Hong Kong Med J 2015 Oct;21(5):455–61 | Epub 28 Aug 2015
DOI: 10.12809/hkmj154572
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
REVIEW ARTICLE
Using the script concordance test to assess clinical reasoning skills in undergraduate and postgraduate medicine
SH Wan, MB, ChB, MRCP (Edin)
School of Medicine Sydney, University of Notre Dame, 160 Oxford Street, Darlinghurst, NSW 2010, Australia
Corresponding author: Dr SH Wan (michael.wan@nd.edu.au)
Abstract
The script concordance test is a relatively new format
of written assessment that is used to assess higher-order
clinical reasoning and data interpretation skills
in medicine. Candidates are presented with a clinical
scenario, followed by the reveal of a new piece of
information. The candidates are then asked to assess
whether this additional information increases or
decreases the probability or likelihood of a particular
diagnostic, investigative, or management decision.
To score these questions, the candidate’s decision in
each question is compared with that of a reference
panel of expert clinicians. This review focuses on
the development of quality script concordance
questions, using expert panellists to score the items
and set the passing score standard, and the challenges
in the practical implementation (including pitfalls to
avoid) of the written assessment.
Introduction
Script concordance test (SCT) is a relatively new
format of written assessment to assess higher-order
clinical reasoning and data interpretation skills of
medical candidates.1
In recent years, universities and postgraduate
colleges worldwide have used SCT for both formative
and summative assessment of clinical reasoning in
various medical disciplines including paediatric
medicine, paediatric emergency medicine, neurology,
orthopaedics, surgery, and radiology.2 3 4 5 6 7 8 In the classic
written assessment, multiple-choice questions
(MCQ) and short-answer questions (SAQ) usually
examine the candidates’ simple knowledge recall at
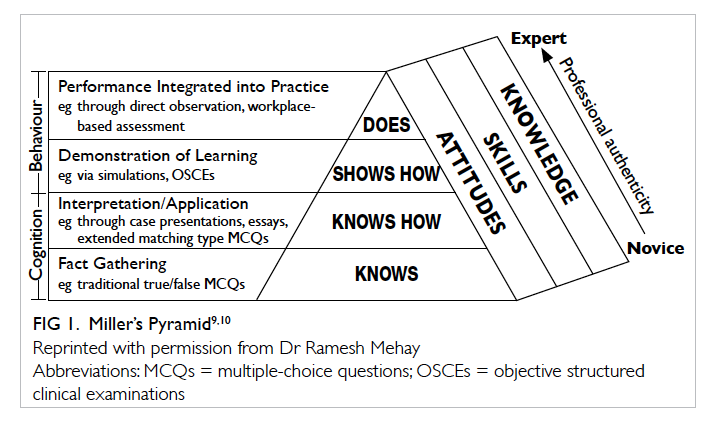
the lowest ‘knows’ level of the Miller’s Pyramid (Fig 1).9 10 Questions in SCT are able to test candidates at the higher order of thinking at the ‘knows how’ and even ‘shows how’ level. It is a unique assessment
tool that targets the essential clinical reasoning and
data interpretation skills in a very authentic way that
reflects the element of ‘uncertainty’ in real-world
clinical scenarios prevalent in clinical practice.
This is the key aspect of clinical competency that
enables medical graduates or fellows in training to
link and transfer their mastery of declarative clinical
knowledge and skills into clinical practice in a real
clinical setting. Recent literature reports the value
of using SCT to assess other areas of disciplines
where classic questions are difficult to develop, for
example, in assessing medical ethical principles and
professionalism.11
The structure and format of script concordance test
In SCT, candidates are presented with a clinical
vignette/scenario, followed by the reveal of a new
piece of information. The candidates are then
asked to assess whether this additional information
increases or decreases the probability or likelihood
of the suggested provisional diagnosis, and increases
or decreases the usefulness/appropriateness of a
proposed investigation or management option.
