies (5%-15%), the potential risks associated
with capsaicinoid exposure may vary up to 30-fold
among different brands of OC spray.21 Second, the
physiochemical properties of the solvent, that is, the
vehicle type and its chemical solubility, can influence
skin bioavailability.52 It increases the effectiveness of
spray by improving penetration, removing skin oils,
or prolonging contact time.12 Lastly, the delivery
device or propellant—liquid spray, powder, or
aerosolisation—dictates particle size and penetration
into mucosal membranes and airways.
The severity of injury also depends on the
circumstances of exposure. Direct exposure may
be accidental or intentional.4 The latter involves a
higher-risk situation that might require long OC
application and tactics with consequent higher
potential for injury. Concurrent disease and health
of victims, varying doses, and distance being
sprayed also determine different degrees of toxicity.
Environmental conditions (windy, rainy weather),
and crowd size and characteristics should also be
taken into account when assessing level of exposure.
Eyeglasses, sunglasses, and other protective eyewear
and clothing can greatly reduce the effectiveness of
OC sprays, as can the behaviour of the victim. For
example, raising the hands in a defensive measure
may block the spray.39 This was exemplified by the
use of goggles and umbrellas at recent altercations
with police reinforcement in Hong Kong.
Neurogenic inflammation
Capsaicin-induced neurogenic inflammation (Fig 221 53) is associated with heat allodynia (decreased heat pain threshold), thermal and mechanical
hyperalgesia and cold hypoesthesia at the site of
challenge.54 Neurophysiological study has demonstrated
increased contact heat pain and shortened
latencies of contact heat-evoked potentials following
capsaicin-induced heat hyperalgesia.55 It is possible
that capsaicin causes a decrease in the A-delta-fibre
threshold giving rise to heat allodynia.55 Therefore,
the ongoing pain and discharges of the sensitised
nociceptors following capsaicin sensitisation depend
on skin surface temperature: mild cooling of skin
results in reduction of the burning pain sensation.55
This is why Lee et al12 suggested that during the
decontamination process, allowing fresh air to
circulate or even fanning the exposed area could
assist in recovery. Cool water soothes the burning
sensation while hot water increases it.
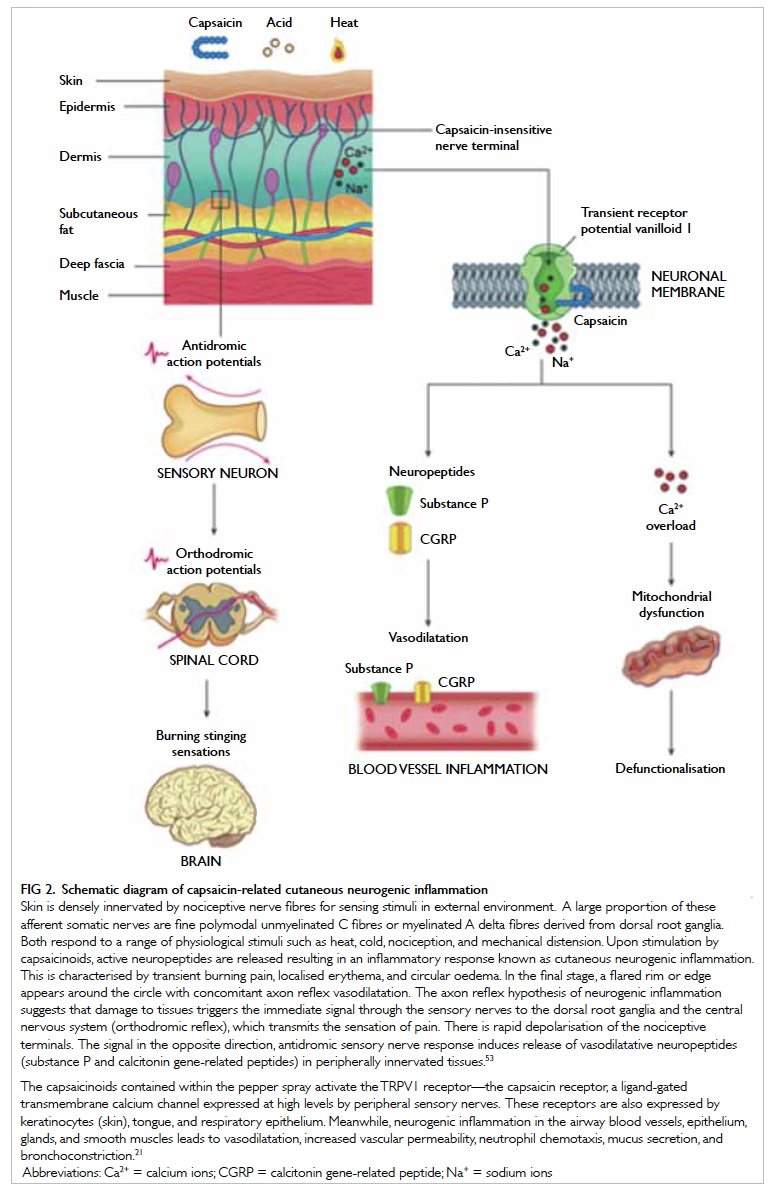
Figure 2. Schematic diagram of capsaicin-related cutaneous neurogenic inflammation
Skin is densely innervated by nociceptive nerve fibres for sensing stimuli in external environment. A large proportion of these afferent somatic nerves are fine polymodal unmyelinated C fibres or myelinated A delta fibres derived from dorsal root ganglia. Both respond to a range of physiological stimuli such as heat, cold, nociception, and mechanical distension. Upon stimulation by capsaicinoids, active neuropeptides are released resulting in an inflammatory response known as cutaneous neurogenic inflammation. This is characterised