Hong Kong Med J 2015 Oct;21(5):475.e3–4
DOI: 10.12809/hkmj154528
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
PICTORIAL MEDICINE
‘Cleft sign’ of severe lipohypertrophy
CM Ng, FRCP (Edin), FHKAM (Medicine);
OL Chui, MNurs;
SC Tiu, FRCP (Lond), FHKAM (Medicine)
Department of Medicine, Queen Elizabeth Hospital, Jordan, Hong Kong
Corresponding author: Dr CM Ng (ngcm2@ha.org.hk)
A 45-year-old woman complained of increasing
truncal obesity in October 2014. Physical examination
revealed a ‘buttock-like’ configuration of her lower
abdomen, with a midline ‘cleft’ flanked on either side
by two rubbery pendulous masses (Fig 1).
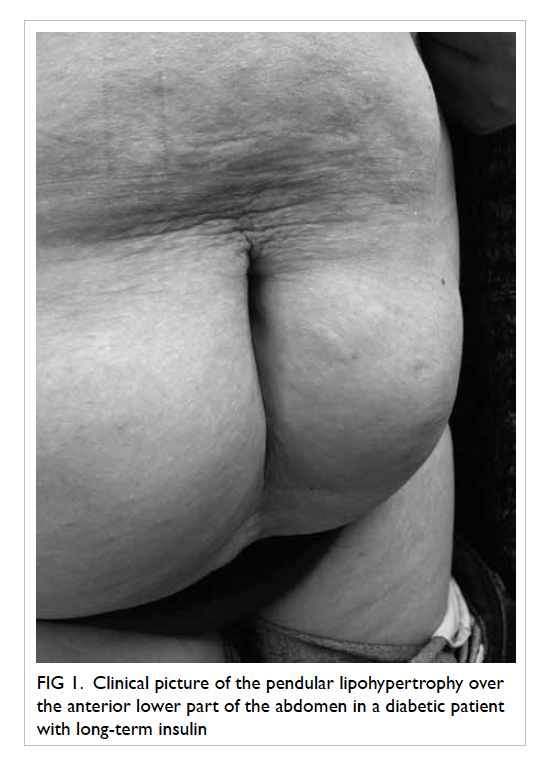
Figure 1. Clinical picture of the pendular lipohypertrophy over the anterior lower part of the abdomen in a diabetic patient with long-term insulin
She had diabetes mellitus and had been
injecting herself with Protaphane HM 26 IU (Novo
Nordisk A/S, Denmark) before bed, and Actrapid HM
15/20/20 IU (Novo Nordisk A/S, Denmark) 3 times a
day, since 2007. Knowing that insulin injection was
often accompanied by weight gain, she attributed
these subcutaneous masses, which had enlarged
slowly over the past 3 years, to abdominal obesity.
The physical finding was more compatible
with severe lipohypertrophy secondary to repeated
insulin injections. Although both conditions involve
an accumulation of adipocytes in the subcutaneous
layer, a ‘cleft’ is normally not seen in abdominal
obesity, except in patients with a history of vertical
sub-umbilical incision (Fig 2). In contrast, in severe insulin-injection lipohypertrophy, there is often this
tell-tale sign of a ‘cleft’, because injections are made
into either side of the abdomen with sparing of the
midline area.
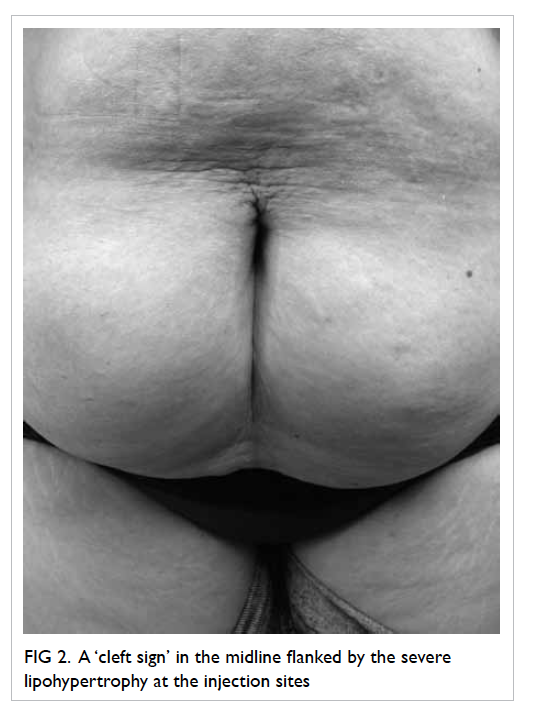
Figure 2. A ‘cleft sign’ in the midline flanked by the severe lipohypertrophy at the injection sites
Lipohypertrophy is a common complication
of insulin therapy and occurs in up to two thirds
of patients using insulin.1 Once a small area of
lipohypertrophy forms, patients tend to favour this
area for injection since it is less painful although it
results in growth of these masses. Risk factors include
use of long needles with wide-bore diameter, re-use
of the same needle, multiple injections, high doses
of insulin, and repeated injections into the same
sites.1 In our own clinic patient cohort, 89 (71%) out
of 125 patients using vial insulin and 36 (72%) of 50
patients using an insulin pen have lipohypertrophy
identifiable by palpation, albeit usually to a lesser
degree. Ultrasound or magnetic resonance imaging
examination may identify an even higher incidence.
Further injection into these areas is not advised
because insulin absorption from these fat masses can
be erratic; this results in hypoglycaemia or a need for
higher doses of insulin.2 Regular examination of the
injection sites for this local complication should be
made during patient follow-up, especially in patients
with unexplained fluctuations in glucose level. The
glycated haemoglobin level of this woman was 6.8%.
Her insulin requirement was 81 units per day. She
had occasional hypoglycaemic episodes at midnight.
The pathogenesis of lipohypertrophy remains
unknown, but is most probably related to the local
anabolic effect of insulin. Daily injection of a glucagon-like
protein-1 agonist has not been reported to cause
lipohypertrophy,3 making it unlikely for mechanical
trauma to be an important factor. Immunogenicity
also contributes little, since change to highly purified
human insulin has not decreased the incidence.
Avoidance of risk factors such as repeated
injection into the same sites, re-use of needles,
and multiple injections is important. Regression of
lipohypertrophy usually occurs over time if further
injections into the affected areas are avoided.
Nonetheless, caution should be exercised when
switching to other sites because insulin requirement
may be reduced.3 Liposuction may be considered
when there is serious cosmetic concern.4
References
1. Blanco M, Hernández MT, Strauss KW, Amaya M.
Prevalence and risk factors of lipohypertrophy in
insulin-injecting patients with diabetes. Diabetes Metab
2013;39:445-53. Crossref
2. Young RJ, Hannan WJ, Frier BM, Steel JM, Duncan LJ.
Diabetic lipohypertrophy delays insulin absorption.
Diabetes Care 1984;7:479-80. Crossref
3. Pledger J, Hicks D, Kirkland F, et al. Importance of injection
technique in diabetes. J Diabetes Nurs 2012;16:160-5.
4. Hardy KJ, Gill GV, Bryson JR. Severe insulin-induced
lipohypertrophy successfully treated by liposuction.
Diabetes Care 1993;16:929-30. Crossref

