Hong Kong Med J 2015 Oct;21(5):407–10 | Epub 3 Jul 2015
DOI: 10.12809/hkmj144440
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
ORIGINAL ARTICLE
Is locking plate fixation a better option than casting for distal radius fracture in elderly people?
LP Hung, MRCSEd1;
YF Leung, FHKAM (Orthopaedic Surgery)1;
WY Ip, MS, FHKAM (Orthopaedic Surgery)2;
YL Lee, FHKAM (Orthopaedic Surgery)1
1 Department of Orthopaedics and Traumatology, Tseung Kwan O Hospital, Tseung Kwan O, Hong Kong
2 Department of Orthopaedics and Traumatology, Queen Mary Hospital, Pokfulam, Hong Kong
Corresponding author: Dr LP Hung (joshua.hlp@gmail.com)
Abstract
Objectives: To compare the outcomes of locking
plate fixation versus casting for displaced distal
radius fracture with unstable fracture pattern in
active Chinese elderly people.
Design: Historical cohort study.
Setting: Orthopaedic ward and clinic at Tseung
Kwan O Hospital, Hong Kong.
Patients: Between 1 May 2010 and 31 October 2013,
57 Chinese elderly people aged 61 to 80 years were
treated either operatively with locking plate fixation
(n=26) or conservatively with cast immobilisation
(n=31) for unstable displaced distal radius fracture.
Main outcome measures: Clinical, radiological, and
functional outcomes were assessed at 9 to 12 months
after treatment.
Results: The functional outcome (based on the
quick Disabilities of the Arm, Shoulder and Hand score) was significantly better in
the locking plate fixation group than in the cast immobilisation group, while clinical and
radiological outcomes were comparable with those
in other similar studies.
Conclusions: Locking plate fixation resulted in
better functional outcome for displaced distal radius
fracture with unstable fracture pattern in active
Chinese elderly people aged 61 to 80 years. Further
prospective study with long-term follow-up is
recommended.
New knowledge added by this
study
- In active Chinese elderly people aged 61 to 80 years, apart from better clinical and radiological outcomes than cast immobilisation, locking plate fixation for displaced distal radius fracture with unstable fracture pattern also improves functional outcome.
- We advise management of displaced distal radius fracture with unstable fracture pattern with locking plate fixation in active Chinese elderly people aged 61 to 80 years.
Introduction
Since the introduction of locking plate fixation,
there has been a tendency to manage distal radius
fracture in elderly people with plate fixation over
cast fixation. In the US, the rate of plate fixation in
elderly people increased 5-fold from 3% in 1996 to
16% by 2005.1
Only a few recent studies have compared
conservative versus operative management of distal
radius fracture in elderly people. Some authors have
concluded that, while grip strength was significantly
better after operation, functional outcome did not
improve.2 3
In Hong Kong, Chinese elderly people tend to
have poorer bone quality than western people of the
same age.4 Life expectancies in Hong Kong, however,
are one of the longest in the world, at 80.9 years for
men and 86.6 years for women in 2013.5 Moreover, an
increasing number of people older than 60 years are
still working and therefore the expectation for clinical
outcomes after distal radius fracture will be higher
than that in the past. As a result, it is imperative to
investigate whether locking plate fixation is a good
option in treating distal radius fracture in Chinese
elderly people. The aim of this study was to compare
the outcomes between locking plate fixation and
cast immobilisation as treatment for displaced distal
radius fracture with unstable fracture pattern in
Chinese elderly people.
Methods
The hospital database was reviewed for elderly
patients with distal radius fracture from 1 May
2010 to 31 October 2013. The study was approved
by the Research Ethics Committee of the Hospital
Authority, Hong Kong.
The operation rate for distal radius fracture
decreased with age and elderly patients (>70 years)
tended to prefer conservative management. The
oldest patient who underwent locking plate fixation
was 77 years. As a result, our inclusion criteria were:
Chinese patients, aged 61 to 80 years, having displaced
distal radius fracture with unstable fracture pattern
(defined as having at least three out of five criteria
of: initial dorsal angulation >20°, initial shortening
>5 mm, >50% dorsal comminution, intra-articular
fracture, and ulnar fracture6), and completion of a
rehabilitation programme after either operative or
conservative management.