The process reflects everyday real-world decision-making
processes where clinicians retrieve their
‘illness scripts’ or network of knowledge (about
similar patient problems and presentations stored
in their memory) when faced with uncertainty in a
clinical presentation. This enables them to determine
the follow-on diagnosis and management options
most appropriate to the situation. As further clinical
encounters are experienced, the scripts are updated
and refined.12 Script concordance test assesses the
candidates’ clinical reasoning and data interpretation
ability in the context of uncertainty, particularly
involving ill-defined patient problems in clinical
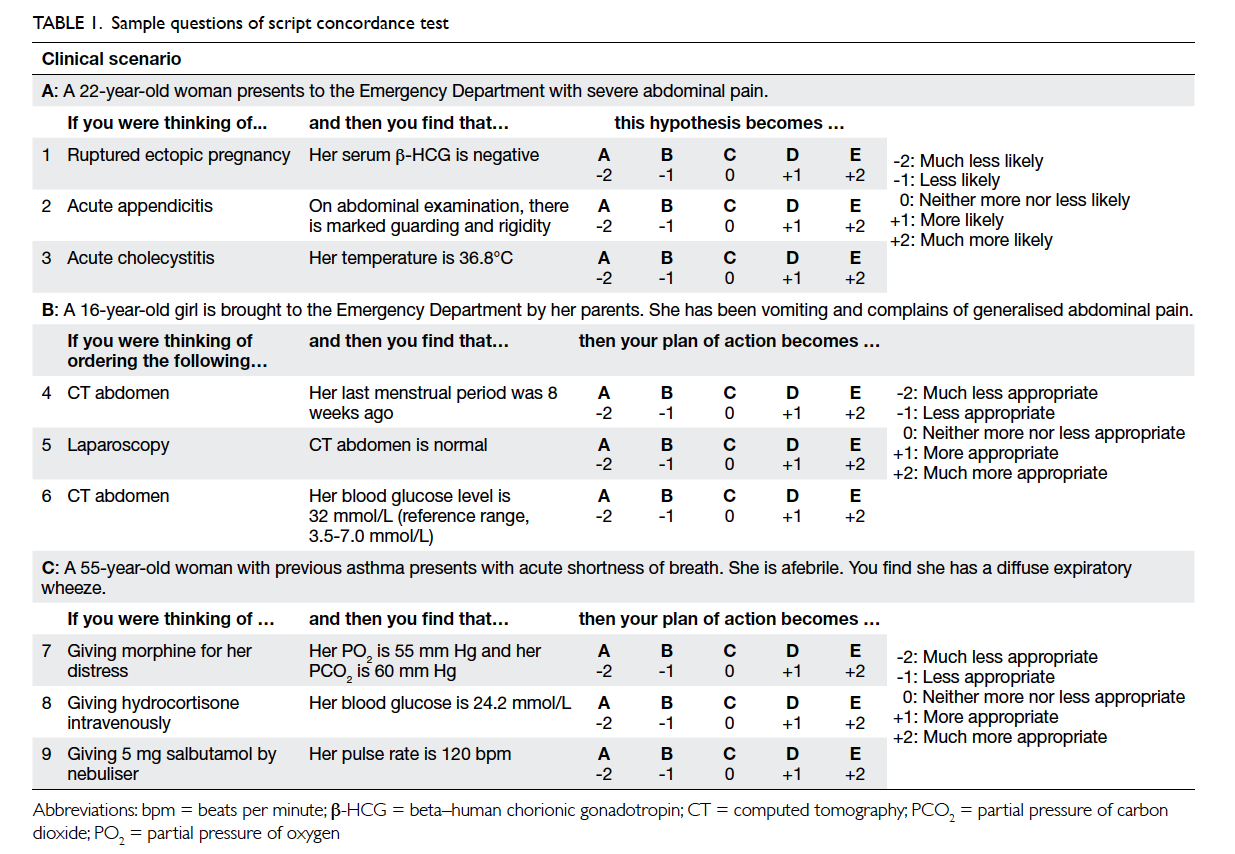
practice.13 Sample SCT questions in Table 1 illustrate
the structure and format of the SCT questions. As
the clinical scenario unfolds, additional data such as
clinical photos, radiological images, or audiovisual
material can also be presented to enhance the
authenticity of the scenarios.5 14 15
In scenario A in Table 1, the ‘clinical vignette’
is that of a 22-year-old woman who presents to the
Emergency Department with severe abdominal
pain. A piece of ‘new information’ is then revealed
that her serum beta–human chorionic gonadotropin
(β-HCG) is normal. The candidate is asked whether
this additional information makes the ‘diagnosis’ of
ectopic pregnancy: much less likely (-2), less likely
(-1), neither more nor less likely (0: no effect on the
likelihood), more likely (+1), or much more likely
(+2). The next piece of new information (independent
of the first one) is that the examination shows
marked guarding and rigidity of the abdomen and
the candidate is asked to determine the likelihood of
a diagnosis of acute appendicitis.