by transient burning pain, localised erythema, and circular oedema. In the final stage, a flared rim or edge appears around the circle with concomitant axon reflex vasodilatation. The axon reflex hypothesis of neurogenic inflammation suggests that damage to tissues triggers the immediate signal through the sensory nerves to the dorsal root ganglia and the central nervous system (orthodromic reflex), which transmits the sensation of pain. There is rapid depolarisation of the nociceptive terminals. The signal in the opposite direction, antidromic sensory nerve response induces release of vasodilatative neuropeptides (substance P and calcitonin gene-related peptides) in peripherally innervated tissues.53
The capsaicinoids contained within the pepper spray activate the TRPV1 receptor—the capsaicin receptor, a ligand-gated transmembrane calcium channel expressed at high levels by peripheral sensory nerves. These receptors are also expressed by keratinocytes (skin), tongue, and respiratory epithelium. Meanwhile, neurogenic inflammation in the airway blood vessels, epithelium, glands, and smooth muscles leads to vasodilatation, increased vascular permeability, neutrophil chemotaxis, mucus secretion, and bronchoconstriction.21
Pharmacological use
While our review focuses on OC spray, the most active
ingredient capsaicin can be used therapeutically
at an appropriate dilution. Prolonged topical
application of capsaicin has been shown to induce a
localised reversible loss of >60% of nociceptive nerve
fibre terminals in the epidermis and dermis56 and
attenuate heat pain sensitivity (defunctionalisation
of TRPV1-expressing nociceptive fibres), resulting
in relief in peripheral neuropathic pain syndromes.57
Limitations
There are limited large-scale case studies in the
English literature of the clinicopathological effects
of OC spray exposure. In some case series, data
were reviewed retrospectively (from poison control
centre registries) and may not have been collected
using a standardised format, including exposure
circumstances, thus some data might be missing.
There was little information about the exact method,
effectiveness, and precise timing of decontamination
procedures or other interventions. Data on the
concentration and especially SHU of OC spray,
which could affect the strength and efficacy of spray
to produce injury, were largely lacking, including
particle size of OC spray and dose administered.
The circumstances of exposure (riot control, crowd
control, police cadet training, or domestic) and the
scale of canister (distance of spray jet) would have
affected the severity of clinicopathological effects of
OC spray but were not recorded in detail. As most
studies were observational or retrospective, a definite
causal relationship between exposure and symptoms
could not be drawn. There are likely variables and
confounders present. In some studies, the reporting
of symptoms was largely voluntary and thus likely
to be biased. Most studies did not address chronic
toxicity or residual disability in people exposed to
OC spray.