The exclusion criteria were: operative
management other than 2.4- or 3.5-mm locking
compression plates (eg K-wire fixation, non-locking
plate fixation, or external fixation), open fracture or
neurovascular deficits requiring immediate operative
management, concomitant same-side upper limb
injury (eg elbow dislocation, shoulder dislocation, or
humeral fracture) that affected the overall functional
outcome, and a history of medical illness (eg stroke
or dementia) that hindered the rehabilitation results.
A total of 57 patients were identified. All of
the patients were active, independent in activities
of daily living, and otherwise healthy. The patients
were admitted to orthopaedic ward at Tseung Kwan O Hospital, Hong Kong from the
Accident and Emergency Department. Initial closed
reduction of distal radius fracture under local
anaesthesia and immobilisation with a backslab were
performed. Options of conservative management
with cast immobilisation or operative management
with locking plate fixation and the associated risks
and complications were discussed with the patients.
The patient made the final decision with written
consent for either treatment.
For patients who opted for cast immobilisation,
the reduced fracture was immobilised with a short
arm cast for 6 weeks, followed by mobilisation and
strengthening exercises. For patients who opted for
locking plate fixation, the operation was done under
general anaesthesia with an arm tourniquet. The
modified Henry approach was used and the fracture
was fixed with a 2.4- or 3.5-mm locking compression
plate, followed by immediate mobilisation and then
strengthening exercises. All patients were reviewed
regularly in the orthopaedic out-patient clinic,
with serial radiographs and rehabilitation until
they reached the maximal improvement in range of
motion and grip strength.
At the beginning of this retrospective study,
the majority of the patients had been discharged
from the clinic. In view of the technical difficulty of
calling back elderly patients for physical assessment,
the clinical parameters recorded in the last section of
the rehabilitation programme were collected and the
last radiographs taken in the clinic were retrieved
for measurement. The duration from treatment to
the last section of the rehabilitation programme
averaged 10 months (range, 6-12 months) and the
duration from treatment to the last radiographs
averaged 9 months (range, 6-14 months).
Clinical parameters, including range of motion
and grip strength of both hands, were measured by
physiotherapists and occupational therapists not
involved in this study. Radiographic parameters—including volar tilt, radial inclination, radial length,
and ulnar variance—were measured by one of the
investigators.
Functional outcome was assessed using the
quick Disabilities of the Arm, Shoulder and Hand questionnaire
(DASH) score at a mean of 12 months (range, 6-24
months) after treatment; DASH score is a measure
of a patient’s perceived disability. The quick DASH
was chosen instead of the full DASH because the
elderly patients generally had a low educational
background, making completion of a comprehensive
questionnaire difficult. The 11-question evaluation
was completed by means of an interview in the
clinic, a telephone interview, or answers to a mailed
questionnaire. In summary, clinical, radiological, and functional outcomes were assessed at 9 to 12 months after treatment.
Data were assessed with different statistical
tests. For categorical variables, Chi squared test (for
sex and side of injury) and analysis of variance (for
Orthopaedic Trauma Association classification)
were used. For continuous variables, independent
sample t test was used for normally distributed
data (including grip strength and radiographic
parameters) and Mann-Whitney U test for non-normally
distributed data (including age, range of
motion, and quick DASH score). A P value of ≤0.05
was considered statistically significant.
Results
Of 57 patients enrolled in this study, 26 were treated
with locking plate fixation and 31 were treated with
cast immobilisation. The number of patients in the
cast immobilisation group was low because many
of them were either excluded due to stable fracture
pattern (n=31) or were lost to follow-up in the
rehabilitation programme (n=49). There were no
statistically significant differences in characteristics
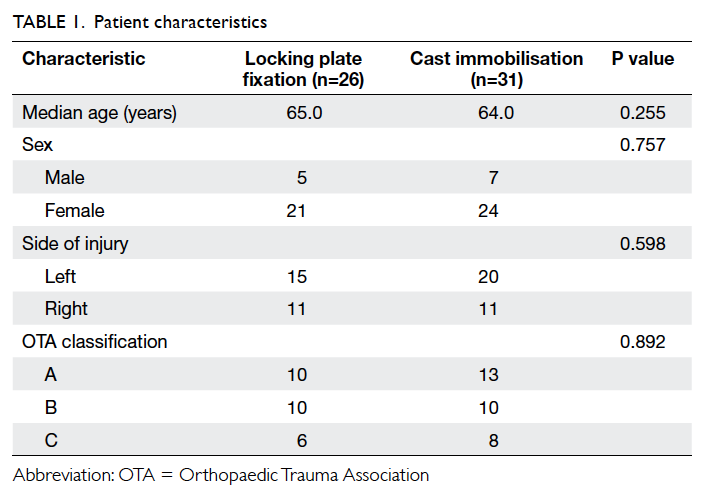
between the two groups (Table 1).