In scenario B in Table 1, a similar format is
used to assess the appropriateness of ordering an
investigation in relation to the respective piece
of additional information. The first question asks
for the appropriateness of ordering a computed
tomographic scan of the abdomen for a 16-year-old
girl who presents with acute abdominal pain if her
last menstrual period was 8 weeks ago.
In scenario C in Table 1, the focus is on
the usefulness of different management options
after being presented with different pieces of new
information related to the clinical vignette.
In preparing candidates to answer the
questions, it is crucial to emphasise that each piece
of new information is independent of the previous
piece but in the same clinical setting. For example,
in scenario A, when answering the second question
given that she has guarding and rigidity in the
abdomen, she does NOT have a serum β-HCG test
done.
With respect to the likelihood descriptors
used in the SCT questions for the diagnosis type
of scenario, the preference is to use the option of
“much less likely (-2)” rather than “ruling out the
diagnosis”; and “much more likely (+2)” rather than
“almost certain/definite diagnosis”. This will allow
candidates to use the full range of the five options.
In the practice of medicine, there are usually few
situations wherein a diagnosis can be confidently
excluded or definitely diagnosed with a few pieces of
information provided.3
There are nonetheless limitations to the
design and format of SCT. Candidates cannot seek
additional information to that given in the question;
the scenario is only a snapshot of the clinical
encounter without the comprehensive history,
physical examination, and investigations that would
be particularly desirable in an ambiguous clinical
situation.16
Scoring script concordance test
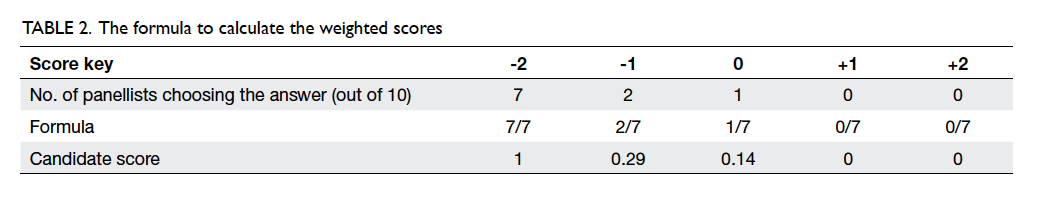
To score these questions, the candidate’s decision in
each question is compared with that of a reference
panel of expert clinicians. Each member of the
panel attempts the same set of questions and the
answers are recorded. As there is no single best
correct answer to the question, a full (1) mark will be
awarded if the candidate’s decision concurs (hence
the name ‘concordance’) with the majority of the
expert panel. A proportional (partially credited or
weighted) score (<1) will be given if the candidate’s
decision concurs with the minority of the panel. The
candidate will score a ‘0’ if no panellist chooses this
option.3 The formula to calculate the weighted scores
is shown in Table 2.
There are other scoring methods reported in
the literature where a consensus-based single-answer
scoring method or 3-point Likert scale scoring
method is employed to determine the candidate
scores.4 17
Selecting the reference panel
In general, a panel of 10 to 15 expert members
relevant to the discipline is recommended to produce
credible and reliable scores.18 The inter- and intra-rater
reliability in the SCT panel have been shown to
be good.19
The composition of the panel should include
clinical teachers and academics who are familiar
with the curriculum and experts in the field relevant
to the discipline tested. Studies have shown that
using general practitioners (GPs) in the panel may
produce similar mean scores to specialists but with a
wider standard deviation.3
A recent study, however, raised concerns about
the reference standard and judgement of the expert
panel. The study compared 15 emergency medicine
consultants’ judgement scores with evidence-based
likelihood ratios. The results showed that 73.3%
of the mean judgement was significantly different
to the corresponding likelihood ratios, with 30%
overestimation, 30% underestimation, and 13.3%
with diagnostic values in the opposite direction.20
Other studies raised concerns about the possibility
of outdated clinical knowledge and cognitive bias in
the experts’ decision-making.21 22 Evidence of context
specificity has also been highlighted whereby the
agreement between SCT scores derived using
different scoring keys with expert reference panels
from a different context (hospitals and specialty) was
poor.23
Implementation of script concordance test in formative and summative assessments
The structure and layout of the SCT questions can
easily be implemented in the usual pen and paper-based
or online electronic format. Candidates
answer each question (with five options) using a
standardised answer sheet to facilitate computer
scanning and scoring or directly online using the
computer.