Conclusion
Based on our review, OC spray appears to be
an effective incapacitating riot-control agent.
Significant adverse clinical effects or life-threatening
conditions are not anticipated in the majority of
exposures and death caused by OC spray exposure
is unlikely. Dermatological and ophthalmic effects
are commonly seen after exposure to OC spray in
humans due to neurogenic inflammation. Careful
early decontamination can minimise the irritant
effects. Victims should be monitored for any
evidence of serious adverse effects, with prompt
medical intervention for any life-threatening
symptoms. Large prospective cohort studies or case-control
studies would strengthen the ability to infer
a causal relationship between pepper spray exposure
and health outcome.
References
1. Reilly CA, Crouch DJ, Yost GS. Quantitative analysis of
capsaicinoids in fresh peppers, oleoresin capsicum and
pepper spray products. J Forensic Sci 2001;46:502-9. Crossref
2. Reilly CA, Crouch DJ, Yost GS, Fatah AA. Determination
of capsaicin, dihydrocapsaicin, and nonivamide in
self-defense weapons by liquid chromatography–mass
spectrometry and liquid chromatography–tandem mass
spectrometry. J Chromatogr A 2001;912:259-67. Crossref
3. Cordell GA, Araujo OE. Capsaicin: identification,
nomenclature, and pharmacotherapy. Ann Pharmacother
1993;27:330-6.
4. Kearney T, Hiatt P, Birdsall E, Smollin C. Pepper spray
injury severity: ten-year case experience of a poison control
system. Prehosp Emerg Care 2014;18:381-6. Crossref
5. Watson WA, Stremel KR, Westdorp EJ. Oleoresin
capsicum (Cap-Stun) toxicity from aerosol exposure. Ann
Pharmacother 1996;30:733-5.
6. Stopford W. Occupational exposures to riot control agents.
In: Olajos EJ, Stopford W, editors. Riot control agents. Issues in
toxicology, safety and health. New York: CRC Press; 2004:
277. Crossref
7. Forrester MB, Stanley SK. The epidemiology of pepper
spray exposures reported in Texas in 1998-2002. Vet Hum
Toxicol 2003;45:327-30.
8. Zollman TM, Bragg RM, Harrison DA. Clinical effects of
oleoresin capsicum (pepper spray) on the human cornea
and conjunctiva. Ophthalmology 2000;107:2186-9. Crossref
9. Gerber S, Frueh BE, Tappeiner C. Conjunctival proliferation
after a mild pepper spray injury in a young child. Cornea
2011;30:1042-4. Crossref
10. Brown L, Takeuchi D, Challoner K. Corneal abrasions
associated with pepper spray exposure. Am J Emerg Med
2000;18:271-2. Crossref
11. Vesaluoma M, Müller L, Gallar J, et al. Effects of oleoresin
capsicum pepper spray on human corneal morphology and
sensitivity. Invest Ophthalmol Vis Sci 2000;41:2138-47.
12. Lee RJ, Yolton RL, Yolton DP, Schnider C, Janin ML.
Personal defense sprays: Effects and management of
exposure. J Am Optom Assoc 1996;67:548-60.
13. Oh JJ, Yong R, Ponampalam R, Anantharman V, Lim SH.
Mass casualty incident involving pepper spray exposure:
impact on the emergency department and management of
casualties. Hong Kong J Emerg Med 2010;17:325-9.
14. Brvar M. Pepper spray (capsaicin) exposure:
decontamination with amphoteric, chelating and
hypertonic solution [abstract]. Clin Toxicol 2013;51:314.
15. Holopainen JM, Moilanen JA, Hack T, Tervo TM. Toxic
carriers in pepper sprays may cause corneal erosion.
