DOI: 10.12809/hkmj144414
© Hong Kong Academy of Medicine. CC BY-NC-ND 4.0
CASE REPORT
Acquired localised hypertrichosis in a Chinese child after cast immobilisation
MW Yuen, MB, ChB;
Loretta KP Lai, MFM, FHKAM (Family Medicine);
PF Chan, MOM, FHKAM (Family Medicine);
David VK Chao, FRCGP, FHKAM (Family Medicine)
Department of Family Medicine and Primary Health Care, Kowloon East Cluster, Hospital Authority, Hong Kong
Corresponding author: Dr MW Yuen (ymw847@ha.org.hk)
Abstract
Hypertrichosis refers to excessive hair growth that is
independent of any androgen effect. Hypertrichosis
could be congenital or acquired, localised or
generalised. The phenomenon of acquired localised
hypertrichosis following cast application for a
fracture is well known to orthopaedic surgeons, but
is rarely encountered by primary care physicians.
We describe a 28-month-old Chinese boy who
had fracture of right leg as a result of an injury. He
had a cast applied by an orthopaedic surgeon as
treatment. On removal of the cast 6 weeks later, he
was noticed to have significant hair growth on his
right leg compared with the left leg. The patient
was reassessed 3 months after removal of the cast.
The hypertrichosis resolved completely with time.
This patient was one of the youngest among the
reported cases of acquired localised hypertrichosis
after cast application. We illustrate the significance
of management of post-cast–acquired localised
hypertrichosis in the primary care setting.
Introduction
Hair growth pattern in humans depends on age,
sex, and race.1 Hypertrichosis refers to excessive
hair growth that is inappropriate for a patient
after consideration of the normal variation of
an individual’s reference group.2 Hypertrichosis
is different from ‘hirsutism’, which is caused
by excessive androgen-sensitive hair growth.1
Hypertrichosis can be categorised into congenital
versus acquired and generalised versus localised,
and it may cause considerable psychological stress.3
Acquired localised hypertrichosis (ALH) following
a fracture or cast application has been reported in
different countries. In this case report, a Chinese boy
with localised hypertrichosis in the right leg after
application of a cast following right leg fracture is
described. To the best of our knowledge, this patient
represents one of the youngest reported cases.
Case report
In January 2014, a 28-month-old Chinese boy
presented to the general out-patient clinic at Tseung
Kwan O Hospital in Hong Kong with limping gait
after removal of a cast applied for right leg fracture.
During the consultation, the child was observed to
have excessive hair growth on his right leg. He had a
history of right leg fracture 6 weeks previously after
he accidentally fell from a height of 1.5 m. He had
consulted a private orthopaedic surgeon and a cast
was applied for 6 weeks. After removal of the cast,
he was noticed to have a lot of new hair growth on
his right leg. There was no increased hair growth
over the left leg or other body parts. There was no
history of systemic or topical medication use before
the onset of increased hair growth. The mother was
concerned about whether any treatment was needed
for the excessive hair growth.
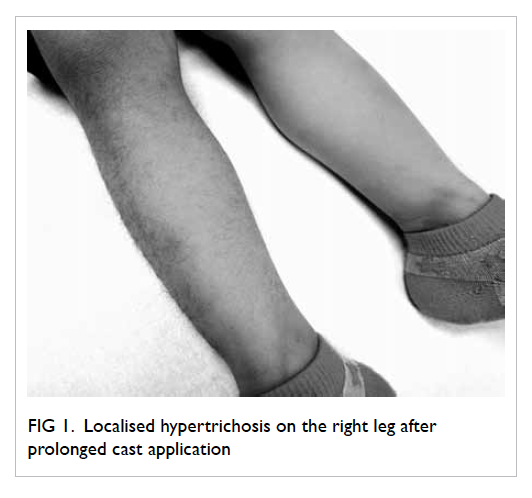
On physical examination, there was
significantly increased thick dark hair growth
over the anterior and lateral parts of the right leg
previously covered by the cast (Fig 1). There was no
other skin change. The new hair growth caused no
skin symptoms to the child. The child walked with a
mild limping gait, but there was no limb deformity,
muscle wasting, or bony tenderness.