It is often difficult to get busy clinicians to
meet together face-to-face to answer the questions.
By uploading the questions online, the panellists
can attempt them anytime and make the questions
available through a secure online platform. The
response data can then be collated and the weighted
scores for responses on each score scale calculated.3
After capturing the candidates’ responses for
all items, scoring of responses for each question
can then be performed using the formula described
above. This will ensure a rapid turnaround time that
will be very effective in the assessment process.
For formative assessment purposes, expert
panel consensus scores are provided to the
candidates, followed by expert clinicians explaining
and discussing the options in each scenario with
the candidates for constructive feedback. Script
concordance test can also be used to identify
borderline students with suboptimal clinical
reasoning skills for appropriate remedial measures
such as bedside teaching, tutorials, or clinical
simulations.24
For summative assessment purposes,
particularly where there is not a large pool of SCT
items, it is important to avoid constructing irrelevant
variance in SCT scores, by not releasing or discussing
post-examination, the expected responses (based on
expert panel’s responses), and the associated score
for each of the answer options in SCT items.
Unlike MCQ where there is only one single
best answer that candidates could memorise and
disseminate after the examination, the partial credit
scoring model applied in SCT, where multiple
answer options are accepted and each carries a
fraction or all of the allocated mark, has to a certain
extent rendered sharing of ‘correct’ answers after the
examination difficult.
Developing quality script concordance test questions
Each clinical scenario has to be authentic and
the presentation represents a realistic clinical
encounter that is relevant to the specific discipline,
preferably with a certain degree of uncertainty. The
new information presented needs to stimulate the
candidate to re-consider and re-evaluate how that
particular piece of new information will affect the
likelihood of the initial diagnosis, or appropriateness
of initial planned investigation or management
option. This will ensure the content validity in the
SCT questions.
Particular care should be taken to develop
options that will attract the full range of the five
options available for the candidate to choose from. In
other words, the additional pieces of new information
should result in the consideration of -2 and +2 as well
as -1, 0, and +1 options. A test-wise candidate might
choose to consider only the options of -1, 0 and +1 if
they notice that most panel consensus answers with
a full score of 1 mark usually fall within these three
options rather than also covering the -2 and +2.25 As
a result, developing good-quality SCT questions is
not easy. Care should be taken to develop clinical
scenarios that do not focus solely on factual recall
but involve a reasoning process with elements of
uncertainty that will likely attract responses that
spread across the 5-point Likert scale.26
Reliability and validity of script concordance test as an assessment tool
The reliability of SCT as an assessment tool has been
investigated.2 6 A 60- to 90-minute examination will
produce a Cronbach’s alpha of 0.70 to 0.85.7 25 27 28 There
are concerns, however, about inter-panellist errors
in SCT; the use of Cronbach’s alpha in measuring the
reliability of the test where partial credit model of
scoring is used, ie multiple options/responses are
awarded either a full or fraction of allocated mark;
and case scenarios that could create inconsistencies
among items.
As an assessment tool, SCT has been shown
to be valid in assessing clinical reasoning.13 14 19 28
Studies have shown that SCT scores correlate well
with other assessment scores from the clinical years
of the candidates.2
The construct validity of SCT questions can
be examined by correlating the scores with the
level of training to predict future performance on
clinical reasoning. A recent study has compared the
progression of clinical reasoning skills of medical
students with those of a group of practising GPs who
are also their Problem Based Learning group tutors.29
Another study showed that there was a statistically
significant gain in SCT performance over a 2-year
period in two different cohorts of medical students
using the same set of 75-item SCT.26 There was
significant progression of clinical reasoning skills
from medical students at the novice level through
to practising GP clinicians, reflected by the higher
scores in the GP group attempting the SCT questions.