Toxicol Appl Pharmacol 2003;186:155-62. Crossref
16. Kniestedt C, Fleischhauer J, Stürmer J, Thiel MA. Pepper
spray injuries of the anterior segment of the eye [in
German]. Klin Monbl Augenheilkd 2005;222:267-70. Crossref
17. Shimada M, Young C, Tanen DA. Corneal ulcer associated
with pepper spray exposure during military training. J
Emerg Med 2012;43:e149. Crossref
18. Das S, Chohan A, Snibson GR, Taylor HR. Capsicum spray
injury of the eye. Int Ophthalmol 2005;26:171-3. Crossref
19. Busker RM, van Helden HP. Toxicologic evaluation of
pepper spray as a possible weapon for the Dutch police
force: risk assessment and efficacy. Am J Forensic Med
Pathol 1998;19:309-16. Crossref
20. Broadstock M. What is the safety of ‘pepper spray’ use
by law enforcement or mental health service staff? New
Zealand Health Technology Assessment Tech Brief Series.
Available from: http://nzhta.chmeds.ac.nz/publications/pepper_spray.pdf. Accessed Oct 2015.
21. Smith CG, Stopford W. Health hazards of pepper spray.
Available from: http://duketox.mc.duke.edu/pepper%20spray.pdf. Accessed 1 Dec 2014.
22. Rasier R, Kukner AS, Sengul EA, Yalcin NG, Temizsoylu O,
Bahcecioglu HO. The decrease in aqueous tear production
associated with pepper spray. Curr Eye Res 2015;40:429-33. Crossref
23. Epstein RJ, Majmudar PA. Pepper spray in the eye.
Ophthalmology 2001;108:1712-3. Crossref
24. Geppetti P, Fusco BM, Marabini S, Maggi CA, Fanciullacci
M, Sicuteri F. Secretion, pain and sneezing induced by the
application of capsaicin to the nasal mucosa in man. Br J
Pharmacol 1988;93:509-14. Crossref
25. Chan TC, Vilke GM, Clausen J, et al. The effect of oleoresin
capsicum “pepper” spray inhalation on respiratory
function. J Forensic Sci 2002;47:299-304. Crossref
26. Winograd HL. Acute croup in an older child. An unusual
toxic origin. Clin Pediatr (Phila) 1977;16:884-7. Crossref
27. Billmire DF, Vinocur C, Ginda M, et al. Pepper-spray–induced
respiratory failure treated with extracorporeal
membrane oxygenation. Pediatrics 1996;98:961-3.
28. Smith J, Greaves I. The use of chemical incapacitant sprays:
a review. J Trauma 2002;52:595-600. Crossref
29. O’Halloran RL, Frank JG. Asphyxial death during prone
restraint revisited: a report of 21 cases. Am J Forensic Med
Pathol 2000;21:39-52. Crossref
30. USA: Excessive and lethal force? Amnesty International’s
concerns about deaths and ill-treatment involving police
use of Tasers. Available from: http://www.amnestyusa.org/node/55449?page=72. Accessed 7 Dec 2014.
31. Steffee CH, Lantz PE, Flannagan LM, Thompson RL, Jason
DR. Oleoresin capsicum (pepper) spray and “in-custody
deaths.” Am J Forensic Med Pathol 1995;16:185-92. Crossref
32. Granfield J, Onnen J, Petty CS. Pepper spray and in-custody
deaths: international association of chiefs of police
executive brief. RCMP Gazette 1994;56:12-7.
33. Pollanen MS, Chiasson DA, Cairns JT, Young JG.
Unexpected death related to restraint for excited delirium:
a retrospective study of deaths in police custody and in the
community. CMAJ 1998;158:1603-7.
34. Lee DC, Ryan JR. Magnesium-aluminum hydroxide
suspension for the treatment of dermal capsaicin
exposures. Acad Emerg Med 2003;10:688-90. Crossref
35. Jones L, Tandberg D, Troutman WG. A controlled
evaluation for household treatments for “chile burns”. Vet
Hum Toxicol 1986;28:486.
36. Vogl TP. Treatment of Hunan hand. N Engl J Med
1982;306:178. Crossref
37. Barry JD, Hennessy R, McManus JG Jr. A randomized
controlled trial comparing treatment regimens for acute
pain for topical oleoresin capsaicin (pepper spray) exposure
in adult volunteers. Prehosp Emerg Care 2008;12:432-7. Crossref
38. Schep LJ, Slaughter RJ, McBride DI. Riot control agents:
the tear gases CN, CS and OC—a medical review. J R Army
Med Corps 2015;161:94-9. Crossref
39. Adkins LD. Oleoresin capsicum: an analysis of the
implementation of pepper spray into the law enforcement
use of force continuum in a selected police department.