The patient was diagnosed with ALH due to
cast application. The patient’s mother was reassured
about the benign, transient, and self-limiting nature
of the condition. His limping gait was treated with
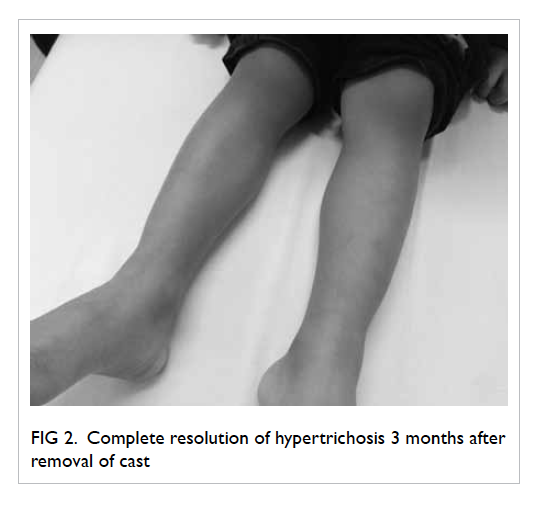
physiotherapy. He was followed up at 3 months,
when his gait had become normal and there was
spontaneous complete resolution of the localised
hypertrichosis (Fig 2).
Discussion
There are many causes of ALH such as chronic
irritation (eg skin overlying areas of thrombophlebitis
or chronic osteomyelitis), friction (eg lichen
simplex chronicus, insect bites, atopic eczema),
or inflammation (eg chemical-induced dermatitis,
ultraviolet irradiation, vaccination sites).2 It is not
uncommon to find ALH following prolonged cast or
splint application for various orthopaedic conditions.
A Turkish study involving 117 patients showed that
post-cast hypertrichosis might occur in up to one
third of patients.4 The study showed that there was
no sex predisposition, but the frequency peaked in
the adolescent age-group.4 Post-cast ALH has been
reported in paediatric and young adult patients
in various countries from 1989 to 2013, but the
prevalence in local Chinese patients is unknown.5 6 7 8 9 10 11
Complete resolution of hypertrichosis was noted at
around 3 to 9 months after removal of the cast or
splint.
One of the major mechanisms of hypertrichosis
is conversion of vellus to terminal hair. Vellus hair is
fine, non-pigmented, and produced by hair follicles
located in the dermis. Vellus hair develops on almost
all parts of the body, and its growth is not affected
by hormones. Terminal hair is thick, pigmented,
and produced by large hair follicles located in the
subcutis. Terminal hair is found on sites where hair
growth is affected by hormones, eg scalp, beard,
axillae, and pubic area.12 Vellus-to-terminal switch
on body sites that usually do not have terminal
hairs will cause hypertrichosis. The underlying
mechanism of this vellus-to-terminal switch is still
poorly understood.13
Another major mechanism of hypertrichosis
involves change in the hair growth cycle. Hair follicles
undergo lifelong cyclic transformation in three
stages: anagen, the active growth phase; catagen,
the apoptosis-driven phase; and telogen, the resting
phase followed by hair shedding.12 Hypertrichosis
results when the hair follicles stay longer than usual
in the anagen phase. Similar to vellus-to-terminal
switch, control of the hair growth cycle is still not
well understood.1
The pathogenesis of post-cast hypertrichosis
after fracture is not well-established and different
hypotheses have been postulated. Some authors
suggested that prolonged cast application provides
an occlusive, moist, and warm environment which,
together with irritation caused by friction, promotes
hair growth.11 Some authors, however, believe that
the increase in regional blood flow to the bone
following fracture provides abundant oxygen and
nutrients that prolong the anagen phase of hair
growth, resulting in transient hypertrichosis.6 This
hypothesis is supported by the speculation that
hypertrichosis has also been observed after splint
application that does not occlude the injured area,
suggesting that the fracture-healing process rather than
the cast-occlusion effect led to hypertrichosis.10
Other hypotheses on the pathogenesis of ALH
include transient cutaneous hyperaemia stimulating
the hair follicles5 and reflex sympathetic dystrophy
induced by immobilisation causing vasodilatation of
the affected area and stimulating hair growth.7
Post-cast ALH is more commonly observed in
children and young adults.4 This could be explained
by age-related changes in hair growth. With ageing,
the activity of the hair follicles declines and the hair
growth rate decreases. Since older adult patients
have a shorter anagen period of the hair growth
cycle, ALH is less frequently observed in this age-group.