Empirical evidence supporting the construct
validity based on progression of SCT scores with
clinical experience from undergraduate students to
postgraduate training has also been reported.2 5 24 30 31
The construct validity of SCT has been questioned
because of the logical inconsistencies as a result
of partial credit scoring methodology making it
possible for a hypothesis to be simultaneously more
likely and less likely.32 Nonetheless, a certain degree
of variability in panel scores has been shown to be a
key determinant of the discriminatory power of the
test and allows richness of thinking about clinical
cases.33 34 Another study found that 27% of residents
in one SCT administration scored above the expert
panel’s mean, which may indicate issues with the
construct validity, particularly in the credibility and
validity of the scoring key and hence the resulting
SCT scores interpretation.33
Test-wise candidates would select the answers
to be around ‘0’ rather than ‘-2’ or ‘+2’ if they noticed
that most panellist scores did not fall in the ‘extreme’
(-2 or +2) range due to the construct of the SCT
questions and options. This could be avoided by
first using the option descriptor of “much less likely
(-2)” and “much more likely (+2)” rather than “ruling
out the diagnosis” and “almost certain/definite
diagnosis” as described in the format of SCT section
above.19 Second, when collating the SCT questions
into an examination paper, one could select a
relatively equal number of items with both ‘extreme’
answers as well as median answers. Recent data
have shown that by employing the above strategies
in developing the paper, candidates who chose ‘0’ for
all the questions would score only around 25% in
the SCT examination and would gain no advantage
(unpublished data). This is in contrast to the finding
of another study wherein candidates who chose
the midpoint scale (‘0’) performed better than the
average candidate.32
The correlation of SCT scores with other
modalities of assessment would be expected to
be low as SCT is designed to measure clinical
reasoning rather than factual or knowledge recall.
The correlation coefficient between SCT and MCQ
was poor (r=0.22), and that between SCT and extended matching
questions (EMQ) was 0.46.4
Collating and moderating the expert reference panellist responses
In collating the SCT questions for use in a summative
examination, appropriate clinical scenarios/vignettes with the related diagnoses, investigations,
and management should be selected according to
the blueprint of the assessment. The clinical topics
should have a good spread and represent core areas
of learning that are relevant to the curriculum and
appropriate to the level of training of the candidates.
In reviewing the expert panel responses to
each question, bi-modal and uniform divergence
responses should trigger a detailed scrutiny of the
clinical vignette and the options. In the case of bi-modal
response (Fig 2a), the panel has an equal split of the best option between -2 and +2. This usually
results from an error in the question or a controversial
investigation or management option with discordant
‘expert opinions’. A modification of the question and
re-scoring will usually solve this issue. If re-scoring
results in the same bi-modal response, the question
should be discarded for scoring in the examination.
In the case of uniform divergence responses (Fig 2b), there is an equal spread in the number of
members choosing all the five options. This usually
signifies a non-discriminating question and the
item should again be discarded. A discrete outlier
response (Fig 2c) usually represents an error in the particular panellist’s decision or ‘clicking the wrong