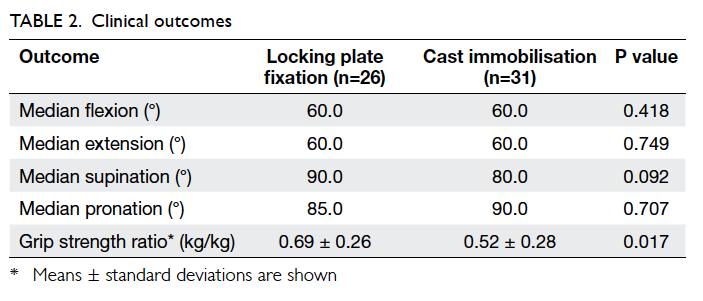
Clinical outcomes are shown in Table 2. Grip
strength was presented in the form of fraction of grip
strength in the non-injured side as the denominator.
The operative group did not achieve significantly better range of
motion when compared with the cast immobilisation
group, but grip strength was significantly better.
Only one complication was documented, which was
carpal tunnel syndrome after cast immobilisation.
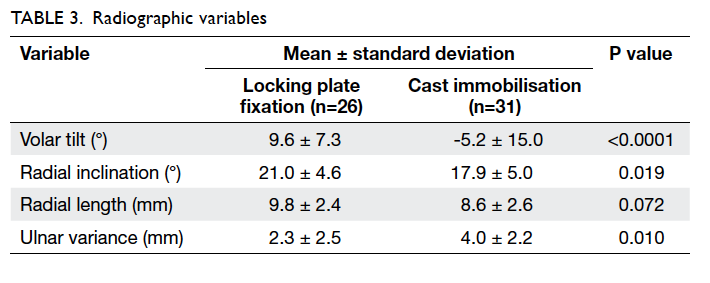
There was a statistically significant improvement
in the radiographic parameters (except for radial
length) after anatomical reduction in the operative
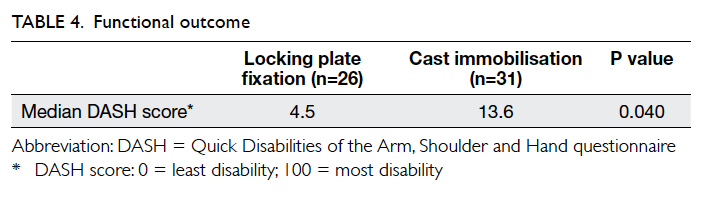
group (Table 3). Regarding functional outcome, the operative group perceived significantly less disability
than the cast immobilisation group (Table 4).
Discussion
This study found that locking plate fixation for
displaced, unstable distal radius fracture achieved
significantly better grip strength, radiographic
parameters, and functional outcome when compared
with cast immobilisation in elderly people aged 61 to
80 years.
Whether anatomical reduction results in
better functional outcome in elderly people with
displaced distal radius fracture of unstable fracture
pattern is still a controversial topic. Some authors
have reported satisfactory functional outcome
after cast immobilisation for displaced distal radius
fracture in low-demand elderly people, regardless of
the radiographic result.7 8 In the younger age-group,
reconstruction of articular congruity of displaced
intra-articular distal radius fractures by means of
internal fixation and/or external fixation have long
been known to improve functional outcome.9 Only
a few studies in the literature have investigated this
correlation in elderly patients.
One historical cohort study compared the
outcomes of 90 patients older than 65 years who
were treated either operatively with plate-and-screw
fixation or external fixation, or conservatively with
cast immobilisation.3 Grip strength and radiographic
parameters were superior in the operative group, but
there was no difference in other outcomes including
DASH score.3 In one prospective randomised trial,
73 patients aged 65 years or older were randomised
to receive open reduction internal fixation with
volar locking plate or closed reduction and cast
immobilisation.2 Similar results were reported.
Lastly, in one diagnostic study examining 53 patients
older than 55 years, operative intervention was
found to have no influence on functional outcome.10
Our study has a discrepancy for functional
outcome, although clinical and radiological
outcomes were consistent with the previous studies.