Children and young adults do not have this
unfavourable effect of the ageing process on hair
growth to cancel stimulation of hair follicles after
cast application, and therefore post-cast ALH is
more commonly seen in this younger age-group.
Cases of ALH following fracture or cast
application have been described by orthopaedic
surgeons and dermatologists, but not in the
primary care setting. Nonetheless, such cases may
be encountered in primary care. Therefore, family
physicians should be aware of the diagnosis and
management of the condition and its implications
for psychosocial consequences, since hypertrichosis
may cause considerable emotional stress to patients
due to the unsightly cosmetic appearance.10 We
should address any psychological distress brought
about by hypertrichosis and reassure patients
and their parents about the benign and transient
nature of ALH after cast application. In most cases,
the abnormal hair growth will disappear within 6
months, as in this patient, and further investigation
or intervention is not indicated. If, however,
hypertrichosis causes cosmetic or psychological
problems for the patient, hair removal—for example,
by shaving or other mechanical methods—could be
considered.2
References
1. Bertolino A, Freedberg I. Hair. In: Fitzpatrick TB, Eisen AZ,
Wolff K, Freedberg IM, Austen KF, editors. Dermatology in
general medicine. New York: McGraw-Hill; 1993: 671-96.
2. Wendelin DS, Pope DN, Mallory SB. Hypertrichosis. J Am
Acad Dermatol 2003;48:161-79. Crossref
3. Vashi RA, Mancini AJ, Paller AS. Primary generalized
and localized hypertrichosis in children. Arch Dermatol
2001;137:877-84.
4. Akoglu G, Emre S, Metin A, Bozkurt M. High frequency
of hypertrichosis after cast application. Dermatology
2012;225:70-4. Crossref
5. Leung AK, Kiefer GN. Localized acquired hypertrichosis
associated with fracture and cast application. J Natl Med
Assoc 1989;81:65-7.
6. Kara A, Kanra G, Alanay Y. Localized acquired
hypertrichosis following cast application. Pediatr Dermatol
2001;18:57-9. Crossref
7. Rathi SK. Localized acquired hypertrichosis following cast
application. Indian J Dermatol Venereol Leprol 2007;73:367. Crossref
8. Leung AK, Wong AS. Localized acquired hypertrichosis
associated with the application of a splint. Case Rep Pediatr
2012;2012:592092.
9. Ma HJ, Yang Y, Ma HY, Jia CY, Li TH. Acquired localized
hypertrichosis induced by internal fixation and plaster cast
application. Ann Dermatol 2013;25:365-7. Crossref
10. Harper MC. Localized acquired hypertrichosis associated
with fractures of the arm in young females. A report of two
cases. Orthopedics 1986;9:73-4.
11. Chang CH, Cohen PR. Ipsilateral post-cast hypertrichosis
and dyshidrotic dermatitis. Arch Phys Med Rehabil
1995;76:97-100. Crossref
12. Wolff K, Johnson RA, Saavedra AP. Disorders of hair
follicles and related disorders. In: Fitzpatrick’s color atlas
and synopsis of clinical dermatology. New York: McGraw-Hill; 2013: 760-89.
13. Stenn KS, Paus R. Controls of hair follicle cycling. Physiol
Rev 2001;81:449-94.