answer accidentally’ when the member should have
answered -2 instead of +2. The ideal pattern would
be relatively close convergence with some variation
(Fig 2d).3
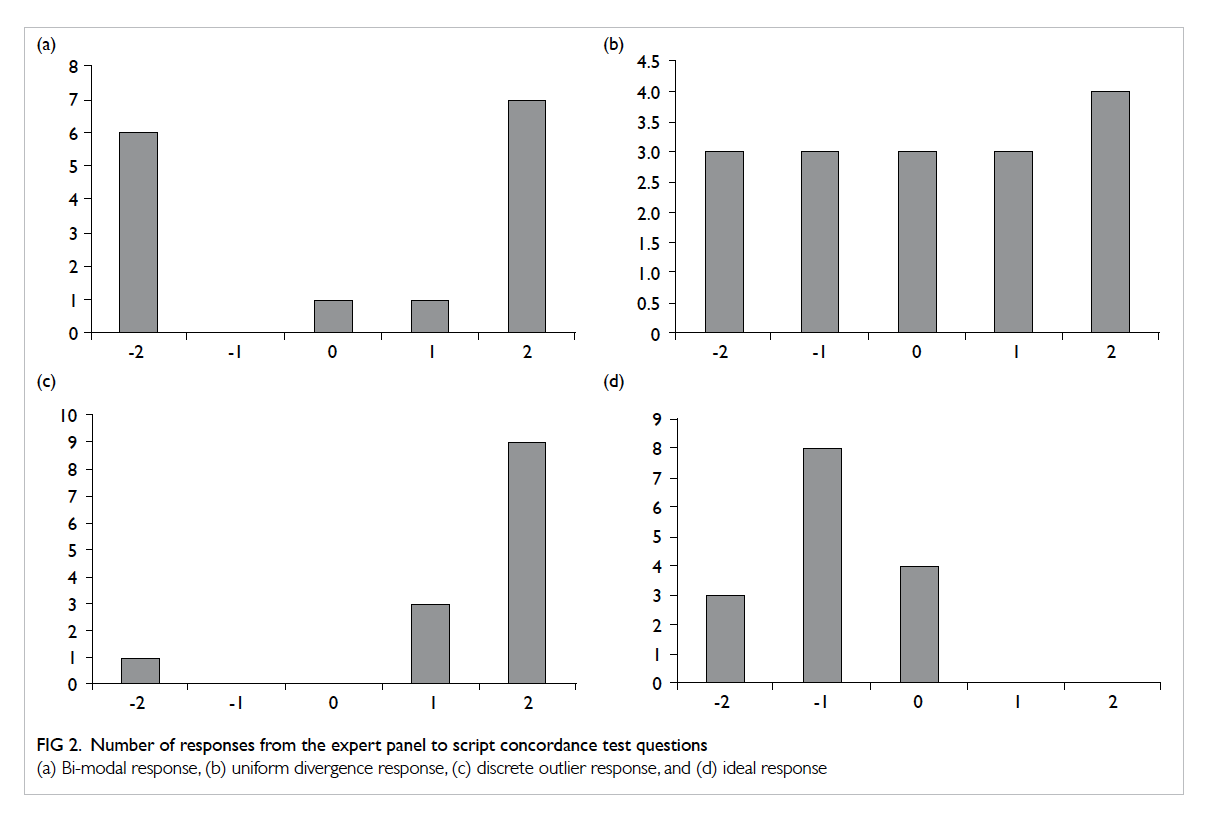
Figure 2. Number of responses from the expert panel to script concordance test questions
(a) Bi-modal response, (b) uniform divergence response, (c) discrete outlier response, and (d) ideal response
As mentioned previously, the set of questions
in the SCT examination should be selected in such
a way that there are similar numbers of full marks
in each option across the five options. This will
avoid the test-wise candidates being advantaged by
selecting only the -1, 0, or +1 options and avoiding
the extreme options of -2 and +2.3 By employing this
strategy to select questions that cover the full 5-point
Likert scale, test-wise students will only score 25%
in the SCT examination if they choose the response
of ‘0’ for all questions (unpublished data) compared
with 57.6% in another cohort sitting a SCT test
without the specific question selection process.32
Standard setting the pass/fail cutoff score
In setting the pass/fail cutoff score of the SCT
questions, the expert panels’ mean scores and
standard deviations are chosen to guide the process.
This is calculated by asking all the members of the
panel to attempt the same set of SCT questions and
their responses are then scored accordingly. The
borderline score of the undergraduate students is
usually set at 3 to 4 standard deviations below the
expert panel’s mean score.3 35 Studies have shown
that using recent graduates or fellows in training
might result in a mean score that is closer to the
students’ mean and therefore a smaller number of
standard deviations would be more appropriate.3
Other methods of standard setting include
using the single correct answer method.29 36 Standard
setting of a pass/fail cutoff score is an area that
warrants ongoing research to inform and improve
the practice of using SCT as a summative assessment
tool for clinical data interpretation and decision-making
skills.
The use of script concordance test in the Asia-Pacific region and its limitations
Examinations using SCT have been successfully
implemented in the school-entry medical schools in
Indonesia, Singapore, Taiwan, and Australia3 7 36 37; and
in graduate-entry medical schools in Australia.29 38
Such test has the potential to supplement MCQ and
SAQ to test the higher-order thinking of medical
candidates to allow a more robust overall written
assessment in the assessment programme. In fact,
SCT is one of the few currently available assessment
tools for clinical reasoning in a written format.28 It
can be implemented relatively easily in the paper-based
format or online. Initial pilot examinations can
be set as a formative exercise to enhance candidates’
feedback and learning.24 Further collaboration
with other institutions to develop, score, and share
question items can ensure effective and efficient
delivery of such examinations.
Limitations to the widespread usage of SCT
could be due to: difficulties in developing good-quality
SCT clinical scenarios, concerns about the
validity of the test, recruiting a sufficient number of
appropriate expert clinicians for the reference panel,
lack of a general consensus in setting the borderline
pass mark, and the candidates’ familiarity with the
question format.3 24 25 28 32 34
Conclusions
This article attempts to review the current
use of SCT in assessing clinical reasoning and
data interpretation skills in undergraduate and
postgraduate medicine. The empirical evidence
reported for the reliability and validity of SCT
scores from existing literature seems encouraging.