Our opinion is that the previous studies included
some patients older than 80 years, for whom
operation might not be suitable due to poorer
premorbid status and lower functional demand than
those aged 61 to 80 years. Therefore, the overall
functional outcome did not improve after operation.
We believe that locking plate fixation for active
Chinese elderly people aged up to 80 years could
achieve good clinical, radiological, and functional
outcomes. However, the decision should not only
be determined by chronological age but also be
balanced with functional age and medical condition.
There are some limitations to this study. Since
it is a non-randomised study, there might have been
bias during discussion of the treatment options with
the patients. Moreover, the two groups of patients
were not blinded (and could not be blinded) to the
therapists and investigator in assessing the clinical
and radiological outcomes, which might have
resulted in information bias. A substantial number
of eligible patients defaulted the rehabilitation
programme (four in the operative group, 49 in the
cast immobilisation group) and were counted as
loss to follow-up. Therefore, there was a possibility
of self-selection bias among the remaining patients,
who had better motivation for rehabilitation and
regaining functions. Other confounding factors,
such as differences in background characteristics
and expectations of outcome, might have made the
two groups of patients non-comparable. The follow-up
duration was relatively short due to limitations of
human resources. The times for assessing outcomes
were not standardised due to the retrospective
nature of this study. The sample size was relatively
small due to the strict inclusion and exclusion
criteria, especially after exclusion of patients older
than 80 years, but this resulted in significantly better
functional outcome. Lastly, the quick DASH score
might have been affected by previous injury or
degenerative arthritis of the same upper limb. Using
a wrist-specific score such as the Mayo wrist score or
Patient-Rated Wrist Evaluation, however, could not
reflect how the whole upper limb compensates for
the wrist function in elderly patients after distal radius fracture.
Conclusions
We advise operation with locking plate fixation for
displaced distal radius fracture with unstable fracture
pattern in active Chinese elderly patients aged 61 to
80 years. Nevertheless, further prospective study
such as a randomised controlled trial is needed to
resolve this controversy.
Acknowledgements
Special thanks to the many dedicated colleagues
from the Physiotherapy and Occupational Therapy
Departments of Tseung Kwan O Hospital.
References
1. Chung KC, Shauver MJ, Birkmeyer JD. Trends in the
United States in the treatment of distal radial fractures in
the elderly. J Bone Joint Surg Am 2009;91:1868-73. Crossref
2. Arora R, Lutz M, Deml C, Krappinger D, Haug L, Gabl M.
A prospective randomized trial comparing nonoperative
treatment with volar locking plate fixation for displaced
and unstable distal radial fractures in patients sixty-five
years of age and older. J Bone Joint Surg Am 2011;93:2146-53. Crossref
3. Egol KA, Walsh M, Romo-Cardoso S, Dorsky S, Paksima
N. Distal radial fractures in the elderly: operative compared
with nonoperative treatment. J Bone Joint Surg Am
2010;92:1851-7. Crossref
4. Lau EM, Lynn H, Woo J, Melton LJ 3rd. Areal and
volumetric bone density in Hong Kong Chinese: a
comparison with Caucasians living in the United States. Osteoporos Int 2003;14:583-8. Crossref
5. Stoker S, editor. Hong Kong 2013. Information Services Department, Hong Kong Special Administrative Region Government; 2013.
6. Lafontaine M, Hardy D, Delince P. Stability assessment of
distal radius fractures. Injury 1989;20:208-10. Crossref
7. Anzarut A, Johnson JA, Rowe BH, Lambert RG, Blitz S,
Majumdar SR. Radiologic and patient-reported functional
outcomes in an elderly cohort with conservatively treated
distal radius fractures. J Hand Surg Am 2004;29:1121-7. Crossref
8. Young BT, Rayan GM. Outcome following nonoperative
treatment of displaced distal radius fractures in low-demand
patients older than 60 years. J Hand Surg Am
2000;25:19-28. Crossref
9. Trumble TE, Schmitt SR, Vedder NB. Factors affecting
functional outcome of displaced intra-articular distal
radius fractures. J Hand Surg Am 1994;19:325-40. Crossref
10. Synn AJ, Makhni EC, Makhni MC, Rozental TD, Day
CS. Distal radius fractures in older patients: is anatomic
reduction necessary? Clin Orthop Relat Res 2009;467:1612-20. Crossref