Available from: http://dc.etsu.edu/etd/779. Accessed 23
Jan 2015.
40. National Institute of Justice. Oleoresin capsicum: pepper
spray as a force alternative. Available from: https://www.ncjrs.gov/pdffiles1/nij/grants/181655.pdf. Accessed 23 Jan
2015.
41. Tominack RL, Spyker DA. Capsicum and capsaicin—a
review: case report of the use of hot peppers in child abuse.
J Toxicol Clin Toxicol 1987;25:591-601. Crossref
42. Monsereenusorn Y, Kongsamut S, Pezalla PD. Capsaicin—a
literature survey. Crit Rev Toxicol 1982;10:321-39. Crossref
43. Hilmas CJ, Poole MJ, Katos AM, Williams PT. Chapter
12: Riot control agents. In: Handbook of toxicology of
chemical warfare agents. Available from: http://www.dtic.mil/dtic/tr/fulltext/u2/a539686.pdf. Accessed Oct 2015.
44. Weinberg RB. Hunan hand. N Engl J Med 1981;305:1020. Crossref
45. Greer JM, Rosen T, Tschen JA. Sweet’s syndrome with an
exogenous cause. Cutis 1993;51:112-4.
46. Blanc P, Liu D, Juarez C, Boushey HA. Cough in hot pepper
workers. Chest 1991;99:27-32. Crossref
47. Kasting GB. Kinetics of finite dose absorption through skin
1. Vanillylnonanamide. J Pharm Sci 2001;90:202-12. CrossRef
48. Durnford JM. Chapter 10: Genetic toxicity of riot control agents. In: Olajos EJ, Stopford W, editors. Riot control agents. Issues in
toxicology, safety and health. New York: CRC Press; 2004: 183-200. Crossref
49. The American Civil Liberties Union of Southern California.
Pepper spray update: more fatalities, more questions; 1995
Jun. Available from: https://www.aclusocal.org/issues/police-practices/pepper-spray/. Accessed 19 Nov 2014.
50. International Association of Chiefs of Police. Pepper spray
evaluation project; 1995 Jun 22. Available from: http://www.theiacp.org/portals/0/pdfs/IntroPepperSpray.pdf.
Accessed 19 Nov 2014.
51. Christensen RG, Frank DE. Preliminary investigation of
oleoresin capsicum. National Institute of Justice Report
100-95, Gaithersburg, MD: National Institute of Standards
and Technology; 1995.
52. Pershing LK, Corlett JL, Nelson JL. Comparison of
dermatopharmacokinetic vs. clinical efficacy methods for
bioequivalence assessment of miconazole nitrate vaginal
cream, 2% in humans. Pharm Res 2002;19:270-7. Crossref
53. Caterina MJ, Schumacher MA, Tominaga M, Rosen TA,
Levine JD, Julius D. The capsaicin receptor: a heat-activated
ion channel in the pain pathway. Nature 1997;389:816-24. Crossref
54. LaMotte RH, Shain CN, Simone DA, Tsai EF. Neurogenic
hyperalgesia: psychophysical studies of underlying
mechanisms. J Neurophysiol 1991;66:190-211.
55. Madsen CS, Johnsen B, Fuglsang-Frederiksen A, Jensen TS,
Finnerup NB. Increased contact heat pain and shortened
latencies of contact heat evoked potentials following
capsaicin-induced heat hyperalgesia. Clin Neurophysiol
2012;123:1429-36. Crossref
56. Kennedy WR, Vanhove GF, Lu SP, et al. A randomized,
controlled, open-label study of the long-term effects of
NGX-4010, a high-concentration capsaicin patch, on
epidermal nerve fiber density and sensory function in
healthy volunteers. J Pain 2010;11:579-87. Crossref
57. Anand P, Bley K. Topical capsaicin for pain management:
therapeutic potential and mechanisms of action of the
new high-concentration capsaicin 8% patch. Br J Anaesth
2011;107:490-502. Crossref