Approaches to develop quality items, moderation
of expert panel scoring and these post-hoc quality
assurance measures, and optimisation of scoring
scale will to a certain extent mitigate the threat
to the validity of SCT score interpretation and
its use for summative examination purposes.
Combining SCT (testing the clinical reasoning and
data interpretation skills with authentic written
simulations of ill-defined clinical problems set at the
‘knows how’ level) with MCQ/SAQ/EMQ (testing
the ‘knows’ and ‘knows how’), objective structured
clinical examination (testing ‘shows how’), and
workplace-based assessment (testing the ‘does’) in
the medical curriculum will enhance the robustness
and the credibility of the assessment programme.
Further research into the use of SCT in both
undergraduate and postgraduate medical education
is warranted, particularly on standard setting for the
pass/fail cutoff score and best practices that may
help reduce the threat to the validity of SCT scores.
References
1. Charlin B, Roy L, Brailovsky C, Goulet F, van der Vleuten C.
The Script Concordance test: a tool to assess the reflective
clinician. Teach Learn Med 2000;12:189-95. Crossref
2. Carrière B, Gagnon R, Charlin B, Downing S, Bordage
G. Assessing clinical reasoning in pediatric emergency
medicine: validity evidence for a Script Concordance Test.
Ann Emerg Med 2009;53:647-52. Crossref
3. Duggan P, Charlin B. Summative assessment of 5th year
medical students’ clinical reasoning by Script Concordance
Test: requirements and challenges. BMC Med Educ
2012;12:29. Crossref
4. Kelly W, Durning S, Denton G. Comparing a script
concordance examination to a multiple-choice examination
on a core internal medicine clerkship. Teach Learn Med
2012;24:187-93. Crossref
5. Lubarsky S, Chalk C, Kazitani D, Gagnon R, Charlin B.
The Script Concordance Test: a new tool assessing clinical
judgement in neurology. Can J Neurol Sci 2009;36:326-31. Crossref
6. Meterissian S, Zabolotny B, Gagnon R, Charlin B. Is the
script concordance test a valid instrument for assessment
of intraoperative decision-making skills? Am J Surg
2007;193:248-51. Crossref
7. Soon D, Tan N, Heng D, Chiu L, Madhevan M. Neurologists
vs emergency physicians: reliability of a neurological script
concordance test in a multi-centre, cross-disciplinary
setting. Neurology 2014;82(10 Suppl):327.
8. Talvard M, Olives JP, Mas E. Assessment of medical
students using a script concordance test at the end of their
internship in pediatric gastroenterology [in French]. Arch
Pediatr 2014;21:372-6. Crossref
9. Miller GE. The assessment of clinical skills/competence/performance. Acad Med 1990;65(9 Suppl):S63-7. Crossref
10. Mehay R. The essential handbook for GP training and
education. Chapter 29. Assessment and competence.
Available from: http://www.essentialgptrainingbook.com/chapter-29.php. Accessed 10 May 2015.
11. Foucault A, Dubé S, Fernandez N, Gagnon R, Charlin
B. Learning medical professionalism with the online
concordance-of-judgment learning tool (CJLT): A pilot
study. Med Teach 2014 Oct 22:1-6. Epub ahead of print. Crossref
12. Schmidt HG, Norman GR, Boshuizen HP. A cognitive
perspective on medical expertise: theory and implications.
Acad Med 1990;65:611-21. Crossref
13. Lubarsky S, Charlin B, Cook DA, Chalk C, van der Vleuten
CP. Script concordance testing: a review of published
validity evidence. Med Educ 2011;45:329-38. Crossref
14. Brazeau-Lamontagne L, Charlin B, Gagnon R, Samson
L, Van Der Vleuten C. Measurement of perception and
interpretation skills during radiology training: utility of the
script concordance approach. Med Teach 2004;26:326-32. Crossref
15. Collard A, Gelaes S, Vanbelle S, et al. Reasoning versus
knowledge retention and ascertainment throughout
a problem-based learning curriculum. Med Educ
2009;43:854-65. Crossref
16. Lineberry M, Kreiter CD, Bordage G. Script concordance
tests: strong inferences about examinees require stronger
evidence. Med Educ 2014;48:452-3. Crossref
17. Williams RG, Klamen DL, White CB, et al. Tracking
development of clinical reasoning ability across five medical
schools using a progress test. Acad Med 2011;9:1148-54. Crossref
18. Gagnon R, Charlin B, Coletti M, Sauvé E, van der Vleuten
C. Assessment in the context of uncertainty: how many
members are needed on the panel of reference of a script
concordance test? Med Educ 2005;39:284-91. Crossref
19. Dory V, Gagnon R, Vanpee D, Charlin B. How to construct
and implement script concordance tests: a systematic
review. Med Educ 2012;46:552-63.
20. Ahmadi SF, Khoshkish S, Soltani-Arabshahi K, et al.
Challenging script concordance test reference standard
by evidence: do judgments by emergency medicine
consultants agree with likelihood ratios? Int J Emerg Med
2014;7:34. Crossref
21. Ramos K, Linscheid R, Schafer S. Real-time information-seeking
behavior of residency physicians. Fam Med
2003;35:257-60.
22. Norman GR, Eva KW. Diagnostic error and clinical
reasoning. Med Educ 2010;44:94-100. Crossref
23. Tan N, Tan K, Ponnamperuma G. Expert clinical
reasoning is not just local but hyperlocal—insights into
context specificity from a multicentre neurology script
concordance test. Neurology 2015;84(14P4):191.
24. Ducos G, Lejus C, Sztark F, et al. The Script Concordance
Test in anesthesiology: Validation of a new tool for
assessing clinical reasoning. Anaesth Crit Care Pain Med
2015;34:11-5. Crossref
25. See KC, Tan KL, Lim TK. The script concordance test for
clinical reasoning: re-examining its utility and potential
weakness. Med Educ 2014;48:1069-77. Crossref
26. Humbert AJ, Miech EJ. Measuring gains in the clinical
reasoning of medical students: longitudinal results
from a school-wide script concordance test. Acad Med
2014;89:1046-50. Crossref
27. Gagnon R, Charlin B, Lambert C, Carrière B, Van der
Vleuten C. Script concordance testing: more cases or more
questions? Adv Health Sci Educ Theory Pract 2009;14:367-75. Crossref
28. Nouh T, Boutros M, Gagnon R, et al. The script
concordance test as a measure of clinical reasoning: a
national validation study. Am J Surg 2012;203:530-4. Crossref
29. Wan SH. Using Script Concordance Testing (SCT) to
assess clinical reasoning—the progression from novice to
practising general practitioner. Proceedings of the 11th
Asia Pacific Medical Education Conference; 2014 Jan
15-19; Singapore.
30. Charlin B, van der Vleuten C. Standardized assessment in
contexts of uncertainty: The script concordance approach.
Eval Health Prof 2004;27:304-19. Crossref
31. Lambert C, Gagnon R, Nguyen D, Charlin B. The script
concordance test in radiation oncology: validation study
of a new tool to assess clinical reasoning. Radiat Oncol
2009;4:7. Crossref
32. Lineberry M, Kreiter C, Bordage G. Threats to validity
in the use and interpretation of script concordance test
scores. Med Educ 2013;47:1175-83. Crossref
33. Charlin B, Gagnon R, Lubarsky S, et al. Assessment in the
context of uncertainty using the script concordance test:
more meaning for scores. Teach Learn Med 2010;22:180-6. Crossref
34. Lubarsky S, Gagnon R, Charlin B. Scoring the Script
Concordance Test: not a black and white issue. Med Educ
2013;47:1159-61. Crossref
35. Wan SH, Clarke R. Using a clinician panel to set the
borderline mark for Script Concordance Testing (SCT) to
assess clinical reasoning for graduating medical candidates.
Proceedings of the 8th International Medical Education
Conference; 2013 March 13-15; Kuala Lumpur, Malaysia.
36. Irfannuddin I. Knowledge and critical thinking skills
increase clinical reasoning ability in urogenital disorders:
a Universitas Sriwijaya Medical Faculty experience. Med J
Indonesia 2009;18:53-9. Crossref
37. Tsai TC, Chen DF, Lei SM. The ethics script concordance
test in assessing ethical reasoning. Med Educ 2012;46:527. Crossref
38. Ingham AI. The great wall of medical school: a comparison
of barrier examinations across Australian medical schools.
Aus Med Student J 2011;2:5-8.